What's On This Page?
ToggleIn the past month, I’ve talked to 4 different people who have either had a sinus surgery or had an actual sinus fungal ball! Yesterday at Zumba, my friend Jeanne told me about her sister’s plaguing symptoms and all I could think of is that I wish I could point her to an article for help! She clearly has a sinus fungal ball (SFB) and I fear it’s getting misdiagnosed according to Jeanne, she is suffering so much. She’s not the only one either! Today, I’m writing about it because a good article needs to be published about it because what you find on Medscape and other generic medical sites is not too helpful or detailed. So I hope that by the end of this blog, I will have helped you, or someone you care for. I’ve outlined 4 simple case studies which I talk about later on.
These sinus fungal balls are occurring at rapid, alarming rates due to this being a new long-term complication of having COVID-19. One confounding symptom is a foul odor that no one else smells, or the inability to smell. Those two symptoms are common with the Omicron variant but it confounds the diagnosis because those are common symptoms of a sinus fungal ball too.
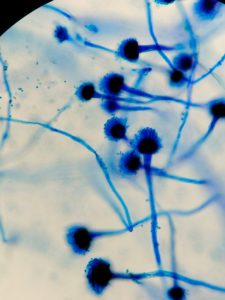
Fun fact, the aspergillus organism that usually is found in a sinus fungal ball was first discovered in 1729 by Pier Pier Antonio Micheli, an Italian priest and biologist. According to this PAPER the shape of the fungus he found looked like similar to a little hand-held device he used to sprinkle holy water during church services called an aspergillum.
This is an interesting topic, and one that is worthy of discussion because this fungal ball can wreak great havoc in your life if you do not know what it is, and you do not receive treatment in time. Many people taking migraine medicines, or experiencing persistent daily headaches could benefit from today’s article as well.
It can certainly cause headaches, that’s one of the main symptoms. I wish I knew more about it when I wrote my book, Headache Free book because I offered many solutions for various headaches, but I did not even mention a “sinus fungal ball” and that’s because I did not know about it until recently. For that I am sorry. I could have helped so many people if I knew about it then. Not many people do, it’s considered rare.
Having a fungus in your head will cause a headache! A bad one too… and it can move around in seconds. It does not usually impact the back of the head though. A fungus may also cause weird visual symptoms due to it affecting the optic nerve. Here’s one of many SCIENTIFIC PAPERS published online that explains the clinical characteristics and reasons for visual impairment.
Many people who have had C*V1D -!9 have temporarily lost their sense of smell, or have other issues with scents. You may be told you have “phantosmia” which is actually a neurological problem… it is an olfactory hallucination of sorts and it’s not the correct diagnosis for someone with a fungal ball! But with a sinus fungal ball, you will often experience distorted or “bad smells” or like something is rotting, or burning —that no one else can smell! The difference is that a SFB is not neurological in nature, whereas phantosmia is. This is a very important distinction because anti-seizure meds will only treat phantosmia, these drugs do not eliminate or help the bad smell associated with a SFB.
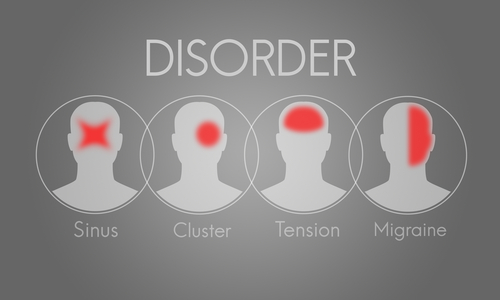
Oftentimes, people with a SFB are told they have an atypical migraine and migraine meds are ordered, but they will not cure the headache. Take a look at my very simple graphic to see the area of pain most often affected if you have a migraine vs. tension vs. sinus vs. cluster headache.
You can see how easy it is to be misdiagnosed because the areas of pain overlap! And the truth is most docs aren’t thinking sinus fungal ball when you say you have chronic headaches! But Aspergillus fumigatus is documented to produce a spore called “Conidia” which can increase Interleukin-8 (IL-8) and other cytokines leading to NF-κB activation — meaning PAIN! Read THIS ARTICLE.
Do you know what reduces conidia? At least in food… N-acetyl cysteine (NAC) and also its metabolite L-cysteine. This is found in some immune-boosting supplements, and if you recall I was very upset last year when Amazon banned this supplement. It is still available for purchase, but not on Amazon.
