What's On This Page?
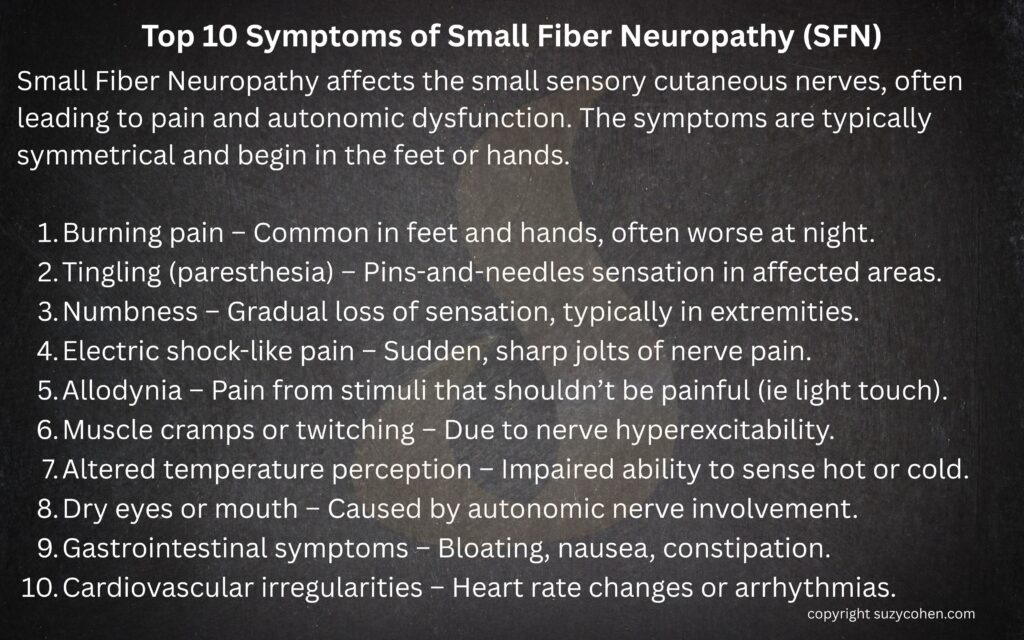
ToggleSmall Fiber Neuropathy (SFN) is a condition that affects the small sensory cutaneous nerves, leading to symptoms such as burning pain, tingling, and numbness, often in a “stocking-glove” distribution. Over the past few years, significant strides have been made in understanding, diagnosing, and treating SFN. My newest article on this topic will delve into these advancements.
While not a direct study on SFN, this one about sleep is important and I’ll explain why shortly. In the meantime, I want to remind you to use my search box to find other relevant articles where I’ve mentioned SFN and other medical conditions. I’ve archived more than 30 years of writing 🙂 Furthermore, you might want to download my ebook on Covid because I share some insights about that and SFN.
According to this NCBI STUDY, sleep is non-negotiable. Sleep deprivation impairs cognition, focus and memory drop. Mood destabilizes, immunity weakens, and chronic risks like heart disease rise. Causes include insomnia or apnea. Adults need about 7-9 hours. Fewer hours harms health for most people. You can cheat a deadline, but not biology!
Sleep matters. Poor sleep can worsen pain perception, and SFN patients often report worse symptoms (like ‘burning’ on their foot or feet) at night, disrupting sleep. It’s a two-way street: SFN can hinder sleep, and lack of sleep will almost always amplify SFN discomfort. No hard data from the study shows sleep deprivation causes SFN, but in practice, I’ve seen sleep issues aggravate neuropathic pain. How can it not?
Managing both, say, with gabapentin 300mg at bedtime is a good idea because it’s a low dose that might help with SFN as well as sleep, but not cause all the side effects of full-dose gabapentin. Ask your doctor about it, maybe it can make a difference. I’ve written about this drug in case you want to know the drug mugger effect of it, and other details: How to Properly Take Gabapentin and Restore 5 Lost Nutrients.
Just a quick word about peripheral neuropathy because it’s different from SFN.
