Many seniors experience dysphagia, which is the term for people who have difficulty swallowing their food or pills. Difficulty can be defined in many ways, but it usually means extra time and effort transferring the food or liquid (or pills) down from the mouth, to the stomach. People describe dysphagia differently because the symptoms vary widely.
Dysphagia refers to difficulty swallowing, whereas dysphasia refers to difficulty with speech such as that experienced post-CVA.
Initially one may frequently need to clear their throat, or have a hoarse voice for a few minutes.
Other Symptoms of Dysphagia
Chronic cough of unknown etiology
Choking sensation
Regurgitation of food
Sensation of fullness or pressure while eating
Burning sensation in the chest (sternal) area while eating
Food “sticking” in the throat
Meal avoidance due to discomfort
Malnutrition
Respiratory infection
Aspiration pneumonia
In the most serious cases, food or pills may be aspirated and result in pneumonia which then requires hospitalization for proper care.
Most of us have experienced the sensation of dysphagia at one time or another. It can happen by simply eating too large a bite, or not chewing enough. A swallowing issue may be felt if you have a dry mouth, or if you swallow while lying down or even laughing or talking. To resolve simple cases of dysphagia, you should eat smaller meals that include softer food, and chew well. Along that venue, I suggest avoiding sticky things like caramel, peanut butter. Eliminating caffeine, tobacco and alcohol is important as these can make heartburn worse and cause dysphagia. Sometimes thickeners are used to change the texture of food.
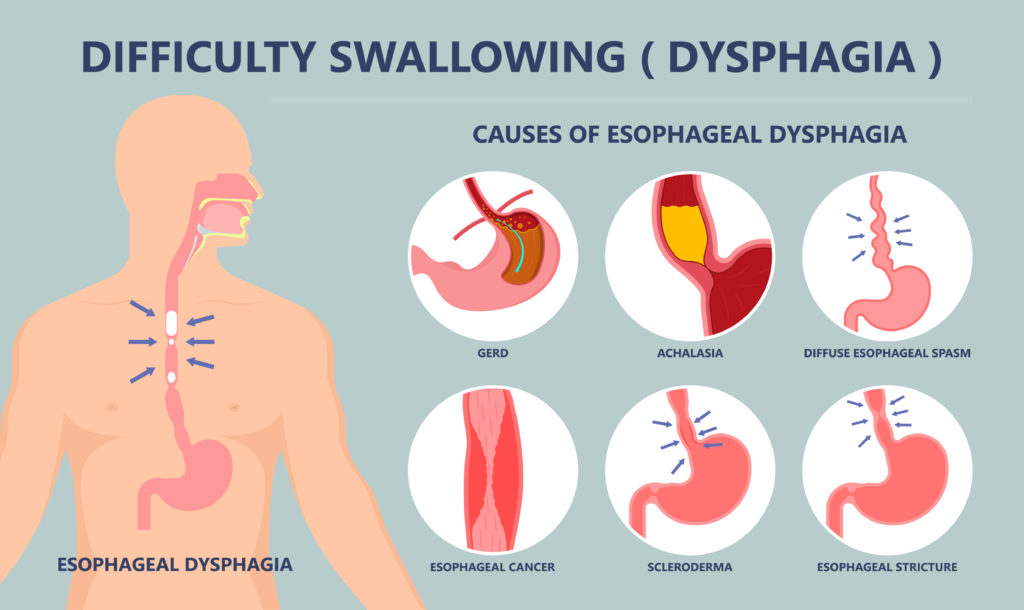
Causes of Dysphagia and Testing
Treatments vary for each individual and hinge on many factors such as age, the severity of the dysphagia and underlying medical conditions that are causing the symptom of dysphagia.
A Barium Test is conducted as part of a larger evaluation to rule out a hiatal hernia which causes an obstruction in the lower esophagus and therefore delays emptying the food contents into the stomach. Many conditions are associated with the symptom of dysphagia, including scleroderma, multiple sclerosis, a stroke, tumor obstructions, reflux disease (GERD) and more, so testing a person and finding out the WHY is critical to resolution.
Sometimes people develop dysphagia rather suddenly. It can happen suddenly too, which is quite scary and life-changing. When I worked in the nursing home setting, we saw this frequently occur with new admissions who were started on medications that induced the dysphagia. Their loved ones didn’t realize what was happening either, but in some cases, a new medication can give a loved one dysphagia. You need to be aware of that before they put a feeding tube into your loved one. Sometimes it’s related to a drug side effect, and oftentimes the medication can be switched to something else that does not induce dysphagia. Here are some other causes, shown in this graphic.