That specific type of sinus headache is honestly completely off the radar for even the most caring, attentive physicians, especially if you do not suffer from sinus issues due to a blocked cavity. And some of you reading this might think that is odd, but it’s not, you can definitely have posterior rhinorrhea with a SFB, read this PAPER and there are many others. In my case studies (at the end of this article, Spencer had this due to a complete blockage, and therefore did not have any typical sinus/nasal discharge, leading to years wasted in getting properly diagnosed.) I found this ARTICLE from 2020 published in the American Journal of Otolaryngology extraordinary in terms of its explanation.
Only a trained, experienced ENT will spot it, and they will see it fast. Opacity on the MRI is one clue. My point is to explain to you why seeing an ENT physician for headaches that are unresponsive to conventional medications is of the utmost importance. Sometimes a person is misdiagnosed with a neurological condition, instead of what they truly have – a sinus fungal ball! The former is difficult to treat, whereas the latter is easily treatable and curable through surgery with a proficient ENT. There is definitely hope no matter how long you have had a SFB.
Complications and Mitigating Factors of SFB
I might add that a fungus can grow in your sinus cavity for many years without you knowing it! It isn’t a sudden medical emergency. You can walk around with this condition for years. It can begin shortly after you’ve had a root canal, or tooth extraction or dental (mercury) removal. All of those procedures increase your risk for SFB.
Once you have a sinus fungal ball, you might expect that it cause sinus problems. Certainly, it can, but it doesn’t have to. It may or may not cause a stuffy nose, or runny nose as you might assume. I know one person named Spencer (see below for the graphic pictures), whose sinus was blocked entirely on the left side, as indicated by complete opacification on the MRI, but he never had a runny nose!
The growth of a “fungal ball” goes under the radar for many years in people, causing symptoms up in the head that often get diagnosed as something else, usually headaches or migraines, however, there is NO aura, a very important distinguishing feature of migraines. The ‘bad smell’ is one tell-tale sign that I have already mentioned. Another is the constant clearing of the throat due to constant drainage of the sinuses down the back of the throat. It can cause a chronic red, sore throat.
A SFB can be associated with LPR or silent reflux requiring you to take Pepcid each day. I tell you this because if you have LPR, you may want to have your sinuses checked with a CT scan and see your ENT.
Today, I have a dual focus on my article. First, I’d like to help you determine if you have a sinus fungal ball because it could look like so many other diseases, and second, I’d like to point you in the right direction in order to get treatment and relief.