Peripheral Neuropathy vs Small Fiber Neuropathy: What’s the Difference
Peripheral neuropathy is a pretty broad term that a lot of people use. This term actually describes damage to the nerves outside the brain and spinal cord… in the periphery and it can affect motor, sensory, or autonomic nerves, or a combination. This includes the large, heavily myelinated nerves that help with muscle strength, coordination, and vibration sense. Now, small fiber neuropathy (SFN) is a subset of peripheral neuropathy, but it targets the tiny, unmyelinated C fibers and lightly myelinated A-delta fibers.
These fibers are involved in your pain perception, temperature control, and things we don’t consciously think about, like digestion, blood pressure regulation, or sweating. It changes how you experience things when you have these two fibers damaged (the C fibers and A-delta fibers). Let me explain first what is NORMAL and HEALTHY: Let’s say you accidentally touch a hot pan. Normally, your A-delta fibers fire first – they’re your quick responders. They send that sharp, immediate “Ouch!” signal to your brain, making you yank your hand away! A moment later, your C fibers chime in with a slower, dull, burning sensation that hangs around reinforcing, “Hey, that was bad—don’t do it again.”
Now, imagine a different scenario. You touch the hot pan and not even feel the heat, or in some cases you feel it but it’s registered it way too late. That delayed or absent signal leads to burns without you realizing it, because the protective pain response is blunted or completely missing. On the flip side, if those fibers are overactive or misfiring as they often are in small fiber neuropathy, you could feel burning, tingling, or stabbing pain even when there’s no injury at all. It’s like your pain alarm system is stuck in the “on” position for no reason.
Examples of Large vs Small Fiber Neuropathy
Here’s another example: Someone with LARGE fiber neuropathy might have trouble with balance (esp in the dark) or feel like they’re “walking on cotton” because they’ve lost proprioception in their feet. In contrast, a person with SMALL fiber neuropathy could experience burning feet sensations, heat intolerance, or heart palpitations when standing up, yet still test normal on standard EMG or nerve conduction studies. That’s because those EMG/nerve conduction tests measure only LARGE fiber function and completely miss small fiber damage. Diagnosing SFN definitely requires a skin punch biopsy to count the nerve endings or specialized tests like QSART (quantitative sudomotor axon reflex testing). I’ve covered those tests before in my prior article on SFN which you can read HERE.
So while both fall under the umbrella of peripheral neuropathy, they’re quite different in how they feel, how they’re diagnosed, and which fibers are involved. It’s like comparing a faulty power line to a frayed wire in your phone charger, both are electrical issues, but they show up differently and need different solutions.
You may be wondering is “large fiber” neuropathy the same as peripheral neuropathy, and NO it’s not.
Peripheral neuropathy is actually the umbrella term, not specific to large or small fibers. It simply means there’s damage to your peripheral nervous system, which includes both large and small nerve fibers. So let me summarize it here:
- Peripheral neuropathy can involve large fibers, small fibers, or both.
- Small Fiber Neuropathy (SFN) is a specific type of peripheral neuropathy that affects only the small fibers.
