What's On This Page?
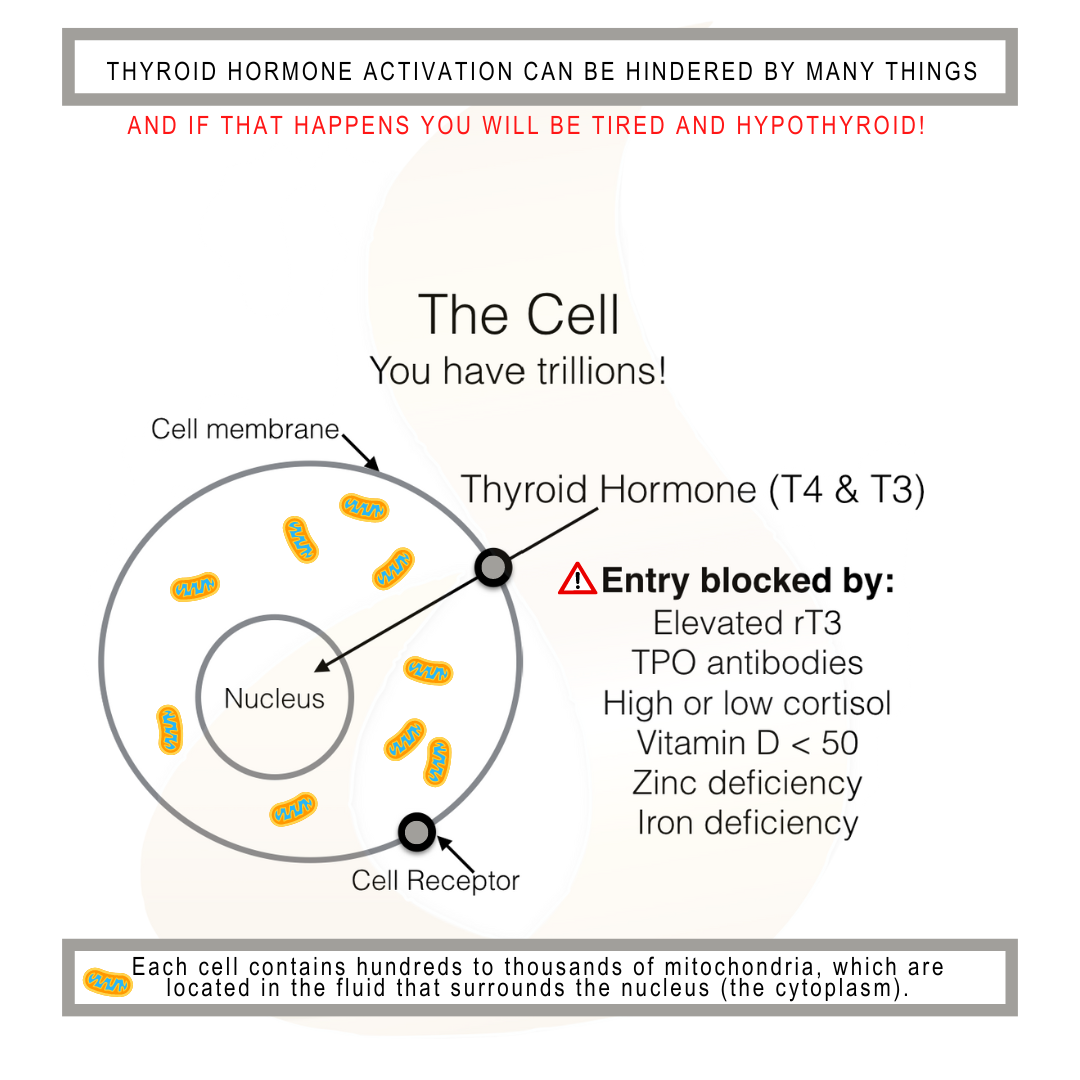
ToggleYour thyroid gland sits at the base of your throat and is approximately 1.5 to 2 inches wide. Under normal circumstances, it produces thyroid hormone that gets distributed throughout your body. Every cell in your body has a receptor for thyroid hormone which most people don’t realize.
