What's On This Page?
ToggleIn this article, you will find at least 10 novel treatments for chronic itch, eczema and skin infections. The average person is estimated to scratch an itch on their body about a hundred times a day, and that is considered pretty normal.
But what if you have a chronic itch? The scratching could be non-stop and you could scratch yourself to the point of bleeding! I can help you today. Itching is one of those symptoms that will drive you mad unless you get to the root cause and treat it. This can be the most difficult part. Treatment is not that hard if you know exactly what you’re treating! Itching and rash names go by many other terms in the medical community.
Unfortunately, digging deep isn’t what happens at first when you show up at the doctor’s office with an itchy rash. You will have to go to the pharmacy to pick up a prescription steroid like a Medrol® (methylprednisolone) Dose pack, and some Benadryl… perhaps even some calamine lotion. If you’re among the lucky ones, your itchy sensation will magically clear up. Here are 7 other quick remedies you can try for general, itchy rashes/spots on your skin:

7 Quick Methods to Control Itch
1. Apply a cold wet compress to the itchy rash for 5 minutes
2. Run an ice cube over the spots
3. Moisturize your skin if it is dry and flaky
4. Apply a dab of diluted tea tree oil or commercial anti-fungal creams for itchy spots
5. Apply something topical containing camphor or menthol (Sarna lotion or Carmex ointment)
6. Cut off a piece of aloe plant and rub directly on the itchy spot
7. Apply dabs of either green clay, or black charcoal mask, let dry and then rinse off.
What if the itch is chronic?
What if it doesn’t clear up with standard, over-the-counter or natural remedies? What if you live with itch? What happens to you then is truly a lot of suffering and I have so much compassion for you. Insomnia is always part of the problem with the misery of chronic itch syndromes and skin infections. The accompanying painful rash could baffle you, and your practitioners for weeks, sometimes months and years!
Itchy rashes are the result of dozens of problems. You can experience an itchy rash from an allergy to latex, mangoes or seafood. It could be a drug eruption, meaning a medication-induced reaction. As an example, you may get opiate-induced itching, or an allergic rash to tetracycline or sulfa drugs.

Sometimes people experience rashes from a bee sting, mites (scabies) or bed bugs. There are many reasons you might itch including bacterial, viral and fungal mold causes. An itch could be autoimmune driven as you see in psoriasis or eczema. Whatever the cause, the problem may become disabling, unsightly and painful!
The underlying mechanism that causes itch may be driven by several factors, but it always results in a cytokine storm.
Could it Be Thyroid Related?
Yes, that’s possible. It’s not that rare. Thyroid disorders may lead to changes in sweating, either increasing or decreasing it, which in turn can contribute to itchiness under specific circumstances. Graves’ disease and Hashimoto’s disease are two different autoimmune thyroid conditions where the body’s immune system mistakenly targets the thyroid gland’s healthy cells. Itchy skin is a common symptom associated with both of these thyroid diseases.
If you are wondering if you have hypothyroidism, or simply don’t know but you know you are fatigued, take 10 minutes to read, 5 Signs of Thyroid Imbalance and How to Adress them Naturally.
For most people, the itch is NOT related to the thyroid gland, but I just wanted you to know it was possible, especially because autoimmune disorders are on the rise (as of 2024 anyway, they have been on the rise for a couple of years!)
Let’s get to helping you right now. The following is a list of chemicals released during itchy skin conditions:
Leukotrienes.
Usually this cytokine is involved in airway problems such as asthma, but it may also be elevated with chronic itchy conditions. Singulair® is a medication that can help reduce leukotrienes. New research shows that leukotrienes are released by basophils too.
Boswellia, curcumin and glycyrrhiza are 3 different natural leukotriene inhibitors.
Histamine is high during mast cell activation which causes itch
This is a well-known mediator of itch and allergy. Histamine release will cause those well known symptoms like redness, itching, swelling, wheezing, itchy eyes and flushing. Histamine is caused when your mast cells are activated sometimes termed Mast Cell Activation Syndrome. This just means your mast cells are dumping histamine like crazy!
