What's On This Page?
ToggleEver heard of the term “food baby”? It has something to do with a condition called gastroparesis. You know it because it’s that overly full feeling after a big meal. Now, imagine having that feeling all the time, even without overindulging. That’s what many people with gastroparesis experience daily. It can be mild or severe, and it can vary from episode to episode.
Essentially gastroparesis means that your stomach is “paralyzed” and it can no longer squeeze or push the food in your stomach out so that it can move along your digestive tract. We are seeing more and more of this condition (which can in some cases require hospitalization) with the advent of those famous GLP-1 agonist drugs like semaglutide (Ozempic®). Read more about the connection between Ozempic and gastroparesis on WEBMED- CLICK HERE.
But not everyone with gastroparesis takes GLP-1 drugs, in fact most people don’t. So let’s talk about why you might be feeling like your full even though you haven’t eaten much. This condition is common in people with diabetes or pre-diabetes. See below for more information specifically about that.
If you often feel bloated, nauseous, or find yourself struggling with persistent fullness, it might not just be what you’re eating—it could be gastroparesis. Surprisingly, certain medications, which are otherwise meant to help us, can contribute to this condition. Today, we’ll dive into the five most popular medications that could be causing gastroparesis and how to recognize the signs of this gastrointestinal disorder.
What is Gastroparesis?
Gastroparesis is a condition characterized by delayed stomach emptying without any mechanical obstruction. In simpler terms, the stomach takes too long to empty its contents into the small intestine. Like I said above, it’s kind of ‘paralyzed’ but not in the literal sense. Regardless of the term you want to use to describe it, the delay in food transit will cause a variety of unpleasant symptoms.
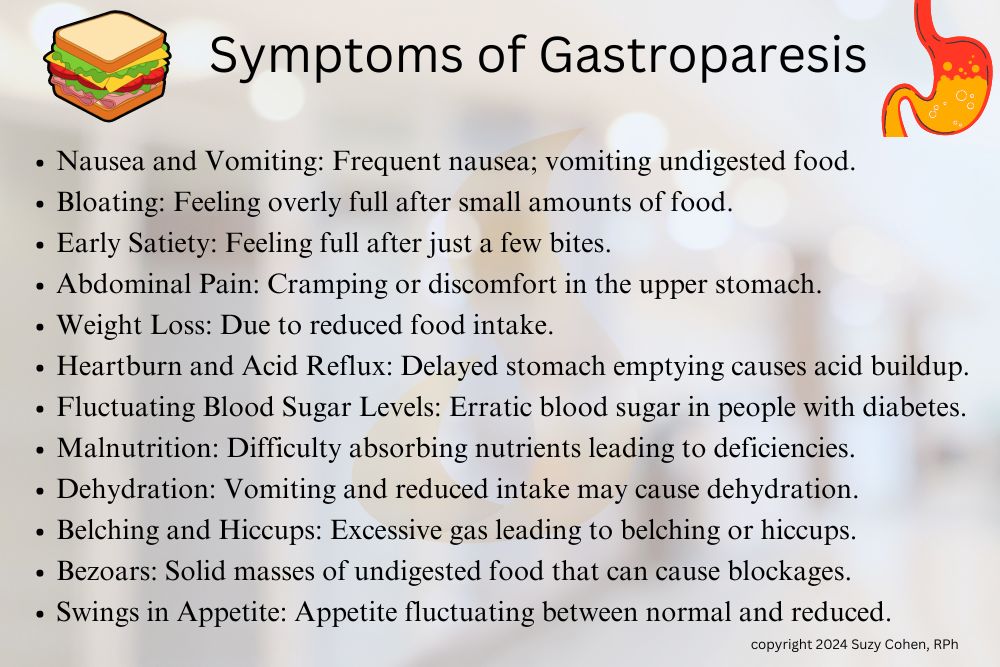
The Symptoms of Gastroparesis – How to Recognize it Before It Becomes an Emergency
Before we get into the medications, it’s essential to recognize the symptoms of gastroparesis. Here’s a quick rundown of what you might feel if your stomach isn’t emptying properly:
- Nausea and Vomiting: The feeling of needing to throw up can be frequent. In severe cases, you might actually vomit undigested food eaten hours earlier.
- Bloating: Feeling bloated, as if you’ve eaten a big meal, even if you haven’t.
Read: 7 Essential Tips to Minimize Bloating Naturally.
Read: Don’t Ignore Bloating, It Could be Ovarian Cancer. - Early Satiety: Getting full after just a few bites.
- Abdominal Pain: Cramping or pain in the upper stomach area.
- Weight Loss: Due to the reduced intake of food.
Are you on Ozempic, or thinking about taking that drug? Here’s an ARTICLE to read about nutrients that are “drug mugged.” - Heartburn and Acid Reflux: The food sitting in the stomach for longer periods can lead to acid reflux.