Since symptoms are broad in nature (ie headaches for example), be careful not to assume you have a sinus fungal ball when you really don’t. A qualified ENT (Ear, Nose and Throat) physician will be of critical importance in determining the true diagnosis for you.
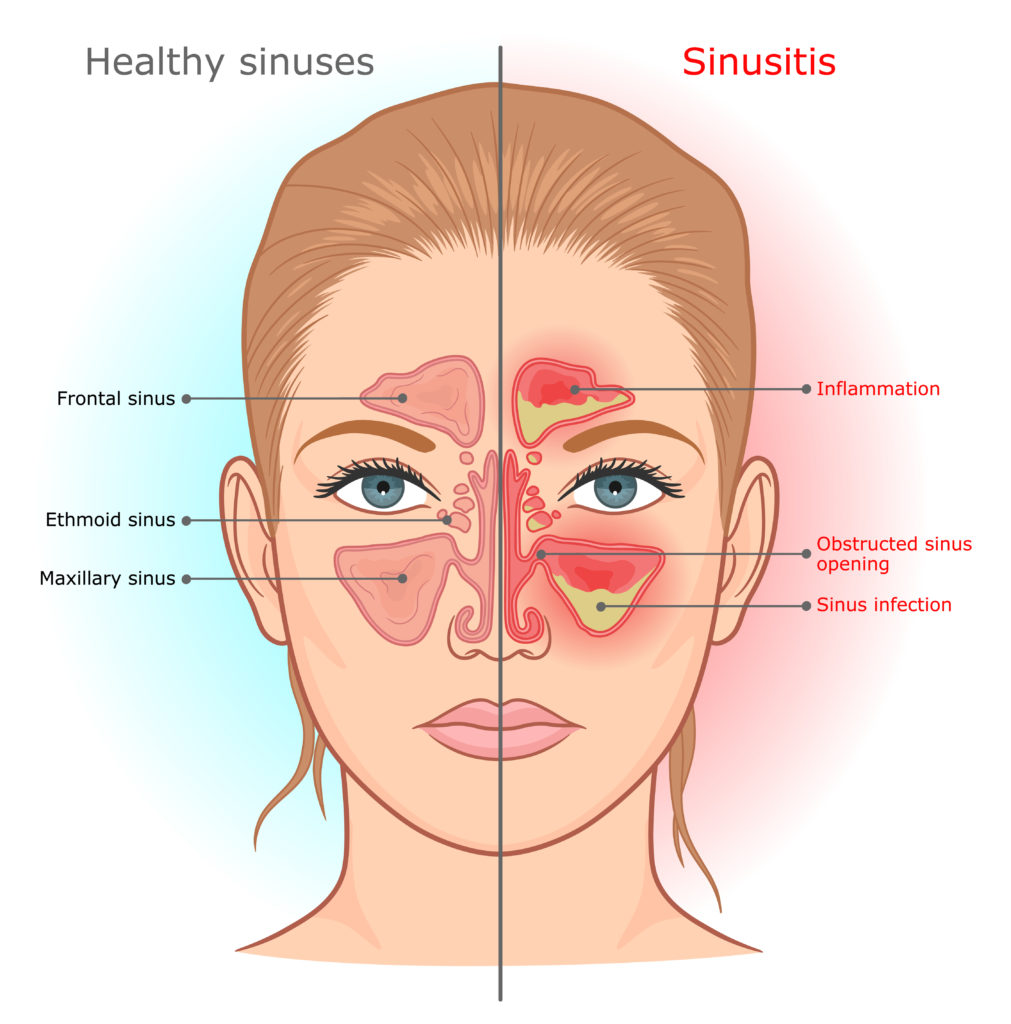
Your Sinus Cavities
You have eight ‘holes’ in your head, meaning your sinus cavities. There are four on the left side of your face, and four on the right side. These should be pretty empty! When one of them fills up, you know about it because you may feel the symptoms of a sinus infection or sinusitis (see graphic comparing healthy sinuses vs. those inflamed in sinusitis).
The “paranasal” sinus cavities are located in your head. You have two frontal ones behind your forehead, two maxillary sinuses behind your cheekbones, two ethmoid sinuses (besides the top part of your nose), and two sphenoids that are directly behind your nose.
What is a Sinus Fungal Ball?
It’s just what it says, a fungal infection in the sinus cavity – it’s usually one-sided. Aspergillus species are the causative organism in most cases. This organism is everywhere, even in garden soil, and in the air we breathe. Not everyone who inhales it gets sick.
Usually you see a sinus fungal ball growing in someone who is immunosuppressed, who takes antibiotics for a long time (like in the case of Lyme disease, or chronic UTIs or COPD, etc). These SFB may also occur in someone who has had serious dental procedures done.
Sinus Fungal Balls are also termed “mycetomas.” Also, they have been referred to as “aspergilloma.”
Aspergilloma is considered older terminology because the fungal mass does not always consist of aspergillus, there are other fungi that can cause it. So I’m calling a “sinus fungal ball” today for the purpose of this article because it is most correct.
It is a fungal infection that is impossible to see from the outside of your face, and difficult to diagnose if you don’t know about it. It is seen only on imaging studies, and can be further elucidated if you take a good history on your patient. History, history, history! If you are a doctor reading this, and your patient has been on numerous courses of antibiotics, or has been diagnosed with repeated sinus infections, or speaks of moving frontal headaches, eye pain and pressure in the eyes or cheek pain, or a bad smell, it’s possible they have a SFB and you can order a CT. Make sure you look at all the different angles though, it can kind of ‘hide’ on there.
If you do know what a SFB is, then determining if you have one becomes much easier! Sadly, those who do not know what a SFB is, may get misdiagnosed. You may go down a deep rabbit hole getting treatment for all kinds of things like headaches, brain fog, oral pain, vision problems, Lyme, mold, autoimmune diseases and other difficult-to-treat medical conditions. If left untreated, the aspergillus infection may spread to the lungs or the cranial nerves. It can at times become fatal if misdiagnosed and therefore left untreated.
The reason is that aspergillus is almost always the causative organism in a sinus fungal ball and it is a bad pathogen. Getting this out surgically is the only way to treat it.