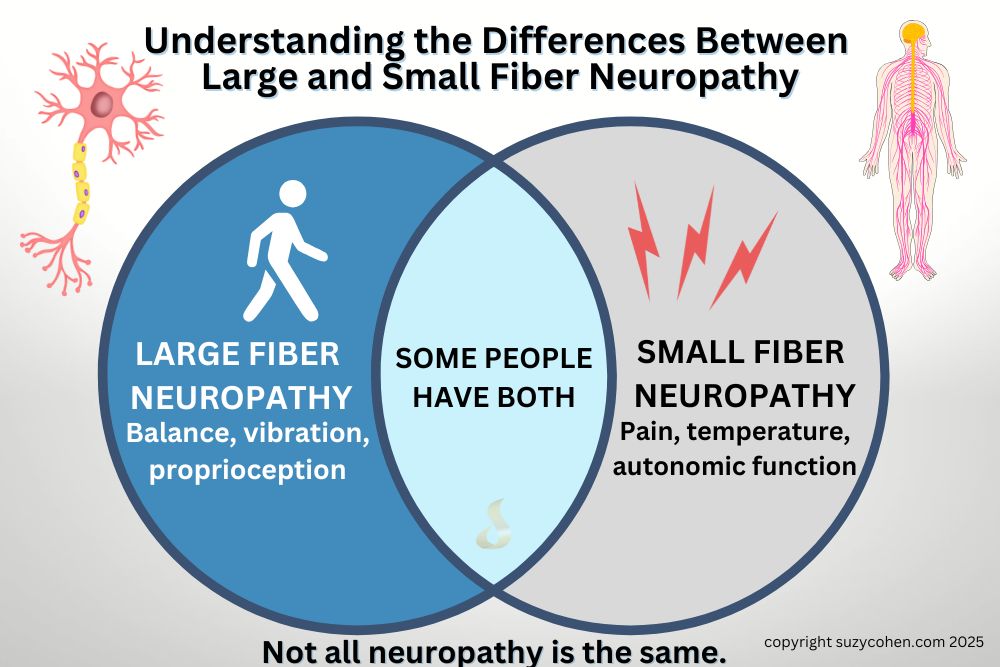
Not all neuropathy is the same. See my graphic above. Large fibers affect movement and balance. Small fibers impact pain, temperature, and even internal systems like digestion and heart rate. Some people experience both.
What is the Clinical Picture?
If someone has large fiber neuropathy, they might have:
-
- Muscle weakness
- Loss of balance (especially in the dark)
- Reduced vibration or position sense
- Abnormal nerve conduction studies
- Difficulty walking at times
If someone has small fiber neuropathy, they would complain of:
-
-
- Burning, stinging, or electric-like pain
- Heat/cold sensitivity
- Autonomic symptoms (like GI issues – see more about this below, as well as dry eyes, heart palpitations)
- Nystagmus – an eye movement disorder – READ MY ARTICLE
- Normal nerve conduction studies like an EMG
-
So SFN falls under the umbrella of peripheral neuropathy, but not all peripheral neuropathies are small fiber. Some are large fiber, and others are mixed. A neurologist can test you for these conditions and easily determine which neuropathy you have. Since this article is dedicated to SFN, I will continue. For a deeper dive, check out my earlier article – it’s one of the most-read pieces on my site and still helps thousands of readers make sense of this complex condition: Small Fiber Neuropathy Causes and Treatment.
GI Issues and Small Fiber Neuropathy
I’ve dedicated this entire section to GI issues because they will almost always be misdiagnosed if they occur! If you know me, you already know that I hate few things more than a misdiagnosis for you! I advocate for you – so I want you to know this: When small fiber neuropathy affects the autonomic nerves that control digestion, it can lead to gastrointestinal (GI) issues like nausea, bloating, constipation, diarrhea, or a mix of both.
Some people may experience gastroparesis, which is where your stomach empties too slowly, causing you to feel totally full after hardly eating! This condition can also trigger some reflux or vomiting, even the type of vomiting where it’s just “throw up in your mouth.” These symptoms happen because the nerves that help move food through the GI tract aren’t firing properly. Read this article I wrote recently on reflux and hiatal hernia: 5 Hidden Links Between Hiatal Hernia, GERD & Shortness of Breath – and Solutions.
These spasms happen when the nerves controlling your esophagus misfire, causing irregular, uncoordinated contractions of the esophageal muscles. It causes what looks and feels like a heart attack! It’s that terrifying – it causes chest pain, difficulty swallowing, or a feeling that food is “stuck” and obviously the panic that comes with all that! Some people can mistake the pain for a heart attack because it can be sharp and radiate.
In the context of small fiber neuropathy, it’s thought that dysregulated nerve signals in the esophageal wall disrupt normal peristalsis (the smooth wave-like muscle movement that pushes food downward). So in summary, esophageal spasms are one of the lesser-known but very real frustrating GI manifestations of SFN autonomic dysfunction. Somebody has to tell you because your gastroenterologist might miss that, even the best of them are NOT familiar with SFN.
Innovations in Diagnosis
Traditionally, diagnosing SFN posed challenges due to the limitations of standard nerve conduction studies, which primarily assess large nerve fibers, not small ones. That’s why a person with SFN often have a perfect EMG study! You might get dismissed even though you have full-blown nerve damage (but it’s to the small fibers, so the EMG doesn’t catch it!)