- Fluctuating Blood Sugar Levels: For individuals with diabetes, delayed stomach emptying can cause erratic blood sugar levels, as food is absorbed unpredictably.
- Malnutrition: Due to poor digestion and the inability to eat normally, some individuals may experience malnutrition or vitamin deficiencies, particularly in vitamins like B12 and D.
- Dehydration: Frequent vomiting and reduced food intake can lead to dehydration, especially if fluid intake is also reduced.
- Belching and Hiccups: Some people with gastroparesis may experience frequent belching or persistent hiccups due to gas buildup in the stomach.
- Bezoars: These are solid masses of undigested food that can form in the stomach, leading to blockages and worsening of other symptoms such as nausea or vomiting.
- Swings in Appetite: While early satiety is common, some people with gastroparesis might experience days of normal appetite alternating with periods of feeling completely unable to eat.
The 5 Most Common Medications that Cause Gastroparesis
Certain medications can slow down stomach emptying, leading to or worsening gastroparesis. Let’s look at five of the most common culprits:
-
Opioids
Opioids like hydrocodone (Vicodin), oxycodone (OxyContin), and morphine are commonly prescribed for pain relief. However, while they are effective at managing pain, they can also wreak havoc on your digestive system. Opioids work by binding to receptors in the brain to reduce pain sensation. Unfortunately, they also bind to receptors in the gastrointestinal tract, slowing down the movement of food through the digestive system.
- Impact on the stomach: Opioids reduce stomach motility, meaning food stays in the stomach longer, which can lead to symptoms of gastroparesis.
-
Anticholinergic Medications
These are medications that block the action of acetylcholine, a neurotransmitter that is essential for muscle contractions in the gastrointestinal tract. Examples include antihistamines like diphenhydramine (Benadryl®) used for allergies and dicyclomine (Bentyl®) for irritable bowel syndrome. There are many others. Read my other blog about how anticholinergic medications cause BLURRY VISION.
- Impact on the stomach: By blocking acetylcholine, these drugs can reduce the contractions that move food through the stomach and intestines, leading to delayed gastric emptying.
-
Tricyclic Antidepressants (TCAs)
Medications like amitriptyline (Elavil) and nortriptyline (Pamelor) are used to treat depression, anxiety, and some chronic pain conditions. While effective for these purposes, they come with a host of side effects, including the risk of causing gastroparesis.
- Impact on the stomach: TCAs have anticholinergic properties, which, as we mentioned earlier, can interfere with the muscle contractions in the gut. This slows down digestion and can lead to symptoms of gastroparesis.
-
Calcium Channel Blockers
Used primarily to treat high blood pressure, calcium channel blockers such as verapamil (Calan®) and diltiazem (Cardizem®) can also slow down the digestive process. These drugs work by relaxing the muscles in blood vessel walls, but they can also relax the smooth muscles of the gastrointestinal tract.
- Impact on the stomach: This relaxation can reduce the contractions necessary for moving food through the stomach, thus slowing gastric emptying.

-
Selective Serotonin Reuptake Inhibitors (SSRIs)
While not as commonly associated with gastroparesis as TCAs, SSRIs such as fluoxetine (Prozac®) and sertraline (Zoloft®) can still have an impact. These medications are commonly prescribed for depression and anxiety.
- Impact on the stomach: SSRIs can influence serotonin levels in the gut, which play a role in regulating digestion. Altered serotonin signaling can lead to delayed gastric emptying.
Recognizing the Signs: How to Know If Your Medication Is Causing Gastroparesis
If you’re experiencing the symptoms mentioned earlier and are on any of the above medications, it might be time to have a conversation with your healthcare provider. Here’s a checklist to help you:
- Symptom Onset: Did your symptoms start after beginning a new medication? If so, note when you started the medication and when the symptoms began.
- Symptom Pattern: Are the symptoms constant or do they seem to worsen after taking your medication?
- Medication Review: Take note of all medications you’re currently taking, including over-the-counter ones. Discuss this list with your healthcare provider.
- Medical History: Do you have a history of diabetes or other conditions that might predispose you to gastroparesis? Diabetes is a leading cause of gastroparesis but can be exacerbated by medication.
Managing Medication-Induced Gastroparesis
If you and your healthcare provider suspect that a medication is contributing to your gastroparesis, there are steps you can take:
- Medication Adjustment: Sometimes, simply adjusting the dosage can help. Other times, switching to a different medication that doesn’t have gastroparesis as a side effect might be necessary.
- Dietary Changes: Eating smaller, more frequent meals can help. Soft, easily digestible foods are less likely to exacerbate symptoms.