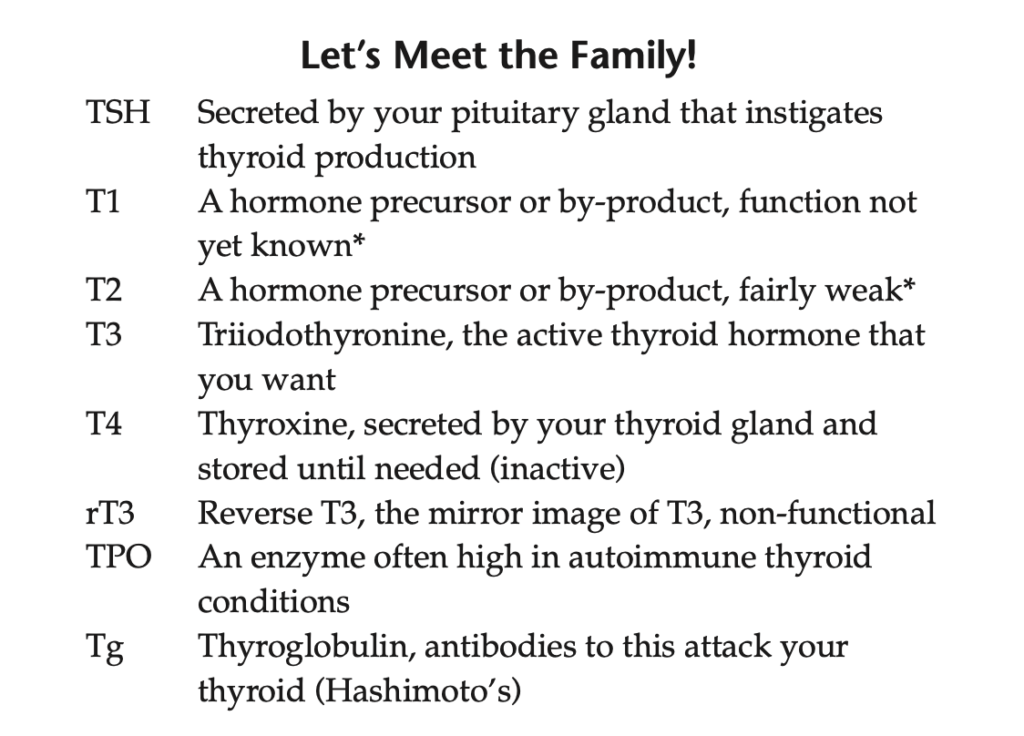
So if you’ve had your thyroid gland surgically removed, you should still be restoring thyroid hormone with prescription medications such as Nature-Throid, Armour Thyroid, Synthroid, or something along those lines. Thyroid hormone isn’t just one hormone, it is borne from your thyroid gland as T4 known as thyroxine.
This has to undergo several chemical reactions. If you have genetic polymorphisms in your genes, and most people do, then you may have difficulty making the biologically active form of thyroid hormone dubbed T3 for triiodothyronine.
This is what your periphery requires, what your tissues and cells need in order for you to feel well. Certain vitamins and hormones are required for the activation of T4 to T3. Let’s dive into that because your blood tests may look “normal” and yet, you may still feel weak, tired, foggy, overweight, and cold.
It could be in the conversion process of T4 going to T3. The numbers (3 in T3 and 4 in T4) refer to the number of iodine molecules attached to the amino acid tyrosine.
Just because your thyroid gland secretes T4 and your lab value for “total T4” is normal doesn’t mean you’re well and healthy. In order for T4 (inactive) to become T3 (active), it has to be converted and the conversion takes place primarily in your liver, as well as your kidneys, brain, and intestines.
