What's On This Page?
ToggleA middle-aged professional walks into the pharmacy looking exhausted. He’s been clearing his throat all day, feels like something is stuck in his esophagus, and has occasional sharp chest pain. Yet, he doesn’t have heartburn, the symptom we all associate with acid reflux.
He’s been to urgent care twice because the chest pain was so sharp and intense, he feared he was having a heart attack! The ECG was fine, yet his chest discomfort persisted. His physician finally ordered an upper endoscopy when nothing with the heart showed up.
Clearly he is now suspecting GERD. Good call! What the man didn’t know was that silent reflux and GERD can cause long-term damage to the esophagus, even in the absence of heartburn.
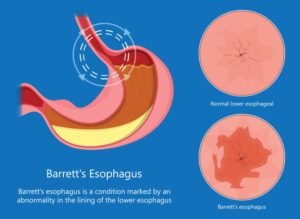
Chronic acid exposure to the esophagus can lead to a condition known as Barrett’s Esophagus, a precancerous change in the esophageal lining that increases the risk of esophageal cancer.
You may be wondering about the name. Back in 1950, British surgeon Dr. Norman Barrett was the first to notice that the esophagus could start looking more like the stomach, growing acid-secreting cells where they shouldn’t be. The surface epithelium of the stomach is composed of columnar cells.
Many people have no idea they have Barrett’s until it is diagnosed during an endoscopy. That’s because it doesn’t always show up with heartburn, the symptoms sometimes look a little bit like allergies. So today, we’ll talk about what Barrett’s is, why it happens, and what can be done to reduce its risks.
What is Barrett’s Esophagus?
Barrett’s Esophagus is a condition where the esophagus “tube” gets exposed to acid more frequently than it’s supposed to. In order to protect itself, the cells in there change and ‘toughen up.’ So Barrett’s is a structural change in the delicate lining of the esophagus, where the normal squamous cells get replaced by columnar cells, which are more resistant to acid, but unfortunately carry a slightly increased risk of cancer.
This transformation is known as intestinal metaplasia and occurs in response to chronic acid reflux (what is aka GERD) or laryngopharyngeal reflux (LPR, also called silent reflux). These are a lot of different names for the same thing, too much acid escaping upward due to a weak lower esophageal sphincter (LES). Barrett’s is like a reflux reality check and too much acid on this delicate tissue is bad.
Some people say it feels like they have “holes” in their esophagus and that’s understandable because severe esophageal irritation can create an intense, sharp, burning pain that mimics the sensation of open wounds or tears. But there are no “holes” or there would be vomiting of blood and fever and severe dysphagia.
So while it may feel there are holes, it’s likely just inflamed, irritated tissue—which can heal! Remember the esophagus is inflamed in this condition, it can feel raw and painful, especially when exposed to acid foods/beverages (like coffee, alcohol, citrus fruits and more). One last thing, some people have touchy nerves, and they become overly sensitive to acid or stretching, making pain feel sharper than the actual damage. Acid irritation can cause esophageal spasms that create stabbing, knife-like pain.
Fast Relief!
- Drink a small amount of warm (not hot) chamomile or marshmallow root tea.
- Try ¼ tea baking soda in 8oz of water and sip, not chug. Don’t do this often, it is just an emergency remedy.
- Try a warm compress on your chest (not ice, which can worsen spasms).
- If pain is unbearable, liquid sucralfate (if available, it requires prescription) can coat the esophagus and provide relief.
The Silent Danger: Barrett’s Esophagus Can Develop Without Heartburn
A common misconception is that only people with severe heartburn develop Barrett’s Esophagus, but this isn’t true. Some people don’t feel any reflux or heartburn symptoms at all, while others may experience some of these symptoms:
- Frequent throat clearing
- A sensation of food stuck in the throat (globus sensation)
- Sharp or burning chest pain
- Chronic cough or hoarseness
- Difficulty swallowing (dysphagia)
These symptoms are often mistaken for allergies, postnasal drip, or muscle strain, leading to unnecessary antihistamines or decongestants. But while the real issue goes untreated, stomach acid continues to damage the esophagus, fueling the growth of harmful columnar cells. This silent progression makes Barrett’s esophagus especially dangerous – by the time it’s diagnosed, the damage may already be significant. It is detected via endoscopy.
How Does Barrett’s Develop?