Mast cells are not the only way to dump histamine. There’s new and important research to prove that basophil cells are releasing it too. Basophils are white blood cells. Histamine is not only stored in mast cells, but it’s also stored in basophil cells. The mast cells and basophils can both dump their histamine out creating a ton of misery in people! Basophils are implicated in “neuropathic itch” which is discussed below.
The best way to control histamine release is with Cromolyn sodium, a prescription medication. You can ask your physician about a prescription for the oral solution. You take 100 – 200mg two or three times daily and this will stop your cells from dumping out histamine. In my opinion this is one of the most useful prescription treatments we have for itch, and it doesn’t matter if it’s caused from infection or allergies.
FYI, the drug is technically prescribed for other reasons since it helps relieve stomach problems such as diarrhea, pain, nausea/vomiting. But in the context of itch, it is just as helpful and works fast. The nasal spray form of Cromolyn is available over-the-counter as NasalCrom.
Cromolyn is not an antihistamine. It works at the source to block release of histamine, whereas antihistamines block the effect of histamine AFTER you’ve released it. Some people take BOTH Cromolyn and an antihistamine.
IgE (Immunoglobulin E).
Levels of IgE can be measured by taking a blood samples, and in some cases, levels of IgE will be elevated. This is an immunoglobulin associated with immune system challenges that include inflammation such as dermatitis, asthma and recurrent lung infections. People with hayfever will have elevated levels of IgE. Reducing this immunoglobulin will help.
IgE can become elevated with parasitic infections, allergies, chronic lymphocytic leukemia and multiple myeloma. IgE immunoglobulins fit into a receptor (like a key fits into the lock) to mast cells and basophil receptors. That then causes a cascade of inflammatory chemicals to get dumped and results in itchiness, inflammation and other symptoms including bronchospasm. So controlling IgE is something you’d want to do.
Xolair is a drug that does that. This ARTICLE is fascinating and discusses how the “mAb drug” like omalizumab (Xolair®) controls IgE. While helpful, antihistamines are after the fact, the histamine has gotten released and is causing problems so IgE antagonism and reduction is ideal.
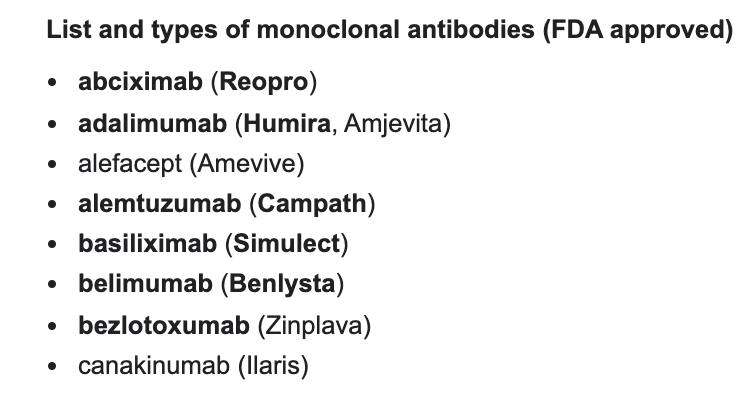
It may cause some serious side effects in sensitive individuals, so it is not a first-line agent in my humble opinion. The mAb drugs is a category of medications that have their chemical names ending with “mab.” And they are so named with the stem “…mab” in order to classify them in the category of monoclonal antibodies which can be shortened to “mab.”
For example, olara-tu-mab refers to a mAb drug that is a monoclonal antibody. These are used for autoimmune conditions and cancer and more.
In addition to Xolair being an anti-IgE drug, there is Cromolyn sodium which I’ve already mentioned above. this drug is also an IgE mediator and helps manage food sensitivities.
An emerging method of controlling mast cells from dumping histamine is by controlling the IgE response. Recent studies show that blocking an enzyme called MAS Related GPR Family Member X2 (MRGPRX2) can help. Drugs that are being tested right now are called “MRGPRX2 antagonists” and one agent is called icatibant (trade name: Firazyr®).