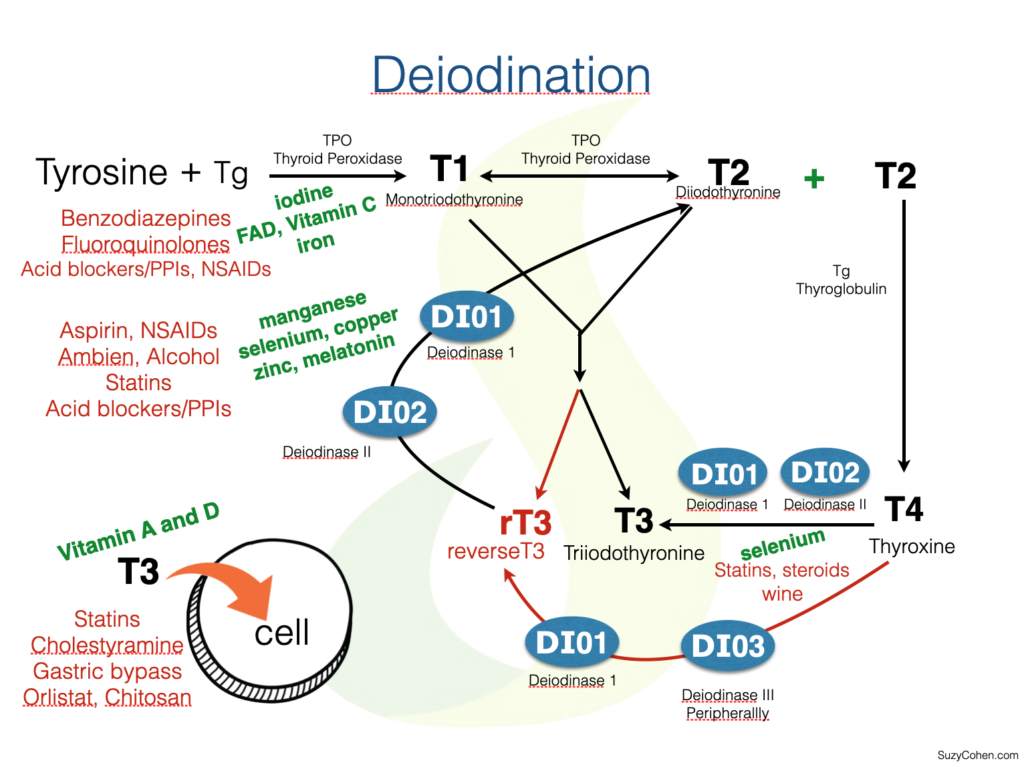
So step one is to be sure that your liver enzymes are in the normal reference range and that you’re not abusing your liver with too much alcohol, cigarettes, or pesticides. Specific deiodinase enzymes are necessary for the activation and utilization of the thyroid.
These deiodinase enzymes clip off iodine from T4, to form T3. That’s how thyroid hormone gets activated! It’s the T3 that helps you feel most active, happy, and warm. T3 is also a fat burner, and it helps with hair growth and cardiac function.
Two Facts About Thyroid Hormone:
1. More than ninety percent of the thyroid hormone produced is actually T4 (inactive storage form) and seven percent is T3 (the active form). That may sound bad, but it’s not because T3 is the gas pedal here, and if you push that too hard (ie strive to make 10% or 20% instead of 7% for example), you’ll feel wired, anxious, sweaty, and sleepless. These symptoms occur in people who take too much T3 hormone in the form of medication or supplements.
2. The other thing is that T4 is needed for proper riboflavin function and ACTIVATION.
If you are T4 deficient, you may not be able to create riboflavin mononucleotide and flavin adenine dinucleotide (FAD) which are two biologically active coenzyme forms of the B vitamin.
Blood Work.
When your blood work in your lab shows T4 levels in the normal range, it’s not a good reflection of how you feel. T4 doesn’t technically work, although it is needed in the body. But it is a pro-hormone. It has to become activated by dropping one of those four iodine atoms in a biochemical process called “deiodination.” Nutrients such as B vitamins and minerals are needed for you to have adequate active thyroid hormone. You need selenium for the deiodinase enzymes to work.
Thyroid hormones can be metabolized in peripheral tissue by deiodination, deamination, conjugation, and decarboxylation enzyme reactions, but again, I’m not going to bog us down with these details because today I want to offer solutions, not too much science. Here are a few things that your body could use to convert the T4 to T3 more.
Your Gut Health.
Some of your thyroid hormone (about 20 – 25 percent) gets activated to form T3 in your gastrointestinal tract, compliments of friendly microorganisms. So step two is to make sure that you have enough probiotics available to activate your thyroid hormone in the gut.
People with poor GI status, either Crohn’s, IBS, diarrhea, or other conditions develop hypothyroidism secondary to the lack of healthy microflora.
TSH or Thyroid Stimulating Hormone.
Let’s back up for a moment because I want to talk about TSH, the most common lab work drawn. It has such limited use, yet it is the gold standard test for thyroid function. It is fine to draw as part of a full thyroid panel, but drawing it by itself is not super useful. Other lab evaluations are more useful such as T4 and T3, and even TPO antibodies if Hashimoto’s is suspected. There are others too.