Reasons for Dysphagia
One other reason people have dysphagia is that they’re forced to swallow big pills. The mere swallowing of a large pill, for example, antibiotics like metronidazole or sulfamethoxazole, can cause pain in the chest area. It doesn’t help these pills are so big and powdery that it can make anyone gag, no matter their age. Moreover, these drugs and many others can cause one to vomit them back up! And if that happens, the person now has caustic stomach acid refluxing into the delicate esophageal tissue. The use of acid blockers like famotidine and demulcents (slippery elm or marshmallow) can bring immediate relief, and may prevent your loved one from having a tube inserted unnecessarily because it looks like they’ve suddenly developed dysphagia.
In my field, we have a saying, “History, history, history!” If someone takes a good history and finds out exactly when the dysphagia started, you might be able to see the cause. Once that is pin-pointed, the proper treatment can be given. Keep in mind that sometimes people with dementia develop dysphagia, which could be associated with the aging process.
In a moment, I will list the most common offenders, but I want to make sure that I’m clear… the drugs I list do not always cause the dysphagia. That symptom may be related to some genuine obstruction. So you cannot blame the drug until you first rule out other esophageal and stomach conditions as well as muscle and nerve problems. People with Parkinson’s and other neurological conditions can develop dysphagia. A physician can offer more advice on testing.
As for the medications that induce dysphagia, they are listed below.
As you will soon see, there are many categories of drugs — some of which induce dysphagia as a direct side effect, and others that increase the risk by harming the esophagus or causing dry mouth. Regardless, if you are taking any medication listed herein (or others that I have not listed but fall in the same category), speak to your physician about your alternatives, and about treatment for dysphagia.
Examples of Medications Associated with Dysphagia
Sedatives and CNS depressants
This is probably the most common offender in people because these agents reduce voluntary muscle control which therefore makes it more difficult to initiate swallowing. Usually, it’s as simple as switching the medication to another agent, and I should stress that weaning these types of drugs is imperative. You should never let the doctor suddenly stop them, they must be weaned. In this category, you have benzos, analgesics and muscle relaxers. I’ve outlined them here:
Benzodiazepines:
Alprazolam (Xanax)
Clonazepam (Klonopin)
Clorazepate (Tranxene)
Diazepam (Valium)
Lorazepam (Ativan)
Analgesics and narcotics:
Alfentanil (Alfenta)
Codeine (Tylenol #2, #3 and #4)
Fentanyl (Duragesic)
Hydromorphone (Dilaudid)
Meperidine (Demerol)
Morphine (Astramorph, MS Contin, Roxanol)
Oxycodone (OxyContin, Roxicodone)
Propoxyphene (Darvon, Darvocet)
Muscle Relaxers:
Baclofen (Lioresal)
Cyclobenzaprine (Flexeril)
Tizanidine (Zanaflex)
Neuroleptics a.k.a. Antipsychotics
Chlorpromazine (Thorazine)
Clozapine (Clozaril)
Fluphenazine (Prolixin)
Haloperidol (Haldol)
Lithium (Eskalith, Lithobid)
Loxapine (Loxitane)
Olanzapine (Zyprexa)
Quetiapine (Seroquel)
Risperidone (Risperdal)
Thioridazine (Mellaril)
Thiothixene (Navane)
Trifluoperazine (Stelazine)
Medications that Potentially Harm the Esophagus
The next most important category of medications that can induce dysphagia are those that directly harm the delicate esophageal tissue. As we age, this tissue becomes even more sensitive to the caustic effects of certain medications. Elderly patients are more prone to esophageal injury because they have the predisposing factors.
First, they are the group that is taking a lot of pills all day which leads to more potential injury of this tissue. Secondly, their motility is reduced as is saliva production. This impairs the transport of medication while increasing the contact time with their esophageal tissue. Many drugs have a low pH, or they’re too big, or uncoated, and so forth. Here are the categories of medications and some examples.