How is a Sinus Fungal Ball (SFB) diagnosed?
Thanks to advanced technology and imaging capabilities, we are able to diagnose problems in the sinus cavity very well today. Your ENT may order an MRI or a CT scan for you. These do not diagnose a fungal ball, but they will show opacity in the sinus region (usually maxillary), and they will paint the picture of something present in your sinuses, which when surgically removed gets sent out for biopsy.
The surgeon can see a green fungus during the operation, which is usually aspergillus. It may also be brown, yellow or black! And it is this observation of fungus that is probably the simplest diagnostic evaluation because the biopsy confirmation isn’t guaranteed. It’s hard to get good biopsy results. There are pictures below. Very often, there is a bacterial infection in there, to go along with the fungal (aspergillus fumigatus) infection.
So in summary, the actual diagnosis is made after the thing is removed! The images show something there – but do not confirm if it’s fungal or cystic in nature.
How Do You Get Aspergillus to Take Up Residence in the Body?
1. Through inhalation
2. Through serious dental procedures
3. Being immunocompromised or getting sick with a respiratory pathogen
4. Inhaling a spore
5. Having a bacterial sinus infection that wasn’t fully cleared, or a blocked ethmoid sinus… because then the parasite takes over because all mold likes to grow in dark, wet places (like a sinus cavity!)
6. People can ingest it from rotten fruit, corn or other foods that are infected by the species
7. Taking oral or IV corticosteroids long-term which suppress immunity and cause opportunistic infections
8. Having diabetes
9. Having neutropenia (abnormally low counts of neutrophils seen in patients with diseased bone marrow, or those taking medications that cause neutropenia). Please review the list of DRUGS THAT ARE ASSOCIATED WITH NEUTROPENIA in this article published in Pharmacy & Therapeutics, 2019.
3 Reasons Why Don’t Antibiotics Work
Antibiotics don’t work for several reasons:
1. Antibiotics don’t kill any bacteria hiding in a biofilm, and this is pretty common up in sinus cavities.
2. The sinuses are dark and moist, so they grow fungus. Antibiotics do not kill fungal colonies.
3. Sometimes the antibiotic prescribed for you isn’t appropriate because it doesn’t kill the actual organism growing in you. Remember biopsies aren’t that telling and rarely grow anything from the mucus culture retrieved from your nasal region.
How to Treat a Sinus Fungal Ball (also called a Mycetoma or Allergic Fungal Sinusitis)
The only true remedy for this problem is outpatient surgery. I know that many sinus doctors will disagree and suggest antibiotics, but in my opinion, these do not cure the fungus or prevent regrowth. The antibiotic may surely kill a bacterial infection (often associated with the SFB) but it will not rid you of the fungal malady. Only surgery can get that out of you. Antifungal drugs like itraconazole or VORICONAZOLE don’t always cure the problem and adversely impact liver function if taken orally for 3 to 6 months. That said, you can administer “azole” drugs right through your neti pot, if your physician is bright enough to know that these drugs can be compounded at a Compounding Pharmacy. Not all compounding pharmacies do it though. But doing so keeps the antifungal local, applied topically through the neti pot, and this helps to kill the remaining fungus that the surgeon could not reach to debride/remove.
Antihistamines are drying agents and may certainly help with mast cell activation and sinus symptoms, but they are not curative and not everyone needs those because again, not everyone with a SFB has a runny nose or any allergic/sinus symptoms. Even if you do have sinus symptoms that benefit from antihistamine (or leukotriene inhibitors), you can’t live on those drugs so if you have severe symptoms and your ENT confirms it is a SFB, then surgery is the best treatment. Remember, you are dealing with a potentially lethal organism that once OUT of the sinus cavities has the potential to cause fatal consequences. Here’s a related article you will like, 5 Natural Antihistamine Foods.
You may also be interested in my other article, The 5 Best Natural Antihistamines.
Or possibly my Vitamin C with Lavitol® which supports mucus production and sinus health.*
Neti pots are useful, but not curative.
Saline nasal sprays are useful, but not curative.
Afrin nasal sprays are not useful, and not curative for a SFB.
Steroid pills are often recommended to reduce inflammation in sinusitis, but I am disagreement with the use of these drugs for most people. I have seen a disturbing trend in people getting worse after taking steroids and it may be due to the fact that steroids have well-documented abilities to fuel fungal growth. So if you take a steroid long-term, even in low dosages, the fungus in your paranasal cavity may grow faster and more vigorously. We know that in immunocompromised patients, steroids may increase secondary fungal infections.