(Excerpt Chapter 3 of Thyroid Healthy book, Suzy Cohen, RPh)
TSH It goes by “Thyrotropin” sometimes produced in the pituitary gland in your brain. It is sometimes referred to as a “brain” hormone but to be technically correct it’s really from your pituitary which is a gland, and different from your brain. Anyway, TSH is a loudspeaker that shouts, “Hey thyroid gland, can you start making more thyroid hormone?” and for most of you, your gland happily responds, “Yes!” and makes T4 (thyroxine) for you. The T4 gets secreted and feeds your brain first, then your peripheral tissues. Your brain always gets fed first.
Now, as I’ve explained, T4 is inactive after it’s birthed from your thyroid gland. If your TSH is high, you can assume your peripheral tissue thyroid is low because your brain always gets first dibs on thyroid hormone.
Now, if your TSH is normal, your test is pretty much irrelevant because your cells may still be starving even while your brain is getting fed. This is the rationale for taking a complete thyroid panel which measures other thyroid biomarkers.
If there’s one thing I want you to learn today it’s this: The TSH hormone is fine if you’re evaluating brain levels of thyroid hormone, but it does not speak about peripheral tissue (intracellular) levels of thyroid.
Put it this way – your TSH level is blind to what’s going on inside your cell and so TSH is not useful at finding people who are failing to convert T4 to T3. If that’s you, and it’s most people, then you will fall through the racks and continue to lose your hair, feel tired, weak and cold, and experience weight gain, or maybe a stubborn ability to lose weight. Adrenal dysfunction is almost always implicated in thyroid disorders, adding one more reason to feel tired, possibly depressed, dizzy and short of breath.
What about Autoimmune Hashimoto’s Thyroiditis?
When your thyroid gland makes thyroxine in response to TSH shouting at it, the production happens with the help of this TPO enzyme. TPO is not a bad thing, it’s a great thing but you often hear TPO cast in a negative light. The reason is that antibodies (the ‘soldiers’ in your body) can attack the TPO enzyme, and that’s the bad part. If your body launches this self-attack upon its own enzyme TPO, you will then be diagnosed with an autoimmune type of thyroid condition.
When doctors evaluate your blood levels of antibodies against TPO enzyme, they are trying to discover if you have Hashimoto’s or Hashi for short. People with Hashi have elevated antibodies to TPO.
Deiodinase Enzymes.
You have two different enzymes with this name, D1, and D2. If either one of these is hindered you will not activate thyroid hormone very well in your muscle cells or periphery. It doesn’t matter how much T4 you make, you have to activate it in your other cells all throughout your body- outside of the thyroid gland!
So D1 and D2 are the enzymatic pathways that truly help to give you energy and make you feel great. They convert that T4 from your thyroid gland into T3 all over your body.
Deiodinase-1 (DIO1 or abbreviated as D1)
Deiodinase 1 helps with the activation of thyroid hormone in the body, but it is less active than D2 (see below). This protein is found primarily in your liver and kidneys, but also in the thyroid and adrenal glands and your pituitary gland.
Just like D2, the D1 enzyme clips off an iodine atom from T4 to induce the formation of T3. D1 helps you make about 5 mcg of T3 each day. The D1 enzyme can’t work without sufficient selenium or cysteine.
Deiodinase-2 (DIO2 or D2)
When DIO2 or D2 is low, decreased conversion of T4 to its active form T3 occurs. Peripheral tissues starve. D2 enzyme is responsible for most of the T3 activation and it generates about 20 micrograms each day which is approximately 2/3 of normal daily T3 production. Compare that to your D1 enzyme which helps you make 5 mcg of T3 each day.
D2 is doing its business and activating your thyroid hormone all over your body, not just your thyroid. It is working in your fat cells (brown fat), central nervous system, and muscles. If you have a genetic SNP that slows down this enzyme, you will not respond well to traditional T4 drugs like Levothyroxine.
In this specific case, if you have an SNP in your D2 pathway you would be a person who would do better with a combination of T4/T3 therapy such as Armour Thyroid, Nature-Throid, NP Thyroid, and WP Thyroid. The D2 enzyme will only work if it has its cofactors available which are selenium and cysteine to create selenocysteine.
As an aside, there is a protein you can research on your own called Phosphodiesterase 8B that breaks down cyclic AMP (cAMP) and this is one of the major signaling regulators indoor thyroid gland, significantly increasing TSH production.
