What's On This Page?
ToggleFor millions of people, acid reflux and heartburn are daily struggles. Some take over-the-counter medications like antacids or proton pump inhibitors (PPIs), while others turn to diet changes and natural remedies to ease discomfort. But what happens when reflux isn’t just heartburn?
What if it’s also affecting breathing, exercise tolerance, and overall quality of life?
Many people with gastroesophageal reflux disease (GERD) or a hiatal hernia experience unexplained shortness of breath (SOB), dizziness, or fatigue during workouts, yet few realize there’s a direct connection between these digestive disorders and the ability to breathe deeply and efficiently. If you have an interest in asthma and wheezing, read my other article: Breathe Easy: Understanding Prescribed Asthma Medications.
I highly recommend you take a few minutes to read my other article if you have SOB: Revealing 15 Hidden Causes of Shortness of Breath and How to Overcome Them.
This article explores how a small hiatal hernia or chronic reflux can impair lung function, impact the vagus nerve, and contribute to exercise intolerance, as well as the potential role of the TIF procedure (Transoral Incisionless Fundoplication) or LINX® in restoring normal function. All of that is below.
If you have an interest in other gastrointestinal issues like SIBO, heartburn or gastrin, betaine with pepsin (which helps thyroid function), use my search box to find relevant articles that I’ve written. In the meantime, here is a graphic to show you some of the symptoms of GERD.
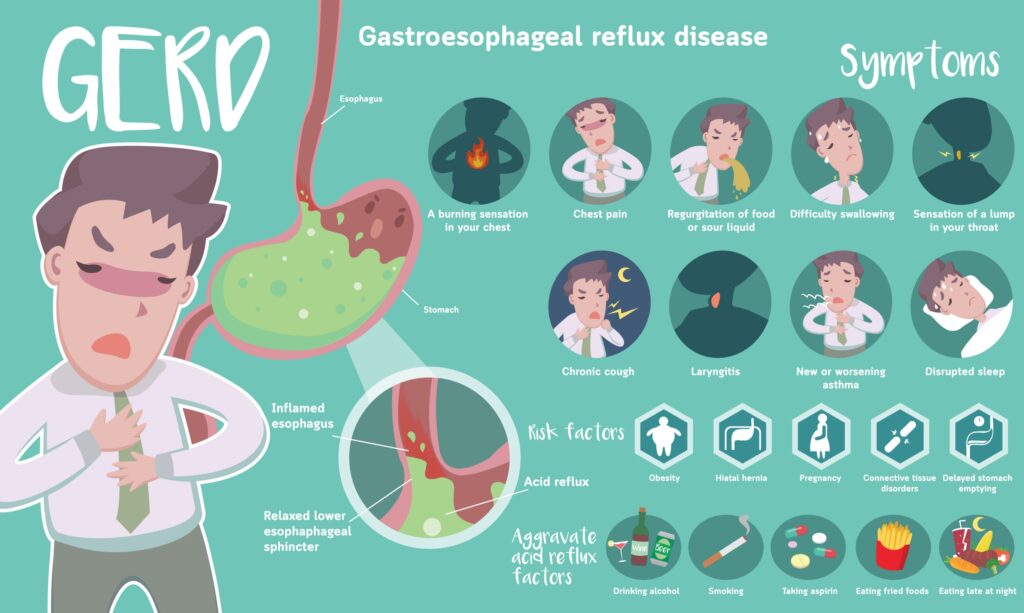 Now one more thing, do not let your reflux go on for a long time. The acid that refluxes upwards is very caustic. It will ruin your esophagus and increase risk for esophageal cancer which is VERY HARD to treat. Make sure that no matter what you do, whether it’s dietary changes, or medications, a procedure, reduction of stress… whatever you do, take care of yourself because this should not go on for years like it does for many people.
Now one more thing, do not let your reflux go on for a long time. The acid that refluxes upwards is very caustic. It will ruin your esophagus and increase risk for esophageal cancer which is VERY HARD to treat. Make sure that no matter what you do, whether it’s dietary changes, or medications, a procedure, reduction of stress… whatever you do, take care of yourself because this should not go on for years like it does for many people.

