What's On This Page?
ToggleAre you feeling tired, gaining weight, or experiencing mood swings and just not sure why? It could be your thyroid acting up, but is it Hashimoto’s disease or hypothyroidism? Though they sound similar, they’re not the same. Let’s dive into the world of thyroid health to uncover the subtle yet significant differences between these two conditions, shedding light on how your body might be telling you something important through these often confusing signals.
In Hashimoto’s disease, the immune system mistakenly targets the thyroid gland, leading to the gradual destruction of cells responsible for making thyroid hormones. This typically results in hypothyroidism, where the body doesn’t produce enough of these crucial hormones. Hashimoto’s is particularly common in middle-aged women, though it can occur in anyone.
Definitions
- Hypothyroidism is a condition characterized by the thyroid gland’s inability to produce sufficient thyroid hormones, which are crucial for regulating metabolism. When the thyroid underperforms, the body’s processes slow down, leading to symptoms such as fatigue, weight gain, cold intolerance, dry skin, and changes in the menstrual cycle among others. A thyroid nodule or goiter is possible.
- Hashimoto’s Disease, also known as Hashimoto’s thyroiditis and sometimes I refer to it as Hashi’s for ease. Here, the immune system attacks the thyroid gland, gradually ruining its ability to produce thyroid hormones. Levels may swing high and low, but always ultimately (over years) lead to insufficient levels of thyroid hormone (hypothyroidism).It’s marked by the presence of antibodies that target thyroid proteins, reflecting the autoimmune nature of the condition. Hashimoto’s can cause the thyroid to malfunction or shrink, progressively worsening over time. The development of thyroid nodules and goiters is relatively common in individuals with Hashi’s!
- Honorable Mention Thyroid Hormone Syndrome aka Thyroid Resistance: I won’t cover this today in my article, but I want you to know there is a condition called Thyroid Resistance which I covered thoroughly in my Thyroid Healthy book. It’s essentially where your body’s cells become less responsive to thyroid hormones, leading to symptoms of hypothyroidism despite normal or elevated levels of thyroid hormones in the blood!
I wrote about more intricacies regarding each of these conditions in my best-selling book called Thyroid Healthy. It’s available at my SHOP. It’s also available on Amazon.
Fun fact
Hashimoto’s thyroiditis was first described by Japanese physician Hakaru Hashimoto in 1912 in a paper he published while working in Germany. His work described a condition he called “struma lymphomatosa,” which is known today as Hashimoto’s thyroiditis. His discovery was very significant as it was among the first conditions to be recognized as an autoimmune disease, where your body’s immune system attacks its own tissues. Dr. Hashimoto’s observations established the concept of autoimmune disease, a major breakthrough in medical science.
Tests that Differentiate Hashimoto’s from Hypothyroidism
Hashimoto’s thyroiditis and hypothyroidism are often intertwined, and patients as well as doctors have an impossible time telling the difference between them based on symptomatology UNLESS they do a few simple tests. It’s nothing invasive, just a few blood tests to look for antibodies and other biomarkers, sometimes an ultrasound.
The majority of hypothyroid patients also exhibiting signs of Hashimoto’s, which is the autoimmune condition. Although both conditions involve the thyroid gland, they are distinct in their pathology. Underneath this section, I’ve created the 4 best ways to tell the difference between Hashimoto’s and hypothyroidism.

Tests to differentiate between Hashimoto’s and Hypothyroidism:
- Thyroid Peroxidase Antibodies (TPOAb): Elevated levels are often found in Hashimoto’s disease and can indicate the presence of an autoimmune reaction.
- Thyroglobulin Antibodies (TgAb): These antibodies, like TPOAb, are also commonly elevated in Hashimoto’s and help confirm an autoimmune etiology.
- Thyroid Ultrasound: This imaging test can show changes in the thyroid’s structure, such as increased echogenicity and irregularities typical of Hashimoto’s, which are not present in non-autoimmune hypothyroidism.
- Thyroid Function Tests: While both conditions may show similar results in TSH and thyroid hormone levels, the presence of antibodies and ultrasound findings can help clarify the diagnosis.
4 Ways to Differentiate between Hashimoto’s and Hypothyroidism:
- Underlying Cause:
- Hashimoto’s thyroiditis: It is an autoimmune disorder where the body’s immune system attacks the thyroid gland, leading to inflammation and gradual destruction of thyroid tissue.
- Hypothyroidism: It can have various causes, including autoimmune disorders like Hashimoto’s thyroiditis, but it can also result from thyroid surgery, radiation therapy, certain medications, or congenital thyroid defects.
- Thyroid Function Tests:
- Hashimoto’s thyroiditis: Typically, thyroid function tests may show fluctuating levels of thyroid hormones over time. Initially, there might be periods of hyperthyroidism (due to thyroid gland inflammation causing the release of stored hormones) followed by hypothyroidism as the gland becomes depleted.