What is the treatment for thyroid disorder?
Treatment for a thyroid disorder varies on the specific disorder you have. This is why there are so many drug treatments, vitamins, herbal remedies, and lifestyle factors. There isn’t one single approach that works. To give you a few examples in the most simplistic form, take a look at this:
Hashimoto’s or Graves’ disease treatments require medications or supplements to calm down the body’s immune attack. Medications may be required to either raise or lower thyroid hormone depending on which direction it was swinging.
Compare that to someone who has hypothyroidism because they are iodine deficient and perhaps eat poorly. You can’t make thyroid hormone without iodine so restoring that would be crucial, as well as a good probiotic. Now compare that to someone who is unable to convert their T4 to T3 and simply needs some ashwagandha, B vitamins, and a smidge more Vitamin D!
Physicians have their hands full trying to figure out what to do with each person who has thyroid disease because it presents differently and the treatment is different. Trial and error and experimentation are required, and so are routine blood draws to gauge where you’re at with all these hormones.
I made a PowerPoint slide for a presentation for physicians once that shows how the deiodinase enzymes work, and what happens peripherally with the activation of thyroid hormone. I’m posting it here for you to see how complicated it can really be and where things can go wrong. The medications shown in the red-colored font are the drugs that interfere in that specific section of the pathway. If you or any physician likes this slide and wants more to help you see where medications ‘create an SNP’ you can purchase it HERE. It is truly invaluable if you like genetic SNPs and want to figure out where your patients are creating an SNP (by taking a medication).
Summary of thyroid disorder Treatment Options
You can optimize the conversion and activation of thyroid hormone levels today easily. With your practitioner(s) help, you can use thyroid medications and/or dietary supplements.
Please discuss these options with your physician because not everything listed here is right for each of you. Furthermore, no one needs to be taking ALL of these either, these are simply ideas. Your specific thyroid condition, allergy profile, medical history, and genetics will dictate which of these -if any- are right for you.
Probiotics – They help convert T4 to T3 in the gastrointestinal tract and support immune function.
Selenium – This mineral helps manage TPO enzymes, often reducing autoimmune problems, while also supporting the D1 and D2 enzymes which activate T3.
Vitamin D – Low levels of vitamin D (below 40) correlate with a higher risk of autoimmune thyroid disorders.
Ashwagandha – Can boost thyroid hormone production, both T4 by about 20% and T3 by 42%. The study is HERE.
Thyroid Hormone – Many medications exist in this category and this help restore lost hormone if you’ve had a thyroidectomy or if your gland is not producing enough.
Adrenal Supplements – Most people with thyroid dysfunction require adrenal support because they need to regulate the cortisol hormone better.
ZINC – Zinc deficiencies can lead to insufficient levels of T4 and T3. Also, zinc is needed for the deiodinase enzymes.
Tyrosine – Required for synthesis of thyroid hormone, this amino acid binds the iodine molecules to form T4 in the human body. Tyrosine has other benefits too.
IODINE – Required for the synthesis of thyroid hormone, there are receptors on every cell for iodine. Iodine is a strong antioxidant and has many profound health benefits for the breast and prostate.
Guggul – Guggul extracts seem to help by increasing iodine uptake in the thyroid gland. Iodine is needed to create thyroid hormone.
B vitamins – B9, B12 and B6 – B vitamins are necessary for healthy nerve function and cognition. Furthermore, deficiencies in B vitamins, especially B12 are associated with autoimmune thyroid disorders.
I hope you’ve enjoyed this article and that it has given you a new perspective on treatment options for your condition. There are many other topics that I didn’t cover in this, as well as more treatment options for you. CLICK HERE if you’re interested in reading a copy of my book Thyroid Healthy – Lose Weight, Look Beautiful and Live the Life You Imagine.
Information is power. Now you have that power. Feel free to pass it along to someone else who is struggling. If you’d like a FREE ebook on the topic, CLICK HERE.

Suzy Cohen, has been a licensed pharmacist for over 30 years and believes the best approach to chronic illness is a combination of natural medicine and conventional. She founded her own dietary supplement company specializing in custom-formulas, some of which have patents. With a special focus on functional medicine, thyroid health and drug nutrient depletion, Suzy is the author of several related books including Thyroid Healthy, Drug Muggers, Diabetes Without Drugs, and a nationally syndicated column.