Using this drug for itch is considered an off-label use right now because the drug is actually prescribed for people with hereditary angioedema. MRGPRX2 inhibitors may become more widely accepted in time as more study data comes in.
IL-31 and IL-33 will make itching worse
These are two different proteins that tell your mast cells and basophils to make more pro-inflammatory cytokines like histamine. This will make conditions like atopic dermatitis worse. You don’t want too much IL-31 or 33 hanging around because it will cause more itching, more lesions, drier skin, hard or scaly patches of skin and other discomforts. Blood levels rise in situations like poison ivy, eczema, urticaria, atopic dermatitis and other chronic skin conditions.
As serum levels of IL-31 increase, you see more symptomatology and more discomfort. That’s because IL-31 (and 33) serve as a critical neuron to immune system connection between Th2 cells and sensory nerves which “sense” the itch and then generate the itch sensation. In this case, you feel what’s called a “T cell–mediated” itch. The itch-sensing nerve cells on your skin utilize JAK (janus kinase) to then tell your brain that you have an itch. It’s one bad signal after another!
The JAK Itch
That’s correct – JAK itch, not JOCK itch.
JAK is the abbreviation for Janus Kinase and it has been recently implicated in skin conditions where itch is very prominent. Finding this out has been revolutionary in the field of dermatologist. Who knew this tiny little protein could cause so much suffering for people?! The National Eczema Association posted this ARTICLE about JAK inhibitors and even if you don’t have eczema, I think it’s an excellent read. The drug category of mAbs works well here. Blocking JAK minimizes the sensation of itch.
Employing a mAb drug to block the JAK enzyme is equivalent to unplugging your TV so you don’t hear the bad news. It’s like that – blocking JAK with a mAb drug means you don’t feel the bad itch.
Blockade of the JAK enzyme may help some cases of neuropathic itch. Putting it simply, when you itch, your brain has received a signal via the JAK enzyme to tell you that you itch! So if you block that signal, you control the itch sensation to some extent. The drugs that are useful in this situation include the “mAb” drugs like omalizumab (Xolair). The “mAb” stands for “monoclonal antibody.”
When the cytokines that I discussed above (Il-33 and IL-31) rise (and remain elevated and unchecked), they disrupt your skin barrier. IL-33 and IL-31 trigger activation of the JAK enzyme and cause you to itch. You see this in many acute and chronic itch syndromes including POISON IVY and in atopic dermatitis – ECZEMA (see below for more on eczema).
As for natural JAK inhibitors, Black Seed Oil supplements (a.k.a. Black Cumin Seed) might be useful because this is high in thymoquinone, a natural JAK blocker. In my extensive research over the past week, I was also able to find you this ARTICLE which suggests some Chinese herbs like danshen as natural JAK inhibitors.
The next section of my article outlines specific skin conditions as well as my suggestions for help. Please ask your doctor about what’s right for you as this is not intended as medical advice, just information about options for you and your physician to learn about:

Tinea Versicolor.
This common fungal infection results in discolored patches of skin that are lighter or darker than surrounding skin. It may itch, however the rash is flat and sometimes flaky, but there are no blisters. It may appear anywhere, especially the chest and back.
Possible Treatments for Tinea Versicolor: Since this is caused by a fungus, the first thing that comes to mind is reducing or eliminating refined sugar in your diet. Dietary sugar nourishes fungal organisms. You could rub some coconut oil on the area since that is an easily accessible natural anti-fungal.
If it’s all over, you could take a shower and use a Selenium Sulfide shampoo/body wash (Selsun Blue® 3-in-1). Another option is Nizoral shampoo – some people use it in the shower as a body wash for tinea versicolor. Since this may be drying to your skin, only use it occasionally (with your doctor’s blessing) and follow with hypoallergenic moisturizers.
One more option that comes to mind is a bar of soap that contains Zinc Pyrithione 2% which you can buy online on Amazon or Walmart. DermaHarmony is just one popular brand used for skin conditions. Zinc can be helpful for seborrheic dermatitis, dandruff, and rashes due to psoriasis or eczema.
