What's On This Page?
ToggleMelatonin might be the most misunderstood supplement on the planet. People pop it right before bed, take huge doses, wake up groggy at 3 a.m., and conclude, “Melatonin doesn’t work for me.”
The truth is simpler, and way more frustrating: Melatonin usually isn’t failing. It’s being mistimed. You’re probably taking it at the wrong time.
Even as a pharmacist, I’ll admit this isn’t taught well. And it matters, because melatonin isn’t a sleeping pill. It’s a timing hormone. Let’s fix the confusion.
What Melatonin Actually Does (And What It Doesn’t)
Melatonin does not knock you out.
It doesn’t sedate you.
It doesn’t force sleep.
Melatonin’s job is to tell your brain, “Night is starting now.”
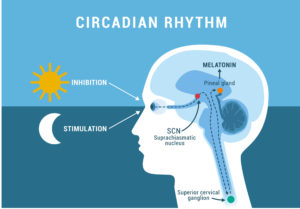
That’s it. It shifts your circadian rhythm, the internal clock that controls:
- Sleep timing
- Body temperature
- Cortisol rhythm
- Growth hormone release
- Immune signaling – If you send that signal too late — or too strong — things get messy.
The Biggest Melatonin Mistake
Most people take melatonin at bedtime. But that’s like turning the porch light on after you’re already inside the house. For most adults, melatonin works best when taken 2 or even 3 hours before your natural bedtime. For many people, that’s around 6:30, 7:30, or maybe even 8:00 pm, certainly not 11 pm or midnight which is when a lot of people take their melatonin. When it’s taken earlier, melatonin advances your sleep clock. In other words, taken late, it can fragment sleep and cause early-morning awakenings like at 4 am. Ironic, isn’t it?
As Dr. Alfred Lewy, a pioneer in circadian biology, has shown, “Light suppresses melatonin secretion in humans and affects circadian rhythms in humans,” underscoring that melatonin’s role is tied to the body’s internal clock more than simple sedation.
Dosing It: Less Is Almost Always Better
This part surprises people. Your brain naturally makes about 0.1 – 0.3 mg of melatonin per night. Yet store shelves are packed with 3 mg, 5 mg, even 10 mg pills.
That’s excessive for most people (unless you’re treating specific neurological conditions like cluster headaches — a topic I cover in Headache Free). For typical sleep support, 0.3–1 mg is usually plenty, and often perfect. Higher doses don’t work better. They just create more side effects that people don’t always realize are coming from melatonin. This is why I only put 1 mg of melatonin in Sleep Script, a product that is one of my best sellers for rest and tranquility.*
Why Taking Melatonin Too Late Can Backfire
When taken too late at night (for example, right when you crawl into bed), melatonin can:
- Disrupt natural sleep cycles
- Interfere with REM sleep
- Trigger awakenings around 2–4 am
- Confuse the brain’s “morning shut-off” signal
- Have you dragging all afternoon but wide awake at midnight because your internal clock is off
This is especially true in people with long-standing insomnia, anxiety, panic disorders, ADHD, migraines, or habitual early-morning waking. In these cases, earlier timing and lower doses matter even more.

Melatonin Interactions: What You Need to Know
I’ll put on my white pharmacy coat now. Melatonin is sold over-the-counter, but it’s still a hormone. It influences circadian rhythm (a system essential for survival) so it deserves respect.
Be cautious if you take any of these medications:
- Sedatives or sleep medications (benzodiazepines, zolpidem, etc.)