However, the advent of minimally invasive skin biopsies has revolutionized this process. It’s called a “punch biopsy” and some podiatrists can do this for you, make sure they specialize in SFN testing as there are some important guidelines to follow when testing. Anyway, by analyzing epidermal nerve fiber density, doctors can confirm SFN with greater accuracy. This technique has become a cornerstone in both diagnosing the condition and uncovering its underlying causes. PMCCleveland Clinic Journal of Medicine.
According to a study published in the Cleveland Clinic Journal of Medicine, researchers evaluated patients with small fiber neuropathy (SFN) and found it damages small nerve fibers, causing burning, tingling, or numbness, often in a stocking-glove pattern. The study reviewed cases linked to diabetes, autoimmune diseases, or unknown causes, common in older adults. Small fiber neuropathy is part of Sjögren’s Syndrome and many people don’t know this. This PAPER talks about it as one of the more common peripheral nervous system issues linked to Sjögren’s. Basically, it shows up as stuff like burning, numbness, or weird pain—usually in the hands and feet.
Pain was sharp or dull, worsening at night. Researchers found skin biopsy confirmed SFN by showing reduced nerve fiber density. Treatment with drugs like gabapentin helped some, while alpha-lipoic acid or yoga offered mild relief. Progression was slow for most, but variable.
A Better Way to Diagnose? Corneal Confocal Microscopy (CCM)
I really appreciate the following research because it doesn’t involve needles, scissors or lidocaine! If you’ve had a punch biopsy, then CCM or Corneal confocal microscopy sounds GREAT!!!
It’s a non-invasive imaging technique that allows for the visualization of corneal nerve fibers. This valuable tool can be used to detect SFN by assessing nerve fiber density and morphology in the cornea. Studies have demonstrated that CCM can identify small nerve fiber loss in various neuropathic conditions, including diabetic neuropathy and idiopathic SFN. A review published in Scientific Reports highlighted CCM’s ability to detect nerve fiber damage and its potential to monitor disease progression and response to treatment.
Because it’s fast and non-invasive, CCM offers a really promising approach for early detection (and monitoring) – I hope it takes over for the punch biopsy method! More people would opt in for the test and find out if they have this condition, which would improve outcomes and comfort for many.
Unraveling New Causes & Treatments – Let’s Talk “Sodium Channels”
Aside from Covid and Covid jabs being a risk factor for SFN, there’s more. Recent research has shed light on genetic mutations as potential culprits in SFN development. Mutations in sodium channel genes, particularly SCN9A and SCN10A, have been implicated in the pathophysiology of SFN. These discoveries have opened new avenues for understanding the condition and developing targeted therapies. But what exactly is a sodium channel? Doctors don’t talk about it much, and when you research online, it gets complicated. Let me break it down first, and then after that, I’ll share the studies that have come out in recent years.
SCN9A, SCN10A, and SCN11A: How They Affect Nerve Pain and Sensation
Your nerves work like electrical wires, sending messages to your brain to help you feel things like heat, cold, and pain. To do this, they rely on tiny “gates” called sodium channels, which allow charged particles (sodium ions abbreviated as Na⁺) to flow in and out of nerve cells. This movement generates electrical signals that tell your brain what’s happening in your body.
The SCN9A, SCN10A, and SCN11A genes provide the instructions for making these sodium channels, specifically Nav1.7, Nav1.8, and Nav1.9. These channels are especially important in sensory nerves, which detect PAIN and TEMPERATURE.
Here’s where things get tricky:
- If these channels stay open too long or open too easily, your nerves send too many pain signals—causing burning, tingling, or stabbing pain (like in small fiber neuropathy, SFN).
- If these channels don’t open enough, your nerves can’t send pain signals properly, leading to numbness or insensitivity to pain, which sounds good, but can actually be dangerous because you wouldn’t feel injuries. Remember my example above where the heat isn’t felt or there is a delay? It’s like a dimmer switch on your sensations!
For example:
- SCN9A (Nav1.7) mutations can cause excess pain (neuropathy) or, in some cases, no pain at all (congenital insensitivity to pain).