Kidney Compromise.
Itch is one of the symptoms of kidney dysfunction but I wouldn’t say it’s the first sign. You might see it in a person who has serious, or late-stage kidney problems and it may be associated with edema in the feet or legs. The reason it happens is because your kidneys filter out toxins and waste.
When this effort is compromise, the waste builds up in the blood and causes a severe and deep kind of itch that feels unscratchable. More specifically, with kidney failure, you will see calcium deposits accumulating in small blood vessels of the skin tissue. It’s termed calciphylaxis and it is associated with itchiness.
Possible Treatments for Kidney Itch
This requires a qualified physician and while palliative treatments may help for a few hours, the real treatment may require dialysis, binders and medical interventions.
Hot Tub Folliculitis
This is sometimes also called Pool Folliculitis and the rash can cause itchy, red and tender bumps that hurt. The rash looks visually very similar to bed bug bites, however there is no relationship. You can get hot tub rashes from a swimming pool or whirlpool that looks like it has perfectly, clean water because the causative bacteria Pseudomonas aeruginosa can survive in water that has been chlorinated!

So to avoid infection, the filters of your pool (or hot tub) must be cleaned out or replaced routinely and you need to change your silver ion sanitizer (if applicable). The itchy rash shows up where you had your swimsuit on, usually the torso, or buttocks. It can spread all over your body and may cause fatigue and mild fever.
Kids get this infection frequently, because they like to go to those water slide parks and sometimes the parks don’t keep the pools clean enough. When discerning whether or not you have this condition, keep in mind that if it’s on the palms of your hands for example, it’s NOT hot tub folliculitis simply because you don’t have hair follicles there!
It’s impossible to grow hair on your palms. So you personally can rule in, or rule out certain conditions with common sense.
Possible Treatments for Hot Tub Folliculitis: This is usually a self-limiting condition that begins the day you come into contact with contaminated water. But it’s only self limiting if you know that you got it from your hot tub (or pool), right?! Remember, the water can look sparkly clean and if you swim in it every day, you’re going to keep the itchy rash going on.
But let’s say you were at a hotel and got in the jacuzzi there… by the time you get home a week later, the rash would have likely healed all by itself. If it persists, there are some topical treatments that will help. The first that comes to mind is Silvadene® cream (silver sulfadiazine) which is a prescription cream that is used for people who have minor burns. It does contain “sulfa” in it.
There are other silver-containing creams that are sulfa-free, and these are sold online or at health food stores. I think they could work well too because they contain silver. A popular remedy to apply calamine lotion on the spots. Some people have used compresses of plain distilled vinegar 3 to 4 times a day for 15 minutes.
And finally, if this is severe, see your physician for a prescription to treat it. In very serious cases they will often combine antibiotics such as Cephalexin with gentamicin cream (or even oral gentamicin). In the most severe cases, they could use a fluoroquinolone such as
Ciprofloxacin because those drugs have anti-pseudomonal activity, however the fluoroquinolones would be my last suggestion since they have a Black Box warning by the FDA.
Progesterone Dermatitis
This is an immune-driven condition that causes itchiness in a recurring fashion due to the rise in progesterone with every menstrual cycle.
The skin eruptions occur during the luteal phase when progesterone is highest. It’s essentially an autoimmune reaction to your own hormones! The skin over-reacts to the hormone spike of progesterone that occurs right before your period and the accompanying rash worsens at that time too.
No one is 100% clear about why this happens to some women, but there are many theories including the body’s autoimmune response to seeing progesterone, either the kind that is taken by pill or injection, or the kind that you naturally produce in your body each month.
Most of the time this hormonal type of rash looks similar to eczema and causes red splotches and/or little pustules.There are other ways that autoimmune progesterone dermatitis manifests, for example, a monthly canker sore, or red splotchy rashes. See a hormone specialist to control the surges of progesterone.