When Acid Reflux Affects More Than Just Digestion
Reflux occurs when stomach acid flows back into the esophagus due to a weakened lower esophageal sphincter (LES). A small hiatal hernia—when part of the stomach pushes through the diaphragm, can make this worse by altering the natural pressure balance between the stomach and the chest.
Most people associate GERD with heartburn, regurgitation, or bloating, but symptoms can extend far beyond the digestive system. Many experience shortness of breath, chest tightness, difficulty swallowing, and even exercise intolerance.
Why does this happen? It turns out that a combination of diaphragm compression, vagus nerve irritation, and airway inflammation can create a sensation of air hunger, rapid fatigue, or difficulty catching one’s breath during physical activity.
The Vagus Nerve, the Diaphragm, and Their Role in Breathing
The vagus nerve plays a vital role in digestion, heart rate, and respiratory control. This long cranial nerve runs from the brainstem, down the throat, and into the abdomen, passing through the diaphragm near the esophagus. 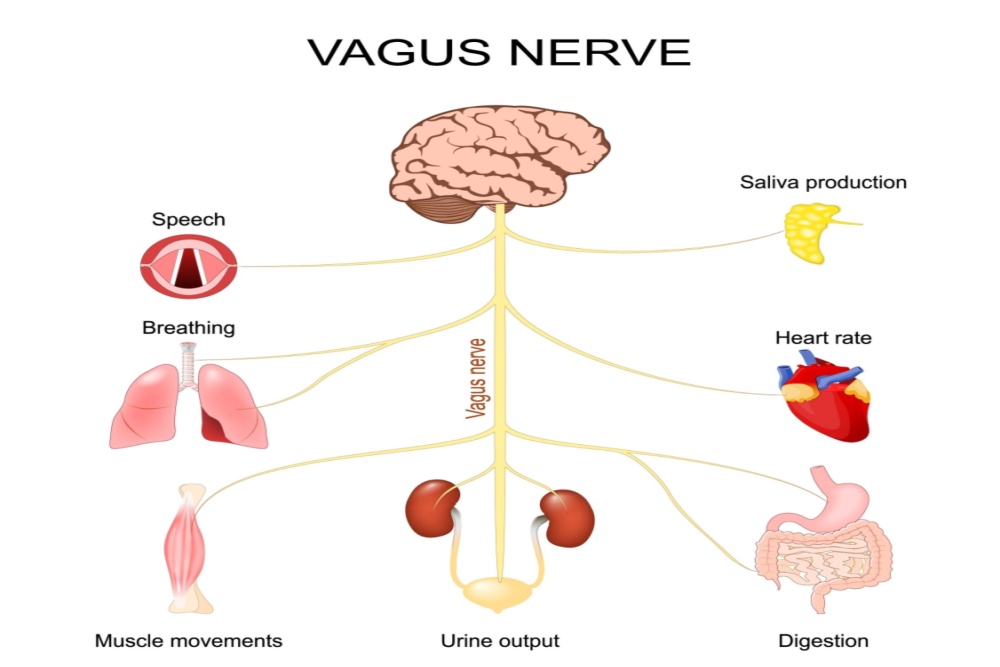
When a hiatal hernia pushes the stomach upward, or chronic reflux leads to inflammation near the esophagus, the vagus nerve can become irritated. This can lead to:
- Breathing difficulties (feeling like you can’t take a full breath)
- Heart palpitations or a “fluttering” sensation
- Mild dizziness or lightheadedness during exertion
- Air hunger (feeling like you need more oxygen, even at rest)
- Increased anxiety around meals or exercise
People experiencing these symptoms (ie related to hiatal hernia with reflux) sometimes undergo extensive cardiac and pulmonary testing, only to be told their heart and lungs are normal. It’s an expensive but true reality. The real culprit? Your nervous system’s misfiring due to stomach dysfunction and it’s not your heart.
Shortness of Breath + Exercise Intolerance: The Hidden Impact of GERD & Hiatal Hernias
For those who experience exercise intolerance, the problem isn’t necessarily weak lungs or poor cardiovascular fitness—it’s the mechanical restriction caused by a hiatal hernia or reflux-related inflammation.