The lower esophageal sphincter (LES) is the muscular valve between your esophagus and stomach that prevents acid from rising. In GERD and LPR, the LES weakens, allowing stomach acid and digestive enzymes (like pepsin) to damage the esophageal lining. Over time, the body attempts to protect itself by replacing the fragile squamous cells with tougher columnar cells creating Barrett’s Esophagus.
Key Risk Factors for Barrett’s Esophagus:
-
- Long-term GERD (over 10 years)
- Male sex (especially Caucasian men over 50)
- Smoking or alcohol consumption (also vaping and marijuana )
- Obesity, particularly excess belly fat
- Diet (esp acidic, fried, or processed foods)
- Family history of esophageal cancer
- Drinking yerba mate, especially hot. See below for more.
Not everyone with GERD develops Barrett’s, but the longer the esophagus is exposed to acid, the greater the risk.
Is Barrett’s Esophagus Dangerous?
Most people with Barrett’s NEVER develop esophageal cancer. However, a small percentage will progress to dysplasia (the word for precancerous changes). If you’ve had an endoscopy, your doctor may have used some of the following words, let’s break it down:
✔ Non-dysplastic Barrett’s: No immediate cancer risk, but still requires surveillance.
✔ Low-grade dysplasia: Some precancerous changes, may need more frequent monitoring or treatment.
✔ High-grade dysplasia: More aggressive changes, often treated with endoscopic ablation or surgery to prevent progression to cancer.
What Do the Studies Say
This STUDY, published in Diseases of the Month in January 2020, explores Barrett’s esophagus and its cancer risk. It highlights how radiofrequency ablation (RFA) a technique that uses heat to remove abnormal tissue, can significantly lower the odds of Barrett’s progressing to esophageal adenocarcinoma, especially in high-risk cases. It’s not a magic fix, but it’s a promising option to help keep that cancer threat at bay for people with concerning Barrett’s changes!
This 2023 STUDY dives into Barrett’s esophagus and its sneaky link to esophageal adenocarcinoma. Researchers found that folks with Barrett’s have a yearly risk of about 0.12% to 0.5% of developing this cancer—translating to a lifetime risk of roughly 5% to 7%. That’s not sky-high, but it’s a heck of a lot more than the general population’s tiny 0.03% risk. It’s a reminder that chronic reflux isn’t just heartburn—it’s a red flag we need to watch closely!
Yerba Mate Beverages
A 2009 study from Uruguay, published in Cancer Epidemiology, Biomarkers & Prevention, explored whether yerba mate – that popular herbal tea – ups the risk of esophageal cancer. Researchers compared 344 people with esophageal squamous cell carcinoma to 469 healthy folks and found something striking: drinking over 1 liter of mate daily nearly tripled the risk. Most people don’t guzzle that much, thankfully! But here’s the thing, sipping it very hot (around 150°F or 65°C) almost doubled the risk on its own. The heat, not just the herb, seems to be the troublemaker.
And if you mix heavy mate drinking with smoking and alcohol? The risk for esophageal cancer shoots up over 7-fold! The takeaway: if you love mate, keep it moderate and let it cool off first. Repeatedly scalding your esophagus with hot liquids, or piling on smoking and drinking, could spell trouble over time, even if this cancer type differs from Barrett’s usual suspect, adenocarcinoma.
How is Barrett’s Diagnosed?
Since Barrett’s Esophagus doesn’t cause unique symptoms, the only way to confirm it is through an upper endoscopy (EGD) with biopsy. Most people see the doctor complaining of something other than heartburn, for example, food that gets caught in their throat, difficulty swallowing, hoarseness or changes to their voice.
An endoscopy is usually done as an outpatient procedure where they put you to sleep with some light anesthesia. Once the lights go out, the doctor inserts a thin scope through your mouth and gently slides it down. You don’t feel anything, you’re out cold. The scope can “see” things and it can examine the esophagus and take small tissue samples to biopsy and check for cellular changes. Results are sent within a few days to your doctor so they can see if there are any cellular changes, strictures, or other issues. A stricture is a narrowing of the esophagus caused by scar tissue, inflammation, or damage, making swallowing difficult.
Other tests that may help assess reflux severity include:
✔ Barium Swallow (Esophagram) – You go to the hospital or imaging center and drink a thick “drink” with the contrast in it while the tech takes an Xray of your esophagus. This test can reveal structural issues, such as strictures or a hiatal hernia. An upper endoscopy (EGD) test can also see if there are strictures, and it’s more definitive than the Esophagram (barium swallow X-ray).