Neuropathic Itch
This type of itch is a difficult one to diagnose because there is often no presentation of a rash or redness unless it’s from you scratching it like crazy! There are no blisters or scaly or flaky skin. You might develop issues such as these but it’s secondary to the scratching – the presentation of neuropathic itch is normal, healthy looking skin.
So it becomes your word basically, and nothing to show for it unless you test for Small Fiber Neuorpathy (learn how to test for that HERE). That’s because it is associated with Small Fiber Neuropathy (SFN) and you don’t see anything upon visual inspection with that either! But you will scratch and scratch all over!
The itch will move all around your body at will, and there is no discernible trigger. You can change your shampoo, soap, laundry detergent, bedding and clothing and the itch will stay with you.
Patient: “Doctor, I itch but I don’t see anything!”
Doctor: “I don’t see anything either!”
So where do you go from there? Usually a steroid dose pack and some Benadryl. That’s essentially everyone’s go-to treatment and it may help some conditions but not neuropathic itch.
It’s possible to receive a diagnosis of “idiopathic pruritus” for example, which could be translated as follows “I don’t know why you’re itching, I can’t see any real cause for it, but you’re itching!” People with fibromyalgia commonly experience neuropathic itch quite often – about 40% of patients with that condition likely have SFN. That condition can cause neuropathic itch because the small fibers can’t sense pressure properly anymore.
The reason it’s impossible to see neuropathic itching is that it is a sensory problem. You have nerve cells in your skin that are sensory in nature. They ‘feel’ the itch and the enzyme called Janus Kinase or JAK is what tells your brain that there IS an itch. If JAK is signaling like crazy, you feel an itch. The itch could move around every few seconds.
One way to stop the sensation of the itch is to block JAK. I discussed this above already. The use of JAK inhibitors may be beneficial to patients with neuropathic itch. Again, there would be no associated rash or scaly skin, or pus-filled blisters with neuropathic itch. The itch has no discernable cause.
Doctors have to trust their patients and not dismiss them as a hypochondriac. They need to believe their patients that there IS an itch. Then, and only then will a potential treatment be ordered. Sadly, most people with neuropathic itch are supported on steroids and antihistamines, neither of which work that well!
Possible Treatments for Neuropathic Itch
One of the most promising treatments for neuropathic itch are the JAK inhibitors. (You may also see it written in the literature as JAK-STAT inhibitors). Dermatologists who are well-studied may prescribe a medication such as Xeljanz (tofacitinib), and unlike other medications in its class of JAK inhibitors, Xeljanz is a pill, not an injection.
It is a JAK1 and JAK2 inhibitor and you can learn more about it at this THIS WEBSITE. The FDA-approved use for tofacitinib (Xeljanz) is rheumatoid arthritis, psoriatic arthritis and ulcerative colitis. It has side effects – the FDA has issued warnings about this medication (and others in its category) that it can cause an increased risk of cardiovascular problems and malignancies with use.
If a person with neuropathic itch takes a low dose, they might see dramatic improvements after just a few days with this drug! That could be a miracle for some of you. It does not reduce inflammatory cytokines, it’s strictly to manage itch. One downside is that it suppresses the immune response a little bit. That makes sense because it’s a drug used for autoimmune conditions, so you would expect that. But it can be taken for a short term to give you relief if you have this type of nerve-related itch. There are videos online on Youtube with patient testimonies.
I researched my brain to find a natural JAK inhibitor and I found some! While much weaker than the drug, thymoquinone suppresses JAK! This natural compound is the primary active ingredient in supplements of Nigella Sativa, also known as Black Seed Oil or Black Cumin Seeds. There are many commercial preparations of Black Seed that people take because it’s an antioxidant.
Black Seed Oil Inhibits JAK2 Enzyme

So Black Seed Oil can inhibit the JAK2 enzyme because it is so rich in the JAK inhibitor thymoquinone! Will it work as well as Xeljanz for neuropathic itch? No, it’s an herb, it’s much weaker, however, I think this antioxidant might play a role in supporting skin and helping itch to some extent via inhibition of JAK2.