During activities like running, cycling, zumba, jui jitsu, or other high-energy workouts like Orangetheory®, the diaphragm needs full and complete mobility to expand your lungs. So when the stomach is pushing against the diaphragm, deep breathing becomes difficult. This may explain why some people have a hard time catching their breath and exercising at full capacity – it feels like your heart’s not complying with you, but in this particular scenario, it’s actually your lungs. It can increase your pulse and cause all kinds of problems inside causing you to have exercise intolerance.
Why Does Pulse Spike in This Situation (During Exercise)?
Ok, let me preface this with I’m not a cardiologist, this is just a high-level view of what might be going on in the situation of a person exercising while having hiatal hernia and moderate to severe reflux issues.There are five main reasons it occurs:
- Vagus Nerve Irritation (Autonomic Nervous System Response)
Your vagus nerve controls digestion, heart rate, and breathing. This is a very important nerve that gets no attention, until something goes awry. When a hiatal hernia presses on the diaphragm (or in the case of reflux, when stomach acid triggers esophageal irritation), it can send faulty signals to the vagus nerve. Take a look at my graphic below to see everything that the vagus nerve impacts in your body. It’s utterly astounding, and yet we only hear about this special nerve infrequently. I can assure you it is 100% involved in severe GERD and hiatal hernia, that’s why irritation of the nerve causes weird/odd symptoms that can be misdiagnosed.
Vagus nerve irritation leads to:
- Heart palpitations or a fast pulse
- Feeling anxious or jittery (even without stress)
- Sudden heart rate spikes after eating or bending over
- Itchiness, especially in the torso
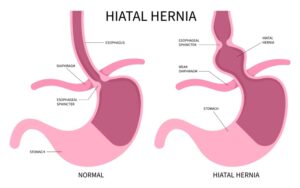
- Diaphragm Dysfunction (Oxygen Demand Increases)
The diaphragm is compressed by the hernia, limiting lung expansion. If less oxygen is reaching your blood, the heart has to pump faster to compensate. This explains the spike. Exercise intolerance (like struggling with aerobic exercise) is a result of this diaphragmatic dysfunction.
- Reflux-Triggered Adrenal Response (“Fight-or-Flight”)
When acid refluxes upwards and constantly irritates the esophagus, your body mistakes it for a threat and releases stress hormones like adrenaline. It puts you into sympathetic overdrive.
It’s not a huge amount of adrenaline (aka norepinephrine), but it’s certainly enough to cause a noticeable spike in your pulse. If you have a health wearable (ie FitBit or Apple Watch) you can see this in real-time as your doing Body Combat® or on the treadmill or whatever.
- The result of sympathetic overdrive:
- Increased heart rate
- Feeling of breathlessness
- Sweating or mild dizziness
- Low Blood Oxygen from Airway Irritation (LPR & Silent Reflux)
If acid reaches the upper esophagus, it can cause laryngopharyngeal reflux (LPR). You won’t notice this if it’s a one-time thing like after over-eating a big bean burrito. But if the LPR is constant and chronic you’ll see problems:
- Silent reflux can lead to:
- Coughing, throat clearing, or tightness
- Swelling of the airway, making breathing feel harder
- Heart rate rising (tachycardia/fast pulse) as your body tries to compensate
- Acid Reflux at Night (Nocturnal GERD Can Trigger Tachycardia)
Don’t eat dinner and then lie down right away. Sit up for about 2 hours, preferably 3 hours. Let’s talk about bedtime now. What if you’re asleep (and you sat up like I just suggested, but you still get GERD?) It’s called nocturnal GERD. Lying flat allows stomach acid to travel higher up than if you were sleeping on an incline. This stimulates your vagus nerve and causing an increased heart rate.
- Some people wake up with:
- Pounding heart rate
- Chest discomfort or a racing pulse
- Shortness of breath
When acid and pepsin (a digestive enzyme) reflux past the esophagus into the throat, they can irritate and inflame the vocal cords, larynx, and surrounding tissues. Pepsin is especially damaging because it breaks down proteins in your throat, just like it does to food that reaches your stomach. So the pepsin starts breaking you down! This can lead to symptoms such as hoarseness, chronic throat clearing, sore throat, and a “lump” feeling (globus).