Yet, it’s common practice to see orders for steroids in people with sinusitis. I don’t like seeing that to be honest. It’s okay at a lower dose, but I don’t recommend taking a steroid dose pack, after dose pack, throughout the year. I don’t like to see doctors order high doses either, because unless there is a true indication (for instance, asthma or post-covid management), these can lead to suppressed immunity, which causes fungus to flourish. I have seen the setbacks repeatedly, on the heels of steroids.
So instead, I suggest safer NSAIDs like ibuprofen or naproxen which do not fuel fungal growth. There are natural, herbal extracts that work as anti-inflammatory agents too. These cannot be ruled out because many of the following ALSO have strong anti-bacterial and antifungal benefits.
For example, natural anti-inflammatories may augment NSAIDs and as such, I think black seed oil (Nigella sativa), fish oil (omega-3s), curcumin, ginger, Boswellia, cat’s claw, and/or garlic capsules. The garlic is a fantastic option and one of my favorites because it doubles as an anti-fungal, as well as anti-inflammatory. Do any of these natural alternatives to steroids cure SFB? No, but they are useful for pain and inflammation and cytokine balance, and in my humble pharmacist’s opinion, they will not breed more fungal growth in an immunocompromised person, on the contrary.
Complications of Waiting
Sometimes people with a SFB want to wait and fix this on their own, but I am not in agreement with the “wait and see” approach. It’s not like a sinus cyst, where you can wait and maybe live a life without an issue. It’s a fungus. And as such, it wants to survive and thrive, therefore it may become invasive.
It’s not a hundred percent going to become invasive… in fact, sometimes they resolve on their own over time. But not always – not all sinus fungal balls resolve on their own, so you need to constantly stay on top of testing, imaging, and treatments. Ever see one mushroom in your grass, and the next day there’s 20, and the following week your whole lawn is destroyed?! Fungus doesn’t usually just pack up and leave. It’s not like a cyst where it will stay put and maybe just do nothing!
Fungus can become invasive and leave the sinus cavities and enter the lungs. It’s called invasive at that point. It can become fatal and we see this sometimes in complications of COVID-19. If you take immunosuppressant medications (like a corticosteroid) or have a condition that weakens your immune system, get treatment right away. Invasive fungal sinus infections post covid are very dangerous. There is more information in this ARTICLE published in 2019.
I had a friend of many years, and fellow author active in the environmental field, pass away of invasive (lung) aspergillosis in 2019. It took me by surprise because he was otherwise vibrantly healthy and fit! We used to meet up at Trade Shows, and sometimes have dinner, he was always very kind and famous in his field, we cross-promoted our books in fact. This man was relentless in his efforts to raise awareness and improve the field of environmental medicine, chelation therapy and more… yet ironically, it was an environmental toxin that ultimately led to his demise. I still think of him often 🙁
Anyway, he apparently inhaled the fungus while doing gardening. Aspergillus was not diagnosed in time, they told him he had cancer. The chemotherapy prescribed for him suppressed his immune system over the months he took it. As you might expect, the fungus went WILD! It overtook his respiratory tract, causing fever, chills, coughing up blood, tremendous chest pain, bronchospasm, dyspnea and more. He was treated in ICU but nothing they did could help at that point because as I’ve mentioned before, he was misdiagnosed like many others reading this today! He did not have a sinus fungal ball, this was an aspergillus infection of the lungs.
What About Headaches that Don’t Respond to Conventional Medicine?
Headaches (and facial pain) are also associated sometimes with fungal sinusitis for various reasons. If the pathogen gets into cranial nerves, or gets into the brain, the condition becomes severe rapidly, blindness may occur due to problems with the optic nerve, and demise is inevitable. But I don’t want to frighten you, most of the time a sinus fungal ball stays put. All I am saying is that it’s not guaranteed because in the diabetic, the immunocompromised or the unlucky, the fungus may travel out of the sinuses and enter the lungs or central nervous system.
It caused the death of my dear friend and colleague, and I know several others who have suffered dearly for many years, due to fungal growth in their sinus cavities that went undiagnosed or ignored. You see, the problem is that many ENTs will actually dismiss mucosal thickening, or partial opacity. This is a huge problem potentially because if you do not have any other explanation for your ‘head’ symptoms, don’t ignore the signs on your imaging.