There is a medical doctor and researcher by the name of Dr. Brian S. Kim who has done ground-breaking research on the topic of neuropathic itch and the use of Xeljanz. Another medication you could try that is an oral JAK inhibitor is called Jakafi (ruxolitinib). This medication comes in 15 and 30 mg dosages. Visit this website for more: https://www.jakafi.com/
This drug has shown tremendous benefits for patients who had terrible itching associated with their condition called polycythemia vera. This is a type of blood cancer. According to one article, the otherwise intractable itch was improved by about 95% in PV patients who were treated with Jakafi, compared to only 2% with standard therapy.
Even if you don’t have PV, you can ask your physician about it. There is a cream formulation of Jakafi coming out soon, it’s in Phase 3 testing. You could apply this to small areas of your skin, but I don’t think it will help as much as the oral tablets if you have a full-body itch.
Topical JAK inhibitors are going to be a new bombshell drug for atopic dermatitis conditions because they do not have the same adverse events associated with steroids, and they work very fast to block the itch sensation via the novel neural-immune connection.
Another category of medications that help with neuropathic itch are the anti-seizure drugs, especially gabapentin and pregabalin.
Fungal Itch
A full-body skin infection that is borne by a fungal pathogen usually appears in the immunocompromised, but not always. Some common, self-limiting fungal infections that you’ve probably heard of include athletes’ foot or a vaginal yeast infection. But what if it’s all over your body? That’s possible too. You might see this in a person who spends a lot of time in the shower, bath, swimming pool, or hot tub. The hallmark feature is the itch but the appearance of the skin rash can vary.
A fungal-based skin infection sometimes has a bright red appearance around the border, but lighter inside. It spreads across a large area like your back or chest. Here’s an interesting ARTICLE that discusses the basophil and mast cell role in allergic fungal disease.
Possible Treatments for Fungal Itch: You could do the Selsun Blue or Nizoral trick, meaning take a shower with the body wash/shampoo that has an anti-fungal in it. Rub it on your itchy legs or wherever the rash is, and then rinse it off in your shower. Try to keep the temperature of the water lukewarm, not hot because the hot water will make you itch more! Pat yourself dry.
In more serious cases, an anti-fungal drug could be used such as Itraconazole or Fluconazole. These are given orally for a period of a week or two, sometimes longer. Another home remedy that might work is the essential oil of the tea tree which you would dilute. Essential oils (EOs) are very useful for skin problems.
Here’s a recipe to make if you want to spray a spot on your body with an essential oil blend that is anti-fungal. Feel free to use any/all of the following EOs. Because dyshidrotic eczema is sometimes associated with mold/fungus please scroll down below to read that section.

Suzy’s Skin-Soothing Itch Relief Formula
A little spray bottle
1/2 cup of water
15 drops lavender essential oil
20 drops tea tree oil
10 drops On Guard®
10 drops Frankincense
Optional: Jojoba oil (about 5ml or 1 tea to the whole spray bottle)
Shake well before each use. Spray as desired on itchy skin.
NOT FOR INTERNAL USE – TOPICAL USE ONLY.
Staph Skin Rash
Sometimes you see this on a baby as diaper rash, but sometimes in adults it can be very dangerous and contagious. It just depends on the type of organism that is causing the infection, it is very commonly Staph aureus. When a person has an oozing blister or boil, think staph. For the most part, the staph infection that is most common is the minor type that is treated with Neosporin for example. This type of minor infection is contracted and spread through a cut or abrasion, or sometimes skin-to-skin contact. Athletes might pick it up by sharing a towel or uniform, or a razor for example.
Possible Treatments for Staph Itch: The most common treatment for mild infections is triple antibiotic ointment like Neosporin. In more serious cases, doctors can prescribe a topical medication called Bactroban® ointment, known generically as mupirocin. This is the gold standard for treatment of staph infections that are methicillin-resistant. On occasion, doctors prescribe antibiotics that help too. There are many to choose from.