- Hypothyroidism: Thyroid function tests often show consistently low levels of thyroid hormones (T3 and T4) with elevated levels of thyroid-stimulating hormone (TSH).
- Presence of Autoimmune Markers:
- Hashimoto’s thyroiditis: Blood tests may reveal the presence of specific antibodies such as anti-thyroid peroxidase (anti-TPO) antibodies and anti-thyroglobulin antibodies, indicating an autoimmune attack on the thyroid gland.
- Hypothyroidism: While hypothyroidism can be caused by autoimmune conditions like Hashimoto’s, not all cases are autoimmune, so these specific antibodies may not always be present.
- Symptom Presentation:
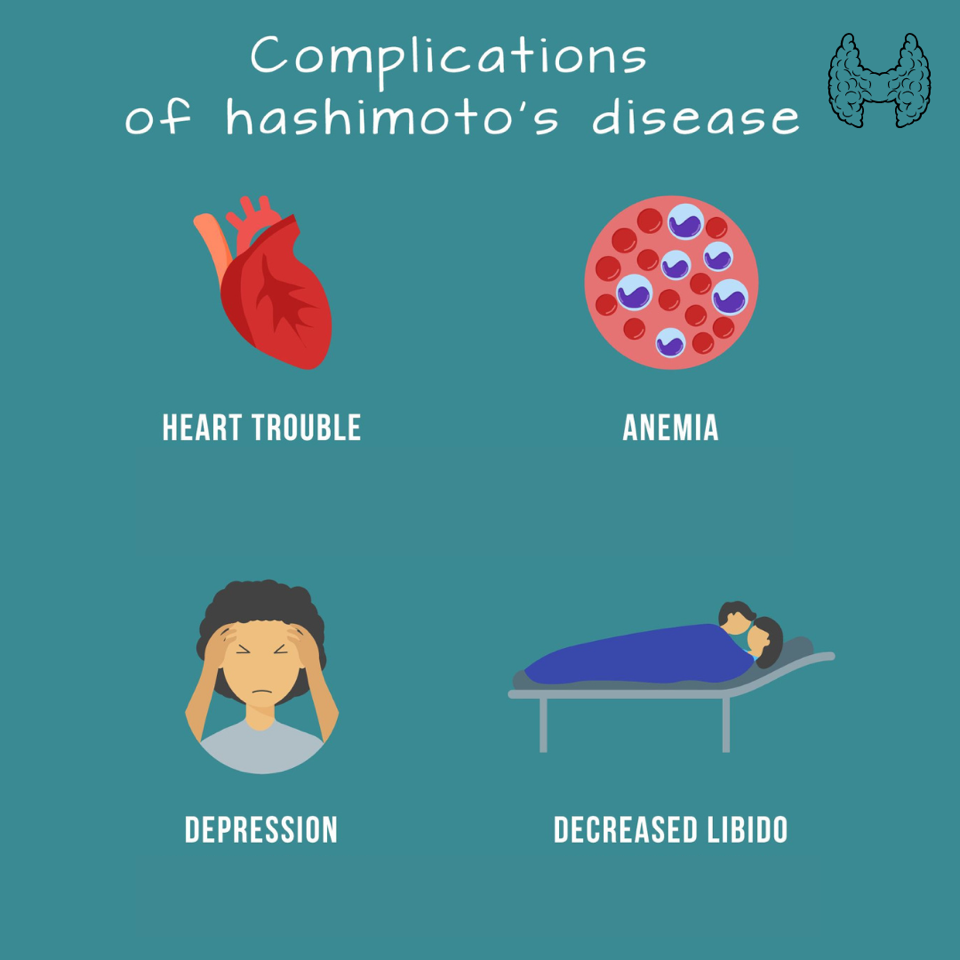
- Hashimoto’s thyroiditis: Symptoms may vary and can include fatigue, weight gain, cold intolerance, depression, muscle weakness, joint pain, and swelling of the thyroid gland (goiter). There may be periods of thyroid hormone fluctuations, leading to symptoms of both hypothyroidism and hyperthyroidism.
- Hypothyroidism: Symptoms typically include fatigue, weight gain, cold intolerance, dry skin, constipation, brittle hair and nails, depression, and muscle weakness. Symptoms may be more consistent and less prone to fluctuations compared to Hashimoto’s thyroiditis.
Treatment Strategies for Hashimoto’s and Hypothyroidism
When treating hypothyroidism, it typically involves thyroid hormone replacement therapy, commonly with levothyroxine (a T4 drug), to normalize hormone levels and alleviate symptoms. Please use my search box to learn more about the way this medication is activated and what to do if you take it.
With Hashimoto’s Disease, it’s critical to think in terms of the whole body which is on fire (as it is with any autoimmune condition). By “fire” I mean that there are elevated cytokines which are pro-inflammatory. While hormone replacement is also used, managing autoimmune activity is crucial. This might include selenium supplements, which have been shown to reduce antibody levels, and ensure optimal levels of vitamin D, iron, and other nutrients that support immune function and thyroid health.