✔ pH Monitoring Test – Measures acid levels in the esophagus over 24 hours. A thin catheter or wireless capsule (Bravo pH monitor) is placed in the esophagus to measure acid levels over 24-48 hours. The patient records symptoms and activities while the device tracks reflux episodes. If using the Bravo capsule, it’s placed via endoscopy under sedation, but after that, you’re awake.
✔ Manometry Test – Evaluates esophageal muscle function. This is an uncomfortable test for people due to the strange sensation and gagging possibility, but it’s still necessary in certain cases to determine muscle function of the esophagus. A thin, pressure-sensitive tube is inserted through the nose into the esophagus to measure muscle contractions and LES function while swallowing. This helps diagnose esophageal motility disorders like achalasia or weak LES tone in GERD.
How to Treat & Prevent Barrett’s Esophagus
If Barrett’s is confirmed, the goal is to prevent further damage and lower the risk of progression. The pain may be tolerable, or it could be unbearable. This is an individual experience, and bear in mind that there is something called “referred pain” from acid splashing up. So even a small amount of reflux can inflame nerve endings, making pain feel much worse than the actual damage. Don’t worry til you have to.

Medications to Reduce Acid Exposure:
✔ PPIs (Proton Pump Inhibitors) – First-line treatment
- Dexilant (Dexlansoprazole): Dual-release formula, longer acid suppression, best for severe GERD. Probably the best of the drug treatments. Sometimes this requires pre-authorization, a doctor may try omeprazole or pantoprazole first, so that insurance covers the Dexilant® which is better (but again, it’s not the first drug prescribed).
- Omeprazole, Pantoprazole, Esomeprazole (Nexium®): Next best in this category, this is a standard option for people, but requires timing before meals.
- H2 Blockers (Pepcid): Weaker than PPIs, used for nighttime acid control. Famotidine (Pepcid®) is a good choice in this category.
✔ Sucralfate (Carafate) – Forms a protective coating over erosions. Available by prescription only. You can swallow it whole or you can make a slurry with the tablets.
✔ Gaviscon Advance (UK Version) – Creates a floating barrier to prevent reflux.
Lifestyle Modifications to Reduce Reflux:
- Elevate the head of the bed by 6-8 inches (not just pillows)
- Eat smaller, more frequent meals – control portions
- Avoid late-night eating (absolutely no food 3 hours before bed)
- Eliminate acid triggers: No citrus, tomatoes, chocolate, coffee, alcohol, mint, fried foods, or carbonated drinks
- Lose excess weight, especially belly fat (which increases intra-abdominal pressure)
- Don’t eat and then lie down, sit up for 2 hours before lying down
For patients with severe symptoms despite medications, surgical options like LINX® procedure (magnetic ring around the LES) or Nissen fundoplication (stomach wrap to strengthen the LES) may be considered. I shared a little information about LINX® in this article, 5 Hidden Links Between Hiatal Hernia, GERD & Shortness of Breath – and Solutions.

Essential Steps to Manage GERD & Protect Your Esophagus While Waiting for Your Appointment
If you’re experiencing painful GERD symptoms or suspect Barrett’s esophagus, taking action now can help reduce acid exposure, protect your esophageal lining, and promote healing while waiting for medical evaluation.
1️⃣ Modify Your Diet to Reduce Reflux
-
Avoid acidic, spicy, fried, caffeinated, and processed foods.
-
Stick to alkaline, low-fat, and easily digestible options, such as:
-
Oatmeal, white rice, bananas, steamed vegetables, skinless poultry, and non-citrus fruits.
-
Healthy fats like avocado and olive oil (in moderation).
-
Non-acidic herbal teas (like chamomile or marshmallow root tea).
-
-
Eat small, frequent meals to prevent stomach pressure buildup.
2️⃣ Use Soothing Natural Remedies
-
Slippery Elm & Marshmallow Root – These coat and soothe the esophagus. Drink as tea or mix the powder in water. Watch my youtube VIDEO NOW: Relieve Abdominal Pain in Under 2 minutes by Suzy Cohen, RPh.
- Watch this VIDEO: Health Benefits of Marshmallow Root Herbal Tea
-
DGL (Deglycyrrhizinated Licorice) – Take chewable tablets or powder 15-20 minutes before meals to protect the esophageal lining.
- Zinc Carnosine – Helps repair tissue damage from acid reflux, and a typical dose is 75 mg twice daily. Studies suggest taking it with meals to boost absorption and avoid stomach upset, though some folks find it works fine right after eating too – splitting hairs, it’s about what your tummy tolerates best!