- Gabapentin or pregabalin
- Opioids (codeine, oxycodone, hydrocodone)
- Blood pressure medications (melatonin can slightly lower BP)
- SSRIs (such as citalopram), which can alter the body’s natural melatonin rhythm
Melatonin can enhance sedation, especially at higher doses or when taken too late. That’s exactly why people assume more is better, but excessive sedation doesn’t equal better sleep architecture. In fact, it often leads to fragmented sleep, less REM, and early awakenings, which feels like insomnia wearing a disguise. So again, higher doses or taken too late in the evening, it can do these three awful things:
- Fragment your sleep
The brain cycles between sleep stages based on tightly timed hormone signals. Overshooting melatonin disrupts that rhythm, leading to lighter sleep and more awakenings. Think tossing and turning. - Reduce REM sleep
Excess melatonin can suppress REM, particularly in the second half of the night when your REM should naturally increase. People then wake feeling unrested despite “sleeping.” - Trigger early awakenings
After an exaggerated melatonin peak, levels can fall abruptly, or cortisol can rebound too early. Either way, the brain flips into wake mode around 2 to 4 am.
A couple of other things I want to say. Melatonin can worsen depression in a small subset of people (not everyone), but mainly in those who have the wintertime blues, SAD, (as in seasonal affective disorder), bipolar tendencies, or altered serotonin signaling.
It can also intensify your dreams — making them sometimes vivid, sometimes cinematic, and occasionally weird enough to deserve a screenplay.
Melatonin shouldn’t be used as a middle-of-the-night rescue pill. It’s more about timing, not instant sedation.
What About Extended-Release Melatonin?
Extended-release melatonin is marketed as “all-night support,” but that doesn’t mean it’s right for everyone. These formulations slowly release melatonin over several hours, which can be helpful in very specific situations:
Older adults who produce less melatonin naturally. This can be evaluated using a DUTCH Complete test, which measures a urinary melatonin metabolite called 6-sulfatoxymelatonin, (6-OHMS) or with a blood melatonin test which you can do but it’s drawn at night (hard to do).
People who fall asleep easily but wake too early. In these cases, the issue isn’t sleep onset (also called sleep initiation), it’s maintaining adequate melatonin levels through the early morning hours. This is different from taking melatonin too late, which pushes the signal at the wrong time entirely.
For most people, however, extended-release melatonin lingers too long, causing morning grogginess, fatigue, or fragmented sleep.
That’s why most adults do better with low-dose, immediate-release melatonin, especially when combined with calming botanicals. This is exactly why I formulated Sleep Script — to support sleep without overpowering the brain’s timing system.
Special Section: Night-Shift Workers
Night-shift workers are a different situation entirely. The rule here is simple: melatonin must match your biological night, not the clock.
For night-shift workers:
- Take melatonin before daytime sleep
- Usually 30–60 minutes before bed
- Take low doses (like bottles that contain supplement with 0.3–1 mg per dose)
Light exposure matters even more. Wear sunglasses on the drive home. Keep the bedroom dark and cool. Avoid sunlight (pull down the shades) or bright indoor lighting once melatonin is on board.
For shift workers, melatonin isn’t about perfect sleep. It’s about damage control. By that I mean protect your circadian rhythm as much as possible. That’s because chronic circadian disruption has been studied. Researchers find that chronic night shift work (or circadian disruption of any sort) increases the risk of metabolic disease, cardiovascular problems, and mood disorders and more. And it’s all linked to a flipped biological clock.
When Melatonin Is NOT the Right Tool
Melatonin is often overused in people whose real problem is nervous system hyperarousal — high adrenaline, excess nighttime cortisol, or genetic patterns or SNPs involving DBH or COMT enzymes.
Another common issue is conditioned insomnia, where the brain has learned to wake at the same early hour night after night due to stress, anticipation, or past sleep disruption.
In these cases, calming the nervous system matters more than shifting the clock. Melatonin might help, I don’t want to talk you out of it, but it isn’t the whole answer. Something else that could help is bright light – not the blue kind you get from your phone or TV though.
The Missing Half of the Equation: Morning Light Therapy (Yes, the Bright Kind)
Your circadian rhythm needs two clear signals, darkness at night and brightness in the morning. If melatonin tells your brain when night begins, then morning light tells your brain when day starts. You actually need both signals working together for your internal clock to behave properly.