Antibiotics that have an acidic moiety as part of their structure:
Clindamycin (Cleocin)
Doxycycline (Vibramycin)
Erythromycin (Ery-tabs, Emycin)
Minocycline (Minocin)
Pentamidine (NebuPent)
Tetracycline (Sumycin)
Bisphosphonate Bone Builders:
Alendronate (Fosamax)
Tiludronate (Skelid)
Aspirin or Salicylates
NSAIDs (Non-steroidal Anti-inflammatory Drugs)
Ibuprofen (Advil, Motrin)
Indomethacin (Indocin)
Ketoprofen (Orudis)
Naproxen (Aleve, Naprosyn)
Others
Iron supplements
Vitamin C synthetic supplements in high doses “ascorbic acid”
Potassium Replenishment:
K-Dur
K-Tabs
Klor-Con
Micro-K capsules
Slow-K
Methylxanthines – Asthma Medications
Theophylline (Theo-Dur, Unidur, Slo-Bid)
Steroids
Dexamethasone (Decadron)
Methylprednisolone (Medrol, Solu-Medrol)
Prednisolone (Delta Cortef)
Prednisone (Deltasone)
Immunosuppressants
Azathioprine (Imuran)
Carmustine (BiCNU)
Cyclosporine (Sandimmune, Neoral)
Daunorubicin (Daunomycin)
Lymphocytic immunoglobulin (Atgam)
Paclitaxel (Taxol)
Porfimer (Photofrin)
Vinorelbine (Navelbine)
Anticholinergic Medications
The following drugs have “dysphagia” as a potential side effects but it’s not direct. The link here is due to their drying effects on the body (termed anticholinergic effects):
Atropine (Atropar)
Benztropine mesylate (Cogentin)
Dicyclomine (Bentyl)
Hyoscyamine (Cytospaz)
Ipratropium (Atrovent)
Oxybutynin (Ditropan)
Propantheline (Pro-Banthine)
Scopolamine (Transderm-Scop)
Trihexyphenidyl (Artane)
Tolterodine (Detrol)
Medications for Cold/Flu or Allergy Including Antihistamines and Decongestants:
Chlorpheniramine (ChlorTrimeton)
Cyproheptadine (Periactin)
Diphenhydramine (Benadryl also sold as Sominex)
Hydroxyzine (Atarax, Vistaril)
Pseudoephedrine (Sudafed)
Loratidine (Claritin)
cetirizine (Zyrtec)
Levocetirizine (Xyzal)
ACE Inhibitors used for Cardiovascular Disease:
Captopril (Capoten)
Lisinopril (Prinivil, Zestril)
Enalapril (Vasotec)
Moexipril (Univasc)
Valsartan (Diovan)
Quinapril (Accupril)
Perindopril (Aceon)
Ramipril (Altace)
Drugs for Heart Rhythm
Disopyramide (Norpace)
Mexiletine (Mexitil)
Procainamide (Procan)
Others
Drugs that Manage Nausea and Vomiting:
Meclizine (Antivert)
Metoclopramide (Reglan)
Ondansetron (Zofran)
Prochlorperazine (Compazine)
Promethazine (Phenergan)
Antidepressants in the Tri-cyclic (TCA) category and Selective Serotonin Reuptake Inhibitor (SSRI) class:
SSRI Antidepressant Examples:
Citalopram (Celexa)
Fluoxetine (Prozac)
Nefazodone (Serzone)
Paroxetine (Paxil)
Sertraline (Zoloft)
Venlafaxine (Effexor)
TCA antidepressants:
Amitriptyline (Elavil)
Desipramine (Norpramin)
Imipramine (Tofranil)
Amoxapine (Asendin)
Doxepin (Sinequan)
Protriptyline (Vivactal) – also used for narcolepsy
Trimipramine (Surmontil)
There are others not listed here because I did these lists mostly off memory since I have been a pharmacist for 30 years. So if you have a medication that you take and think it might be in one of these categories, please ask your local pharmacist to verify that, and speak to your practitioner(s) about a therapeutic alternative. CLICK HERE for a LIST of other medications that have been implicated in dysphagia.
As for treatments of dysphagia, it depends on the actual cause and whether or not it is drug-related or medically related to your condition (ie Parkinson’s, dementia, MS, diabetes or others). It also depends on whether the dysphagia problem stems from the area of the mouth/throat or the esophagus.
Speech therapists (also called “Speech and Language Therapists”) can help, because there are exercises that they can teach you to strengthen muscles in the area.
A dietician will almost always be required to help determine the best type of diet for you. Sometimes surgery is needed, as well as acid-blocking medications. The latter is commonly sold over-the-counter in any pharmacy and includes popular names like Pepcid (famotidine), or the PPI drug Omeprazole (Prilosec).
In the most severe cases, a feeding tube is inserted in order to provide the person proper nutrition (and prevent malnourishment and dehydration). This is usually temporary while a person is recovering their own ability to swallow.