⚠️ See a doctor if you experience:
- Heart rate spikes above 120 bpm for no reason
- Chest pain, dizziness, or fainting
- Irregular heartbeats or skipped beats
- You develop hoarseness or a sensation of something in your throat
A Word About Silent Reflux
Additionally, stomach acid can spill into the upper airway (a condition called laryngopharyngeal reflux or LPR), leading to these four symptoms:
- A sensation of tightness in the throat or a globus
- A chronic cough or throat-clearing
- Postnasal drip or hoarseness
- A burning sensation in the upper chest, throat, or mouth (different than BURNING MOUTH SYNDROME which I’ve talked about).
Over time, the inability to take deep, full breaths can create fatigue, dizziness, and shortness of breath during exertion.
TIF: A Minimally Invasive Solution for Reflux and Hiatal Hernia Repair
For those whose medications, diet, and natural remedies aren’t enough, there’s an endoscopic, incision-free procedure called Transoral Incisionless Fundoplication (TIF). You’ll have to ask your gastroenterologist or surgeon about this procedure for more details. To do it, they have to give you general anesthesia and the procedure takes about 45 minutes. It’s a same-day procedure, and non-invasive, meaning no knives or cuts into the belly!
TIF restores function to the lower esophageal sphincter (LES) without the need for abdominal surgery. It is performed through the mouth using an endoscopic device, which folds part of the stomach around the esophagus to create a brand new anti-reflux valve.
Additionally, small hiatal hernias (under 2 cm) can be repositioned during the TIF procedure, helping to relieve the mechanical compression on the diaphragm. For those with larger hernias, a laparoscopic hiatal hernia repair may be done before TIF to fully correct the issue. Again, you have to ask a doctor about all of this, but the good news is that for most people today, they can do a TIF procedure where no knives are involved, as in scalpels… just general anesthesia for a short period of time. The LINX® procedure does require a few minor incisions, but it’s very quick. I’ll discuss it next. Recovery time for these procedures takes a few hours and you go home, then the process is a special diet of liquid/soft foods for a while.
Research shows that TIF significantly reduces GERD symptoms and improves quality of life for patients suffering from chronic reflux. You can read more about the study in this PAPER.
LINX: Another ‘Less Invasive’ Solution
The LINX® procedure is a minimally invasive surgical solution for GERD, designed to strengthen the lower esophageal sphincter (LES) and prevent acid reflux. It involves placing a small, flexible ring of magnetic titanium beads around your LES reinforcing the valve’s ability to stay closed when you’re not swallowing. This means less acid refluxing upward (which is a good thing).
In case you’re wondering LINX® doesn’t stand for anything, it’s just the trade name for the procedure.
The magnets provide just enough pressure to keep stomach acid from rising while still allowing food and liquids to pass through when needed. Since the procedure is performed laparoscopically, it requires only a few small incisions, making recovery quicker and less invasive than traditional anti-reflux surgeries. Most patients return home the same day and resume normal activities within a week.
Clinical studies show that LINX® is highly effective, with 85-90% of patients experiencing significant reflux relief and reducing or stopping PPI use. That is a good thing so taking PPIs long-term can cause a host of side effects, and via the drug mugger effect, several new diseases! The body doesn’t do well long-term if you have to live on those drugs, so something like LINX is a more permanent solution.
Unlike Nissen Fundoplication (a procedure not discussed here, but used by some surgeons) which wraps part of the stomach around the esophagus, LINX preserves normal physiological function, meaning you can still burp and vomit if you ever need to. That’s a huge advancement because sometimes people just need to throw up and obviously burp! These two simple things that we take for granted are something that’s often restricted after fundoplication procedures. So the LINX is a step up in this regard, however there is a downside.
The most common side effect to LINX is temporary difficulty swallowing, but this usually resolves within a few weeks as the body adjusts. Another downside is that people with a large hiatal hernia (>3 cm) may need hernia repair FIRST. I think the biggest downside is that if you get a LINX procedure, you can’t get an MRI in those older machines for about 3 years. Newer devices are MRI-safe up to 1.5T or 3.0T, older models can pose a risk in high-powered machines.