3️⃣ Consider a PPI Like Omeprazole (Now Sold OTC)
-
If symptoms are severe, a proton pump inhibitor (PPI) like omeprazole or Dexilant may help reduce acid production.
-
Take one dose every morning, 30-60 minutes before eating for best results.
-
PPIs can deplete magnesium, B12, and zinc – consider supplementation, especially magnesium glycinate which is in my CHELATED MAGNESIUM capsules.
4️⃣ Add a GERD-Safe Probiotic
Not all probiotics are GERD-friendly – certain strains can increase gas and fermentation. Choose:
✔ Bifidobacterium infantis – Supports digestion & reduces inflammation.
✔ Bifidobacterium longum – Strengthens gut lining integrity.
✔ Lactobacillus rhamnosus GG – Helps regulate digestion.
Avoid: Lactobacillus casei, reuteri, or bulgaricus, which can trigger histamine and worsen reflux in this case.
5️⃣ Check for Underlying Infections & Imbalances
- SIBO (Small Intestinal Bacterial Overgrowth), H. pylori, and Clostridium overgrowth can worsen GERD which increases risk.
- Consider a GI Effects stool test or a SIBO breath test to rule out infections or dysbiosis. SIBO increases risk for Barrett’s esophagus.
- Talk to your doctor about treating SIBO if found, as bacterial overgrowth can contribute to reflux symptoms.
6️⃣ Herbal & Natural Compounds That May Help Barrett’s Esophagus
✔ Mastic Gum (500-1,000 mg daily) – Supports esophageal healing and fights H. pylori.
✔ Curcumin (500-1,000 mg with black pepper or fat) – Reduces inflammation & oxidative stress.
✔ Melatonin (3-6 mg before bed) – May strengthen the LES (lower esophageal sphincter) and reduce reflux.
7️⃣ Peptides That May Support Esophageal Healing
✔ BPC-157 – A synthetic peptide that promotes tissue repair and may aid esophageal healing.
✔ Thymosin Beta-4 (TB-500) – Supports tissue regeneration and reduces inflammation.
While you wait for your appointment, taking proactive steps can reduce inflammation, protect the esophageal lining, and help manage symptoms. PPIs, dietary changes, soothing herbal remedies (DGL, slippery elm, zinc carnosine), and probiotics can all work together to provide relief. If symptoms persist, testing for bacterial overgrowth or infections may uncover hidden triggers.
Final Thoughts
If you’ve had chronic GERD for more than 10 years, trouble swallowing, or persistent throat issues, an endoscopy is necessary to check for Barrett’s. Don’t wait too long. The risk of cancer is low, but not zero, so early detection makes a difference.
This 2020 STUDY from Frontiers in Pharmacology, 2020 dives into Barrett’s esophagus and cancer risk. It found that people with Barrett’s who have a family history of esophageal adenocarcinoma face a higher chance like up to 2.5 times of developing it themselves. It’s not just reflux—or how much hot salsa you scoop up—that matters – your genes could be quietly raising the alarm too! Let me touch on genes next, just in case you want to see if you have them.
Genetic Testing
Testing for genes like COL1A1 and SPP1 can be done with a cheek swab or blood test, and several companies offer this through at-home kits or clinical labs. Big name labs like 23andMe (which is going out of business), or AncestryDNA don’t specifically target these genes, they focus on ancestry and broad health traits… but specialized outfits like INVITAE, or possibly Labcorp can analyze them if ordered by a doctor. It’s not a test I recommend though, your genes only play a role, they are not predictive, and knowing these results will only create mental chatter.
You’ll usually need a doctor or practitioner’s license to order these tests, especially for something tied to Barrett’s or cancer risk, since they’re not standard in over-the-counter (home) kits. If you insist on testing your genetic mutations, just check with your practitioner to get the right test.
I hope my article has helped you. If you suspect you have GERD or Barrett’s Esophagus, talk to your doctor about screening options, and tests because prevention is always better than treatment.

Suzy Cohen, has been a licensed pharmacist for over 30 years and believes the best approach to chronic illness is a combination of natural medicine and conventional. She founded her own dietary supplement company specializing in custom-formulas, some of which have patents. With a special focus on functional medicine, thyroid health and drug nutrient depletion, Suzy is the author of several related books including Thyroid Healthy, Drug Muggers, Diabetes Without Drugs, and a nationally syndicated column.