- SCN10A (Nav1.8) is involved in how long pain signals last. Mutations here have been linked to chronic nerve pain.
- SCN11A (Nav1.9) affects how easily nerve cells get excited. If it’s overactive, you might feel constant pain even without an injury.
Think of it like a dimmer switch for pain: If it’s stuck on high, you feel too much pain. If it’s stuck low or off, you don’t feel enough.
Scientists are studying these genes to develop new treatments, like sodium channel blockers, which could help turn the “switch” back to normal for people with nerve pain conditions like SFN. Are you curious if there are natural or prescription “sodium channel blockers”? The answer is yes. 👉 Take a few more minutes to read my other article entitled, Soothing Small Fiber Neuropathy: 11 Natural and Prescription Sodium Channel Blockers.
These genes control how your nerves process pain, and when they don’t work right, it can lead to chronic pain or numbness. Understanding them is helping doctors find better treatments for conditions like small fiber neuropathy.
Studies Regarding Small Fiber Neuropathy (SFN) and Sodium Channels
In this PAPER entitled, Expanding the Genetic Causes of Small-Fiber Neuropathy: SCN genes and beyond, mutations were found in people who had SFN. This isn’t a surprise but many (if not most) cases are linked to metabolic or immunological factors, and a significant number of cases remain idiopathic. The genetic mutations were discovered in sodium channel genes like SCN9A, SCN10A, and SCN11A. Having a gene SNP in these genes can cause pain signal amplification.
According to a published in Journal of Neurology, Neurosurgery & Psychiatry, researchers evaluated 248 patients with small fiber neuropathy (SFN) and found that 12 of them, about 5%, had mutations in the SCN9A gene.
These sodium channel changes make your nerves overactive, causing the burning and tingling SFN is known for. Most patients had no other obvious cause, and the mutations were confirmed with genetic testing and nerve studies. It’s a small group, but it shows SCN9A could be a key player in some SFN cases, pointing to possible future treatments.
Treatments – Natural and Rx for Sodium Channel Issues
Let’s start on the natural side 🌿. If you’ve got SCN9A mutations ramping up nerve pain, some plant-based compounds might offer gentle relief. Think turmeric, chili peppers, and a few antioxidant allies—nothing magic, but possibly enough to take the edge off.
The science is still evolving (we’re talking lab dishes more than human trials), but some of these natural options show intriguing potential to calm overactive sodium channels. Curious what they are?
👉 I put together a full list of natural and prescription sodium channel blockers RIGHT HERE.
Let’s talk about the FDA-approved drugs. Sodium channel blockers are the big players here. Lidocaine, available as a patch at any pharmacy or available by injection, actually clamps down on sodium channels, including Nav1.7 from SCN9A, cutting pain signals. I talk about this in my other article, Soothing Small Fiber Neuropathy: 11 Natural and Prescription Sodium Channel Blockers.
It’s approved for post-herpetic neuralgia but used off-label for SFN. Mexiletine, an oral antiarrhythmic, does the same trick and shows promise in SCN9A-related SFN pain, though it’s not officially tagged for neuropathy. Anticonvulsants like carbamazepine and lacosamide also target sodium channels. Lacosamide’s newer and has buzz for SFN linked to SCN9A mutations—small studies say it helps pain without knocking you out.
These are prescription-only, and side effects like dizziness or heart rhythm quirks need watching.
The catch? Natural stuff lacks solid SCN9A-specific data, and even FDA drugs aren’t tailored just for SFN – they’re broad-spectrum. If SCN9A’s your culprit, talk to your doc about genetic testing and maybe as a l lacosamide (Vimpat® — but it has cardiac side effects so it’s not my favorite) or mexiletine, an anti-arrhythmic drug. For now, science is still connecting the dots on those two.