Dyshidrotic Eczema Causes Itch
This atopic dermatitis type of rash is characterized by tiny red dots that look like petechiae, but they are not truly petechiae, and these vesicles morph into blisters. You may feel a stinging sensation, similar to the sting that you feel if you get a cold sore on your lip. This minor stinging sensation is the first clue before the breakout. Soon after you may see tiny red spots which are usually 1 to 2 mm in size. These deep seated vesicles appear on the palms, or the lateral aspects of your fingers and/or feet.

Dermatologists should be aware of this pruritic skin reaction to IVIg infusions
As dyshidrotic eczema progresses, it begins to look like tapioca pudding with lots of tiny blisters. But this condition begins on the palms of the hands and/or the feet/ankles. It will sometimes spread all over the body and create a lot of itching which worsens in the evening and more so at bedtime. This condition is driven by an autoimmune reaction in the body, however, it could also be related to taking various medications including IVIG. See my ARTICLE about Small Fiber Neuropathy. IVIG is mentioned in that article, as well as testing procedures.
The gold standard treatment for dyshidrotic eczema is Protopic® a topical ointment known chemically as tacrolimus. Topical tacrolimus is available by prescription and belongs to the drug class of calcineurin inhibitors. Another popular drug in this category is Elidel® Cream, known generically as pimecrolimus.
Eczema is a very complicated condition with many different root causes and potential treatments. It is beyond the scope of my article today, however, I want to let you and physicians reading this about a novel approach to treatment. Block eosinophil infiltration and you might prevent the skin thickening that occurs with this condition.
There is an animal model STUDY that you can read to learn about: Strategies that block eosinophil infiltration, cys-LT production, or the CYSLTR2 might be useful in the treatment of AD. It’s a specific gene (and you may even have an SNP there) that encodes for a protein that makes cysteinyl leukotriene receptors. Reducing inflammation in this pathway would help.

Possible Treatments for Dyshidrotic Eczema: Antihistamines and steroids are the mainstays of treatment but they sadly have a limited role. Interleukin 5 and 18 (IL-5 and IL-18) are high in atopic dermatitis (and eczema) and so for that reason, I recommend Levocetirizine (Xyzal) specifically as one of the potential antihistamines to use for this condition.
A combination of this newer (2nd generation type of antihistamine) with the older 1st generation antihistamines (think of Benadryl or Atarax) work best..
But maybe there’s an even better way?! If you can get yourself a prescription for oral Cromolyn sodium and take 100 – 200mg three times daily it would work very well in a severe, acute case of itching (termed pruritus).
This prevents the dumping of the histamine, whereas antihistamines deal with processing the antihistamine AFTER it has been released from the basophils and mast cells. You could do both for a few days to really make a systemic, non-pathogenic type of itch resolve quickly.
The use of an anti-fungal such as tea tree essential oil, or even oral prescription drugs (Itraconazole) can be helpful in calming down the itch. In some cases, there is a staph component going on (think Bactroban ointment) or a fungal component (think itraconazole or fluconazole).
If you want to spray your legs or feet using essential oils that help with the itch, scroll above to see the “recipe” for my Skin-Soothing Itch Relief Formula (using essential oil) and keep the spray bottle on your nightstand to use in the middle of the night.
Taking a shower with “Selsun Blue Active 3-in-1” and use it like a body wash (and immediately rinse it off). This can bring immediate relief to some people if there’s a fungal component to the rash. The product is widely available and sold as a dandruff shampoo/conditioner/body wash. The anti-fungal activity of selenium sulfide can be very soothing for some skin rashes (but not all). Remember to test yourself in case you’re allergic/sensitive to it.

Applying Clobetasol or Betamethasone ointment can be helpful as well, and you can dilute a wad of those in some Sarna Lotion and spread all over. The real treatment for dyshidrotic eczema however is to find out the specific root cause and address that.
It is not contagious like hot tub folliculitis or scabies. Furthermore, it is not spread by sharing a bath or pool with someone. Eczema appears as an eruption on the outside of your skin, but it is driven by that person’s immune dysfunction which is on the inside.