This may not sound like a big deal, but imagine a traumatic injury where an MRI is needed. Or imagine a woman with breast cancer who needs an MRI periodically… there are many instances where an MRI of this part of your body is needed.
If you anticipate needing frequent MRIs for other health conditions, the LINX could be a drawback, or contraindicated. You can read more here about LINX at the Duke Health WEBSITE.
Theoretical Symptom-Management Plan (Not Medical Advice!)
For those managing GERD and a small (< 2cm) hiatal hernia while waiting for proper treatment, let me share a basic plan that you can use until you get your procedure. This is opinion-based so run everything by your own doctor. It’s a combination of dietary modifications, medications, and natural supplements that may help reduce symptoms. This regimen won’t negate the need for a procedure, but might help.
Dietary Adjustments
- Eat low-acid, high-fiber foods like oatmeal, bananas, sweet potatoes, and lean proteins
- Avoid caffeine, citrus, tomatoes, alcohol, and carbonated drinks
- Avoid black coffee
- Eat small, frequent meals to prevent stomach distension
- Avoid eating at least 3 hours before exercise or bedtime
- Avoid spicy condiments and foods
Supplements and Natural Remedies
- DGL Licorice (before meals) to soothe the esophageal lining.
- Aloe vera juice to reduce inflammation
- Slippery elm or marshmallow root tea (or non-alcoholic extract/supplement/lozenge- to coat and protect the throat).
- “Zinc carnosine” capsules to support the stomach lining (this is not the same as chelated zinc).
- Try coating your stomach with alginates, one good product is on Amazon called “Reflux Gourmet” in Vanilla Caramel. Take it about 30 minutes after your meal. (If you’re taking zinc carnosine too, you should take that supplement immediately after eating, wait 30 minutes and then take the Reflux Gourmet). One more thing, this product (alginate products) cause a “raft effect” and this might not work properly in some people. So this alginate products like this can backfire making reflux much worse in some people, so it’s not right for everyone. If you try it, start low and go slow. Don’t take it if your stomach is too empty, or too full and if you do get a bad reaction, slowly sip 8 oz of water that has about 1/8 or 1/4 tea baking soda in it to alkalize the esophagus.
Medications (If Needed, Under Medical Supervision)
- Gaviscon Advance Aniseed Flavor for immediate symptom relief (for some of you). It contains 1000 mg sodium alginate and 200 mg potassium hydrogen carbonate You take this product after meals. It’s similar to Reflux Gourmet Vanilla Caramel, however it contains peppermint so I don’t usually recommend it because mint makes reflux worse. I am listing it here for completeness. Also, let me repeat this part: This product (alginate products) can backfire making reflux much worse in some people, so it’s not right for everyone. If you try it, start low and go slow. See above in red for more tips.
- Pepcid (H2 blocker) for reducing acid at night, for example Pepcid® (famotidine). Don’t take this if you already take a PPI like omeprazole. It’s one or the other. Pepcid is sold OTC as 10mg per tablet. It’s available in higher doses by prescription.
- Proton pump inhibitors (PPIs) if symptoms are severe (but long-term use should be monitored). These are now sold OTC as omeprazole and esomeprazole.
- Sucralfate (Carafate®) for esophageal healing – this medication requires a prescription.
Final Thoughts
For those struggling with exercise intolerance, shortness of breath, or unexplained fatigue, GERD or a hiatal hernia may be playing a larger role than expected. While diet and natural remedies can help, some cases may require medical intervention, such as the TIF procedure.
Understanding the vagus nerve connection and how reflux impacts breathing can help patients advocate for the right treatment. If symptoms persist despite lifestyle changes, it may be time to explore minimally invasive options like TIF to restore normal function and improve quality of life.

Suzy Cohen, has been a licensed pharmacist for over 30 years and believes the best approach to chronic illness is a combination of natural medicine and conventional. She founded her own dietary supplement company specializing in custom-formulas, some of which have patents. With a special focus on functional medicine, thyroid health and drug nutrient depletion, Suzy is the author of several related books including Thyroid Healthy, Drug Muggers, Diabetes Without Drugs, and a nationally syndicated column.