Emerging Treatments and Therapies
The therapeutic landscape for SFN has expanded with several promising interventions:
- Sodium Channel Blockers: The identification of sodium channel gene mutations has led to the exploration of sodium channel blockers as potential treatments. Clinical trials are underway to assess their efficacy in alleviating neuropathic pain associated with SFN. ScienceDirect
- Scrambler Therapy: This FDA-approved form of cutaneous electrostimulation offers neuromodulation of pain and has shown effectiveness in some SFN patients. OUP Academic
- Biopsychosocial Rehabilitation: Recognizing the multifaceted nature of SFN, personalized rehabilitation approaches that address both physical and psychological aspects are under investigation. Early studies suggest improvements in quality of life and reductions in disability. Frontiers
- Supplements: Certain supplements, such as acetyl-L-carnitine, alpha-lipoic acid, B VITAMINS, and capsaicin, have been explored for nerve pain relief in neuropathy. While some research supports their benefits, more studies are needed to fully understand their effects. Consultation with a healthcare professional is essential before starting any supplement. Verywell Health
Oleuropein and Small Fiber Neuropathy
Oleuropein, a polyphenolic compound predominantly found in olive leaves and olive oil, has recently garnered attention for its potential neuroprotective and anti-inflammatory properties, which may be helpful for SNF patients. Animal studies have shown that oleuropein can alleviate neuropathic pain behaviors and probably reduce nerve damage markers.
For instance, research published in the Journal of Food Biochemistry suggests that regular intake of oleuropein correlates with decreased risks of neural disorders, including Alzheimer’s, Parkinson’s, strokes, depression, anxiety, and epilepsy. In short, regular intake of oleuropein, a powerful compound in olive oil and olive leaves and dietary supplements, may help reduce the risk of those neurological conditions I just mentioned.
What’s even more fascinating is that oleuropein can help restore healthy levels of hydrogen sulfide (H₂S) – a signaling molecule, in the body that’s often depleted in people with nerve damage. Since H₂S plays a key role in nerve function and pain signaling, this could make oleuropein a promising natural remedy for easing symptoms of small fiber neuropathy. I love simple and natural options. They don’t hurt, and they might help!
You can read more in my other blog, 6 Critical Ways that Olive Oil Helps Painful Neuropathy – Even Small Fiber!
The Impact of COVID-19
The COVID-19 pandemic has introduced new considerations for SFN. Emerging evidence suggests that some people develop SFN following a COVID-19 infection or vaccination. Preliminary studies indicate that Intravenous Immunoglobulin (IVIG) therapy may be effective in treating post-COVID SFN, highlighting the need for further research in this area.
According to a 2024 study published in Neurology, researchers evaluated 102 patients with small fiber neuropathy (SFN) and found that 33% had autoimmune conditions—like Sjögren’s or lupus—linked to their nerve damage. They tested blood for antibodies and used skin biopsies to confirm SFN, spotting immune system overactivity in many cases. The big find? Treating the autoimmune issue with stuff like IV immunoglobulin (IVIG) or steroids improved pain and nerve function in some, especially those with specific antibodies. It suggests SFN isn’t always a mystery, sometimes it’s your immune system gone rogue.
So this is the latest scoop on everything that I could find related to small fiber neuropathy. There are sleep issues, sodium channel glitches, and the possibility of rogue immune function all playing a part.
But SFN’s a tricky beast, and there’s more to unpack. Do you want the whole story on how it’s different from other neuropathies, plus some practical tips I’ve shared before? Check out my earlier blog – it’s one of my most popular blogs: Small Fiber Neuropathy: It’s Different. It’s a deep dive that pairs perfectly with this new info, go give it a read!
Conclusion
The past few years have marked significant progress in the realm of Small Fiber Neuropathy. Advancements in diagnostic techniques, a deeper understanding of genetic factors, and the development of novel therapies offer hope to those affected by this condition. As research continues to evolve, it is imperative for you to consult with healthcare professionals to determine the most appropriate and personalized treatment strategies.

Suzy Cohen, has been a licensed pharmacist for over 30 years and believes the best approach to chronic illness is a combination of natural medicine and conventional. She founded her own dietary supplement company specializing in custom-formulas, some of which have patents. With a special focus on functional medicine, thyroid health and drug nutrient depletion, Suzy is the author of several related books including Thyroid Healthy, Drug Muggers, Diabetes Without Drugs, and a nationally syndicated column.