Diet becomes important, and the avoidance of allergens, high histamine foods and dairy as well as gluten. There’s a free ebook below, you can click on the image. Also, I have ebooks available for free on these topics if you’d like them. Just email us, customerservice@suzycohen.com if you want one of those.
The Role of Iodine and Supplements in Hashimoto’s and Hypothyroidism
Iodine plays a complex role in thyroid health. While essential for thyroid hormone production, excessive iodine intake can exacerbate Hashimoto’s by increasing the antigenicity of thyroglobulin and thyroid peroxidase, potentially worsening the autoimmune attack. In hypothyroidism caused by iodine deficiency, iodine supplementation is beneficial and necessary. However, in areas with sufficient or excess dietary iodine, adding more iodine can sometimes lead to complications.

Vitamin D is essential for immune regulation and may be particularly beneficial for both condition, and especially those with Hashimoto’s disease. And omega-3 fatty acids can help reduce inflammation and support hormonal balance in both conditions. Additionally, magnesium plays a role in the production of T4 and can aid in managing symptoms such as muscle cramps or sleep disturbances for people with both conditions.
Can Drug Nutrient Depletion Cause Thyroid Diseases?
Certain medications can deplete nutrients important for thyroid function, such as lithium, which can cause hypothyroidism by affecting hormone synthesis, or amiodarone, which impacts iodine metabolism. Regular monitoring and possible supplementation can mitigate these effects, highlighting the importance of personalized treatment plans based upon your labs, symptoms and medication history.
Potential Triggers of Hashimoto’s and Hypothyroidism
Environmental toxins such as perchlorates and heavy metals can impair thyroid function. Genetic factors also play a significant role, as a family history of thyroid disorders increases the likelihood of developing these conditions. Additionally, certain viral or bacterial infections can trigger autoimmune responses against the thyroid gland, potentially leading to Hashimoto’s or hypothyroidism.
Innovative Therapeutic Approaches to Explore
Some studies suggest that Low-Dose Naltrexone (LDN) can help modulate the immune system, which might benefit those with autoimmune thyroiditis. I wrote an article about The 7 Benefits of Low Dose Naltrexone.
A gluten-free diet can also be beneficial for some people with Hashimoto’s, and even better is a gluten and dairy free diet, but that may feel like a big ask! But reducing these allergenic proteins will help reduce autoimmune inflammation.
You may want to take 5 or 6 minutes to read the 8 Best Strategies to Reduce Histamine and Ease Hashimoto’s, and All Other Autoimmune Diseases.
In the early days of treating Hashimoto’s thyroiditis, options were quite limited and, by today’s standards, might seem a bit rough around the edges. Before the advent of synthetic hormones, treatments primarily included surgery to remove part or all of the thyroid gland in severe cases.
This was often the go-to solution when thyroid enlargement or other complications interfered significantly with a patient’s health. Additionally, iodine therapy was commonly used once it was understood that iodine played a crucial role in thyroid health, though it wasn’t always effective for autoimmune-related issues.
Another historical treatment involved using desiccated thyroid extracts derived from animal thyroid glands. These treatments aimed to manage symptoms by attempting to restore some balance to thyroid hormone levels, but they lacked the precision and efficacy of today’s thyroid hormone replacements. As science advanced, so did our approach, leading to the more targeted and less invasive treatments we have now, like synthetic levothyroxine, which precisely addresses hormone deficiencies with far greater success and comfort for the patient.
Summary
Hypothyroidism refers to a clinical state characterized by insufficient levels of thyroid hormone, which can arise due to various causes including iodine deficiency, surgical removal of the thyroid, or excessive use of thyroid-suppressing medications. In contrast, Hashimoto’s involves an autoimmune process where the body mistakenly attacks its own thyroid tissue, leading to fluctuations of thyroid hormone until chronic thyroid damage causes hypothyroidism.
Understanding the interplay between Hashimoto’s and hypothyroidism is key to managing these conditions effectively. When visiting your healthcare practitioner, keep a symptom diary and share detailed notes about your condition. Always ask for explanations regarding any tests or treatments recommended to better understand how they will help manage your condition.
It’s okay to ask questions, and take quick notes so you don’t forget. Discuss any concerns openly, whether they are about medication side effects or lifestyle changes, to help tailor your treatment plan more effectively. With proper testing, early diagnosis, and informed treatment strategies, you can achieve better health outcomes and potentially mitigate the progression of thyroid disease.

Suzy Cohen, has been a licensed pharmacist for over 30 years and believes the best approach to chronic illness is a combination of natural medicine and conventional. She founded her own dietary supplement company specializing in custom-formulas, some of which have patents. With a special focus on functional medicine, thyroid health and drug nutrient depletion, Suzy is the author of several related books including Thyroid Healthy, Drug Muggers, Diabetes Without Drugs, and a nationally syndicated column.