Please see an ENT (preferably two so you can get two opinions) if you have chronic sinus or head-related symptoms that are difficult to treat. I’d say it’s critical if your symptoms are centered around frontal (or temporal) headaches, brain fog, altered mental status like feeling drunk or intoxicated, experiencing eye pain or puffiness, tearing without crying, ear pressure, sinus pressure, pain behind your cheeks, or your temples, pain behind your eyes, or a bad odor that no one else smells. These are the most common symptoms.
As a point of interest, I should tell you that Aspergillus is in no way related to other fungus that you might have, for example, Candida which is often seen in gut. Also, one more note, the production of mycophenolic acid (MPA) is a toxin given off by certain aspergillus organisms, but luckily it’s not given off by the Sinus Fungal Ball which is commonly Aspergillus fumigatus. That MPA is produced as a secondary toxin only by Aspergillus pseudoglaucus species. As for Aspergillus fumigatus, it produces a spore during reproduction and spreads by dumping out a toxin called conidia.
Case Studies
The following people are a handful of those I know with sinus issues.
1. A friend, Spencer – This 51 yo man had chronic sinus problems for over 10 years, mainly parietal/frontal headaches, concentration difficulties, eye puffiness, and facial pain. He would on occasion experience the ‘bad smell’ problem that no one else could smell. Sometimes, he would experience inexplicable altered mental status changes, feeling of ‘drunkenness’ and brain fog, although these symptom are not usually associated with a SFB.
One ENT physician ordered his CT and diagnosed him with a cyst and told him to do nothing, just try to live with it. He extracted some nasal mucus from the sinus area but nothing grew on the C&S. The physician was basing the “cyst” diagnosis on what he saw on the CT scan as a uniform, homogenous area in the maxillary sinus that was completely opacified. A second ENT physician told Spencer that he could make out what was most likely a SFB on the CT scan. He disagreed with the first doctor about it being a cyst. Doctor #2 insisted he could see the fungal ball from a different angle on the same CT scan. The take home point – having a second physician look and a second opinion is critical and important prior to a surgery like this.
Spencer took a chance with the Doctor #2 (the second ENT), and underwent surgery for a suspected SFB. So far, he has yet to experience any of the bizarre symptoms he had prior to the procedure. The horrible smell he lived with instantly disappeared, making eating food a pleasure again. The physician confirmed the SFB after the surgery because he could visually inspect the ‘green fungus’ after cleaning out the maxillary sinus. I posted two pictures here down below, so you can see his before and after.
No cyst was ever found which is what Doctor #1 stated with complete assuredness. Imagine the outcome if Spencer agreed with that decision and never sought Doctor #2!!! Remember, a cyst or nodule won’t kill you, but an undiagnosed Aspergillus fungal ball that gets out of control could, because it may leave the sinus cavity. Here is more information about mortality rates as they pertain to invasive fungal sinusitis, CLICK HERE.