This is where 10,000-lux light therapy comes in. It’s one of the most underused — and misunderstood — tools for sleep problems, even though it’s remarkably effective when used correctly.
Bright light in the morning sends a powerful message to the brain. It suppresses leftover melatonin, anchors your circadian rhythm, and strengthens the contrast between day and night. Over time, this helps prevent early-morning awakenings and improves sleep the following night — not instantly, but reliably. While light therapy can improve mood, its real purpose here is biological: retraining your internal clock.
Timing matters just as much with light as it does with melatonin. For most people, the light should be used within 30 to 60 minutes of waking, and earlier is better than later. Consistency matters more than perfection. If you wake at 6:30 a.m., aim for around 7. If you wake at 8, use it shortly after. What you want to avoid is bright light later in the day, which can delay sleep. This is strictly a morning tool. In terms of dosage, the standard recommendation is 10,000 lux for about 20 to 30 minutes. Your eyes should be open, but there’s no need to stare directly at the light. You can read, eat breakfast, drink coffee, or scroll your phone — just keep the light angled toward your face so it reaches your eyes.
This approach is especially helpful for people who routinely wake between 2 and 4 am. Early-morning awakenings are often a sign of a weak circadian anchor, where the brain doesn’t clearly distinguish night from day. Morning light gently pushes the clock earlier, reduces that slow nighttime cortisol creep, and helps melatonin shut off more cleanly in the morning. Paradoxically, that cleaner shut-off allows melatonin to rise more naturally the next evening.
Strong mornings create better nights – that’s the rule.
When paired correctly, light therapy and melatonin work beautifully together. Morning light strengthens your circadian anchor, while evening dimming of lights and screens prepares the brain for rest. If melatonin is needed, it works best in low doses taken earlier in the evening. Using melatonin without morning light is like setting an alarm clock but never winding it back up. Most people tolerate light therapy well, but some caution is warranted. People with bipolar disorder, light-triggered migraines, or certain retinal conditions should be careful. If light causes agitation or headaches, the fix is usually simple: shorten the session, move the light farther away, or build up gradually.
The bigger picture is this: many people keep increasing their melatonin dose when sleep doesn’t improve. What they actually need is less melatonin, earlier melatonin, and more morning light.
This isn’t about forcing sleep.
It’s about restoring rhythm.
The Simple Takeaway
Melatonin isn’t a sleeping pill. It’s a timing signal.
Your brain naturally makes a tiny amount, it’s only about 0.1–0.3 mg of melatonin each night, yet most supplements and commercial formulas contain 10–100 times that amount! I personally don’t think that’s good for you (unless you have cluster headaches where huge doses are prescribed). That mismatch explains why higher doses of melatonin lead to restless sleep, bizarre dreams sometimes, headaches, or morning brain fog, also that wired-but-tired feeling — especially when taken too late.
If melatonin hasn’t worked for you, it may not be the supplement that’s wrong.
It’s usually the timing OR the dose OR both. For most adults, taking it earlier in the evening, and taking a normal physiological dose works better than large doses at bedtime.
And melatonin works best when it’s paired with the other half of the circadian equation: Bright morning light. You can get sunlight for free if you can get up and get out fast enough. Or you can buy something to force the ‘sunlight’ What I mean is a 10,000-lux light, such as a Verilux® light box (find it on Amazon) used for 20–30 minutes shortly after waking helps shut off melatonin in the morning and strengthens its natural rise at night.
Strong mornings create better nights. Bright mornings create better sleep.
Sometimes better sleep isn’t about adding more of this, or that — on occasion, it’s about using the right signals, at the right time.

Suzy Cohen, has been a licensed pharmacist for over 30 years and believes the best approach to chronic illness is a combination of natural medicine and conventional. She founded her own dietary supplement company specializing in custom-formulas, some of which have patents. With a special focus on functional medicine, thyroid health and drug nutrient depletion, Suzy is the author of several related books including Thyroid Healthy, Drug Muggers, Diabetes Without Drugs, and a nationally syndicated column.