- Prokinetic Agents: In some cases, medications that stimulate stomach muscle contractions, such as metoclopramide (Reglan), can be used to improve gastric emptying. However, these come with their own set of potential side effects and should be used with caution.
- Alternative Therapies: Some people find relief through natural supplements and alternative therapies. Ginger, for example, is known for its stomach-soothing properties and may help with nausea. Acupuncture has also been explored as a treatment for gastroparesis, with some patients finding it helpful.
Diabetes and Gastroparesis
There is a STUDY titled “Diabetic Gastroparesis” by Adil E. Bharucha, Yogish C. Kudva, and David O. Prichard which was published in 2019 by the Endocrine Society. It examines the prevalence, causes, symptoms, diagnosis, and management of diabetic gastroparesis, highlighting how delayed gastric emptying (which occurs in both type 1 and type 2 diabetes) and anyone else with poor glycemic control, can significantly impact quality of life.
Diabetic gastroparesis is the same thing we’ve been talking about here today, where the stomach empties food too slowly. About half of those with type 1 or type 2 diabetes and poor blood sugar control may experience delayed stomach emptying. Like everything in medicine, symptoms vary, and there’s an individual response. What I’m saying is that some people may not have any symptoms, while another person could feel bloated, nauseous, or have constant indigestion.
In more severe cases, it can cause anxiety or depression. The cause of diabetic gastroparesis is usually tied to high blood sugar, nerve damage, or inflammation in the stomach muscles. Managing diabetic gastroparesis involves adjusting diet, improving nutrition, and taking medications to help the stomach work better. Severe cases may need more intense treatments, like a FEEDING TUBE or stomach stimulation! Hopefully, it doesn’t come to that for those of you reading today.

Natural Alternatives to Consider
If you’re looking for natural ways to manage or mitigate gastroparesis, there are a few options worth exploring:
- Ginger: Known for its anti-nausea properties, ginger can help soothe the stomach. You can consume it in the form of ginger tea, ginger candies, or capsules.
- Peppermint Oil: Peppermint has antispasmodic properties, which can help reduce bloating and abdominal pain. Peppermint tea or enteric-coated peppermint oil capsules are good options. Here’s my ARTICLE about how peppermint helps with irritable bowel syndrome.
- Probiotics: A healthy gut flora balance is crucial for digestion. Probiotics can help maintain this balance, potentially aiding in symptom relief.
- Magnesium: Magnesium supplements can help relax the muscles of the gastrointestinal tract and may improve symptoms. The problem is that certain forms of magnesium supplements cause diarrhea (or a laxative effect), so you have to know which kind to take. READ THIS ARTICLE to find out if you’re taking the right dosage form. The right kind of magnesium, in the right dose helps you by improving motility and easing symptoms like bloating and constipation. It may also help reduce muscle spasms and support overall nerve function, which can be beneficial in managing digestive issues. However, in some cases, too much magnesium can cause diarrhea, so it should be used with caution and under medical guidance.
- Vitamin B12: This is very important to replenish deficiencies if you have gastroparesis. Let me elaboborate right now and create it’s own section for you with more details.
Vitamin B12 and Gastroparesis
One important vitamin that can help with gastroparesis is vitamin B12. Gastroparesis can impair the body’s ability to absorb nutrients, including B12, due to delayed stomach emptying and digestive issues. Vitamin B12 is essential for nerve function, red blood cell production, and energy levels. Deficiency in B12 can lead to fatigue, neurological issues, and anemia. Because gastroparesis patients often have difficulty absorbing this vitamin, supplementation (either through diet or injections) can help maintain proper levels and support overall health.
Taking a B complex vitamin alongside B12 is beneficial because it ensures balanced levels of all B vitamins, preventing an imbalance that could occur from supplementing B12 alone. This approach helps avoid tilting the ratio of other B vitamins, like B6 or B9, into a relative deficiency, ensuring that the body maintains proper energy metabolism, nerve function, and overall health.
Summary
Gastroparesis can be a challenging condition to live with, but understanding its causes can help you take control. If you suspect that your medication is contributing to gastroparesis, don’t hesitate to reach out to your healthcare provider.
A medication review, along with lifestyle and dietary adjustments, can often provide significant relief. Remember, you have the power to take charge of your health and well-being. Whether it’s through tweaking your medications or exploring natural remedies, there are ways to manage gastroparesis and improve your quality of life.

Suzy Cohen, has been a licensed pharmacist for over 30 years and believes the best approach to chronic illness is a combination of natural medicine and conventional. She founded her own dietary supplement company specializing in custom-formulas, some of which have patents. With a special focus on functional medicine, thyroid health and drug nutrient depletion, Suzy is the author of several related books including Thyroid Healthy, Drug Muggers, Diabetes Without Drugs, and a nationally syndicated column.