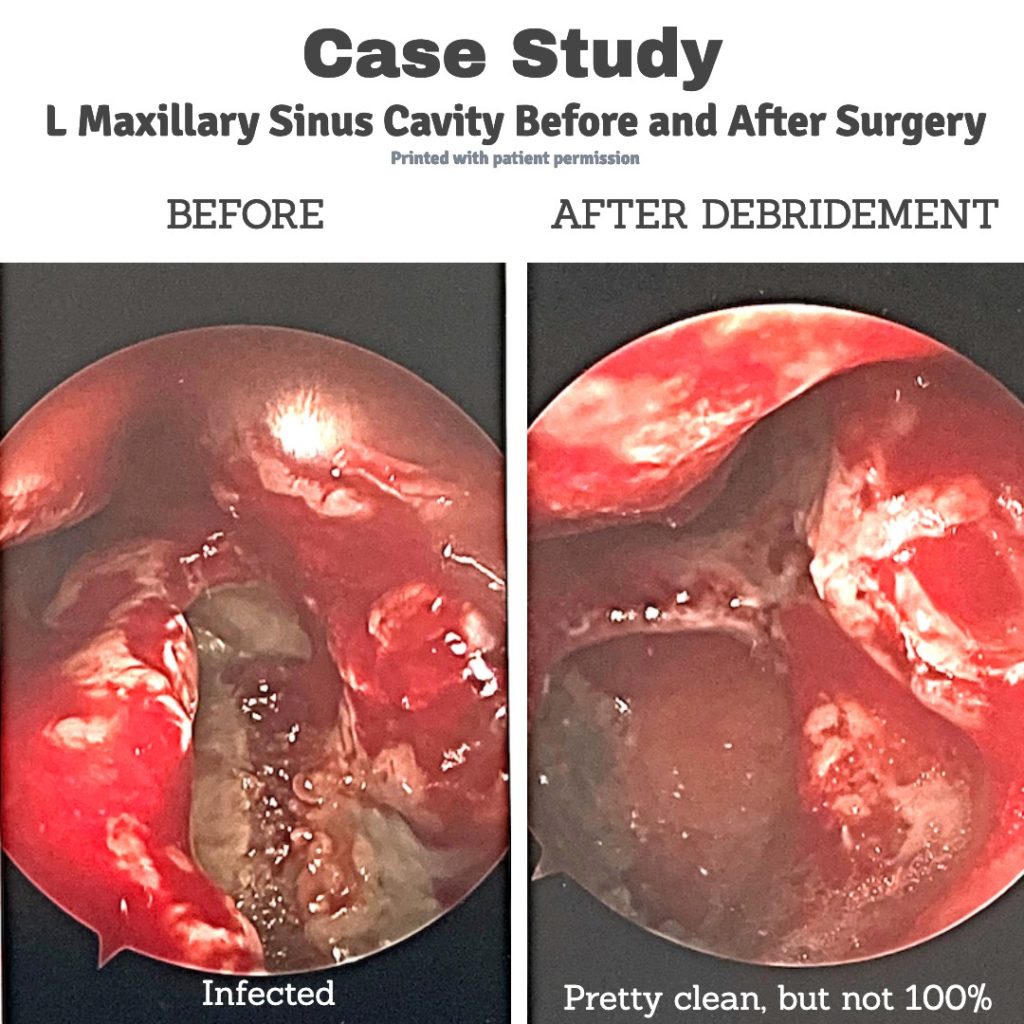
What’s fascinating about this case is the patient’s complete lack of sinus problems, he never suffered with any runny nose, no stuffiness, no infections, all the while the sinus fungal ball caused complete opacification in the left maxillary sinus and triggered disabling symptoms.
2. A colleague, Emma – She has a family and has suffered with chronic sinus infections for many years. They caused non-stop headaches that did not respond to any medication. She is 59 and in 2019 underwent sinus surgery. She did this because her physician told her there was a high risk of the infection spreading and causing meningitis, which could have led to fatal consequences.
Upon hearing the word “meningitis” she opted in for surgery. She is doing well, and has not had another sinus infection since, and remains diligent with neti pot therapy. She is also much less fatigued and feels better overall.
3. A friend, Ayden – I just spoke to him so that I could garner more details to write this article. He is 48 very nice man who has had 20 years of dealing with chronic sinus infections and headaches, as well as brain fog. He pretty much lived on strong antibiotics and medications for inflammation and pain, you can imagine his microbiome at this point!
He underwent sinus surgery in early 2020. Ayden told me, “I am a new man! I have never felt better in my life now that I had that cyst and fungus removed. I try not to think of my life before the surgery, and my wife and I certainly wish I had done it sooner. The antibiotics never helped me, just made me sick.” I asked for Ayden’s picture from his sinus surgery, and I will post it here if he can find it in his files and send it to me. He’s doing great these days and camping, fishing and having a normal life again, for which I am very happy!
4. Jeanne’s sister – I mentioned her earlier at the outset of this article. The lady is a 49 y.o. smoker and while smoking is not a risk factor for a SFB, it does suggest suppressed immunity which puts her at risk for all kinds of infections of the lung, including aspergillus should she become immunocrompromised. I don’t know this person, she is the sister of a friend. I am told that she has been diagnosed with sinusitis repeatedly and given various antibiotics, to no avail, they make her sick. She has tooth pain, but the dentist can find no reason. She has had numerous root canals, and one extraction in 2016.
The likelihood that she has a sinus fungal ball is high in my opinion because she has many symptoms of it, including daily frontal headaches, a foul smell odor that comes and goes, sinus difficulties that only began after her dental extraction. She also has nerve pain in her teeth, as well as right-sided trigeminal neuralgia facial pain. She has a lot of symptoms for a SFB, so I would recommend a CT scan and/or MRI and a proper evaluation with an ENT in her area. She was sadly referred to a psychiatrist for help to cope with her pain, and remains on antibiotics at the time of this writing. I hope she reads this and gets help soon!