Mustard seed oil is rather interesting and there are studies to support its use in eczema. I found a product that might help some of you online and bought it to examine it. (I don’t have eczema myself but almost always buy and test things on myself or friends before I write about them here).
It is a strong and unique product that I think plays a role for people with skin/itch syndromes, but please careful and do a test patch first. It’s actually a bath soak called Dr. Singha’s Mustard Seed bath salts and it’s sold online.
You can add a few drops of water to turn it into a thick (but spreadable) paste. I suggest you try applying it to your palms as long as the skin is not broken. And the paste will instantly dry up and harden on your skin within a minute or two. You then rinse it off after about 2 minutes.
As for taking a bath in it, I’m not 100% sure if that is right for you… that is actually what it’s intended for, but again, test yourself to make sure this product makes you feel more comfortable, and that you don’t react to it before you jump in a bath with it. Finally, if you take a bath, keep the water warm, not hot because the heat will make this situation far itchier than it was before!
Miscellaneous Anti-Itch Remedies
Below are other options and ideas for you to consider.
1. Cnidium Fruit Extract.
This product is available on Amazon as a dried powder. It is rich in an ingredient called “osthole” which blocks histamine-related itching. You can take it orally as a dietary supplement, but it’s a powder, so you could also turn it into a paste with some water, and then apply it to a rash topically. This could help with ringworm. You can read the animal STUDY here.
The exact anti-pruritic mechanism of osthole is unknown, we just know it can help in some instances.
2. White Peony Extract.
Peony extract is a potent antioxidant and anti-inflammatory herb, and it can help if you have redness, tingling or itching on the skin. Be aware that as an herb, it could also CAUSE an itch to sensitive people, but again for the most part, people use it on the skin for its soothing benefits. One of the major active constituents in this is called paeoniflori. Peony extracts are sometimes used topically in skin care formulations, but you can also buy a dietary supplement of it, which is sold online.
If you do decide to try this specific herb be aware that it can increase aromatase enzyme, turning your testosterone into estrogen faster. The white peony (paeoniflori) can support liver function too. Keeping your liver functioning well is important.
3. Liver supplements.
If you can take supplements like catalase, glutathione, NAC or CoQ10 (ubiquinol) this may help with itch. When the liver is not functioning well, ot does not perform its filtration job very well. When you can’t clear out toxins and bacterial by-products, or even bile salts, you will itch with more vigor. So detoxification is important and your liver (and kidney) health play a critical role in skin conditions.
4. Calendula Creams
This is an herbal extract that is known to soothe skin and its itchiness. It can be very nice on mild skin rashes. There are many brands available at health food stores for calendula-based creams.
5. Probiotics
There are 3 strains that are known to help improve skin conditions:
L reuteri
L plantarum
L rhamnosus
These can be helpful with acne, eczema and other skin conditions.
6. A diet rich in flavonoids
Eating a diet that is rich in vitamin C and quercetin can be extraordinarily helpful. C is known to help make collagen and quercetin is a natural antihistamine. Fruits with color and citrus fruits will help, and of course, you can consider supplements.
I’ve covered a variety of skin conditions today, and numerous medications and supplements that can ease the situation. I surely hope this article has helped you feel better. If you have read this article and are uncertain about what you should do for your specific situation, please consult your doctor or dermatologist to help you decide upon the proper treatment.
Every person is unique, and your practitioner(s) will know what’s best for your specific condition. The remedies and medications listed above are outlined for educational purposes only, simply to help you learn about more options, and not intended as medical advice.

Suzy Cohen, has been a licensed pharmacist for over 30 years and believes the best approach to chronic illness is a combination of natural medicine and conventional. She founded her own dietary supplement company specializing in custom-formulas, some of which have patents. With a special focus on functional medicine, thyroid health and drug nutrient depletion, Suzy is the author of several related books including Thyroid Healthy, Drug Muggers, Diabetes Without Drugs, and a nationally syndicated column.