There are 2 types of feeding tubes and your doctor will ONLY use these if necessary:
- An “NG” tube – short for nasogastric tube – requires a tube to be passed through your nose all the way down into the stomach. These are designed for short-term use while you heal, usually a week or two. Beyond that, it gets very uncomfortable for a patient to wear.
- A “PEG” tube – a percutaneous endoscopic gastrostomy tube – is surgically implanted directly into the stomach and is more permanent and remains in place for several months. Many people prefer this tube because it’s hidden underneath their clothing and allows for easier walking/mobility. It can be removed after a couple of months if need be, it is not necessarily a permanent insertion.
The difficulty with feeding tubes of course is the inability to eat and taste food like normal, which is a pleasurable thing. This can lead to severe depression and melancholy. Do your best to avoid the need for these extreme treatments by recognizing dysphagia right away in a loved one. Once you see it manifesting, urge your loved one (parent, spouse, friend) to get treatment because this is a very treatable symptom in most cases. For more information, follow these resources:
Here’s a link to the National Foundation of Swallowing Disorders.
Here’s a link to the National Speech, Language and Hearing Associationhttps://www.asha.org/Practice-Portal/Clinical-Topics/Adult-Dysphagia/ site.
Link to Dysphagia Research Society.
Link to IDDSI – International Dysphagia Diet Standardization Initiative.
10 Tips to Enjoy Eating with Dysphagia
Sometimes, in a case where the person has a sudden onset of dysphagia, all they need for treatment is an acid blocker (given by shot) and some steroids to help reduce the spasm/pain. It doesn’t work every time, but it can in some people. If food is allowed, the diet varies and a dietician can weigh in on what’s best. There are different levels of dysphagia and the diet is 100% contingent on the level you are at. I cannot emphasize this enough. There is a LINK you can click on to see what the different diets are for each level. This information is derived from the National Dysphagia Diet Task Force.
I also found another paper written by Dr. Jean Justad from Montana about DYSPHAGIA and DIET which may be of interest to you. I can offer general suggestions here for people who have mild dysphagia and are allowed to eat but you should still ask your dietician or doctor what is right for you:
1. Eat a “Mechanical Soft” or liquid diet that has been thickened (with “nectar thick”) if you are mild/moderate.
2. If permitted, use 1 “nectar mildly thick” packet for every 4 ounces of liquid or follow directions on your product. Some come as packets that are easy to use, and other products come as bulk tubs. There are several thickening products on Amazon, including Clear DysphagiAide Thickener Powder or another option Thick-It. Thickeners are useful but you have to know what you’re doing, and how thick to make the food. There are different ways to thicken foods, such as “honey thick” for example. Thicker is not always better.
3. No hard foods like steak or chicken, and no rice, peas or corn which may flow back to the throat before they’re chewed. Bread is especially troublesome, and so is peanut butter. Their texture makes them especially dangerous if they get stuck in the back of the throat.
4. Baby food might be okay depending on consistency, and what the person is allowed. Thickening agents may be required on certain baby food meals.
5. Direct supervision during all meals in case of choking or difficulty.
6. Medications have to be crushed in applesauce (make sure they are crushable and never crush anything that is sustained release or long-acting). Here is a LIST OF NON-CRUSHABLE MEDICATIONS.
7. Take small sips and little bites
8. Sit UPRIGHT while consuming food or drinking, do not attempt to swallow foods/beverages or pills while lying down because there is a higher risk for aspiration.
9. Do dysphagia exercises. If you CLICK HERE you’ll be taken to the National Foundation of Swallowing Disorders website, where you can download a PDF of swallowing EXERCISES.
10. Try improving lung capacity and breathing techniques each day with a device such as The Breather, or similar. Here’s the Amazon LINK.
I hope you’ve enjoyed this article and learned something to help a loved one (or even yourself). Forward it if you think it will benefit others. As a final note of caution, please ask your practitioner(s) what diet is right for your specific situation. Remember, having “dysphagia” means you have a symptom and there are variations of it, and proper treatment depends on what level you are, and how long you’ve had it, as well as its etiology. Feel free to email me at scriptessentials@gmail.com if you would like to share your own tip that could help someone else. I’ll post a few below later on.

Suzy Cohen, has been a licensed pharmacist for over 30 years and believes the best approach to chronic illness is a combination of natural medicine and conventional. She founded her own dietary supplement company specializing in custom-formulas, some of which have patents. With a special focus on functional medicine, thyroid health and drug nutrient depletion, Suzy is the author of several related books including Thyroid Healthy, Drug Muggers, Diabetes Without Drugs, and a nationally syndicated column.