Note to Physicians or Other Prescribers on the Front Line and those with ASTHMA
If you see patients, one thing I’d like to highlight now is about asthma. An important aspect of the lung response to pathogens as you know, especially in allergic conditions or MAST cell activation, is that the initial inflammatory response must be dampened, to enter a state of immunological tolerance. A. fumigatus gives off conidia to bronchial cells and this activates the secretion of kynurenine, an anti-inflammatory molecule in an effort to control. That’s because Aspergillus fumigatus is sometimes implicated in asthma and no amount of albuterol or fluticasone, cromolyn, loratadine or even monteleukast will help! If this is of interest, and you have patients with stubborn asthma, please read further research here: Interaction of the Pathogenic Mold Aspergillus fumigatus with lung epithelial cells.
Post-Surgical Tips After Removal of a Sinus Fungal Ball
I confess I do not know everything about this because I do not have sinus problems, and do not have a SFB. But your surgeon will give you specific advice for your individual needs. I am merely stating my opinion here and just trying to help so here goes:
If surgery is indicated, it’s usually done at a surgical center, but sometimes it can be done at a hospital if you have other serious conditions where a hospital setting is safer.
If you have surgery to remove your SFB, it can usually be completed in one hour, and it requires general anesthesia things like propafol, midazolam and others. You will be sent home shortly after the surgery, after becoming more alert and ambulatory. You will be given a prescription for a post-surgical antibiotic to take (sometimes doxycycline or clarithromycin, or others) and I believe they will tell you to start that the same day as your surgery if you’re not too nauseous – but do as your own physician tells you. You will probably have to spray saline nasal spray into your nose every 30 minutes to an hour right after the surgery, starting on Day 1. I’m told they do this in order to keep your nasal passages very moist so it will drain properly, but again, your surgeon or his nurse or P.A. will properly advise you.
You may be told to use a neti pot beginning on Day 2 to help reduce post-surgical blood clot formation, and promote healthy drainage. This is useful to rinse out the nasal passages where blood and mucus are draining. Be vigilant with this neti pot, and learn to use a neti if you don’t already know how because it is important. You can youtube how to use a neti pot and learn.
NOTE AND CAUTION – ALWAYS USE DISTILLED WATER FOR YOUR NETI POT TREATMENT. THERE HAVE BEEN A FEW CASE REPORTS OF PEOPLE DYING FROM BRAIN-EATING AMOEBAS THAT THEY GOT FROM USING CONTAMINATED TAP WATER, OR WATER FILTERED BY REGULAR DRINKING WATER FILTRATION SYSTEMS SUCH AS BRITA, ETC. USE DISTILLED WATER IN NETI POTS.
After surgery, you will need to rest, and avoid heavy lifting after your surgery. You may be sleepy and nauseous right after the procedure, and that is a normal side effect of anesthesia but if it persists, you should call your doctor. Again, follow your surgeon’s advice, I am just giving you general tips here.
Your ENT will give you very specific instructions, what I’ve posted here are just basic guidelines. You will start to feel better within a week. After a month, you will probably feel so much better for having taken out the green fungus from your head! It’s hard to have vibrant health if you’re carrying around a bunch of fungus, and when they die off and reproduce in your sinus cavities, or give off toxic spores… well, you are dealing with poisonous chemicals – some of which can contribute to altered mental status, seizures in invasive cases, and more. These same chemicals can hurt surrounding cranial nerves too, that’s why you see tooth pain, facial or scalp pain, etc.
If you have enjoyed this article, or you have a comment for me, or you wish to add some helpful tips due to your own experience, email me at scriptessentials@gmail.com with full consent and knowledge that I may post your comments on this blog (using only your first name).

Suzy Cohen, has been a licensed pharmacist for over 30 years and believes the best approach to chronic illness is a combination of natural medicine and conventional. She founded her own dietary supplement company specializing in custom-formulas, some of which have patents. With a special focus on functional medicine, thyroid health and drug nutrient depletion, Suzy is the author of several related books including Thyroid Healthy, Drug Muggers, Diabetes Without Drugs, and a nationally syndicated column.
