What's On This Page?
ToggleHello beautiful souls! This article on the parathyroid glands is very personal to me because I used to have hyperparathyroidism. I had a quick 20-minute surgical procedure to help myself, completed in late 2022.
I am now cured. This blog contains information for people who are not sure what’s wrong yet, but they know something is wrong! As you can see from my image here, taken just hours after surgery, the cut is made at the base of the neck.
My story is woven throughout this blog too. Let’s start with the basics of parathyroid glands.
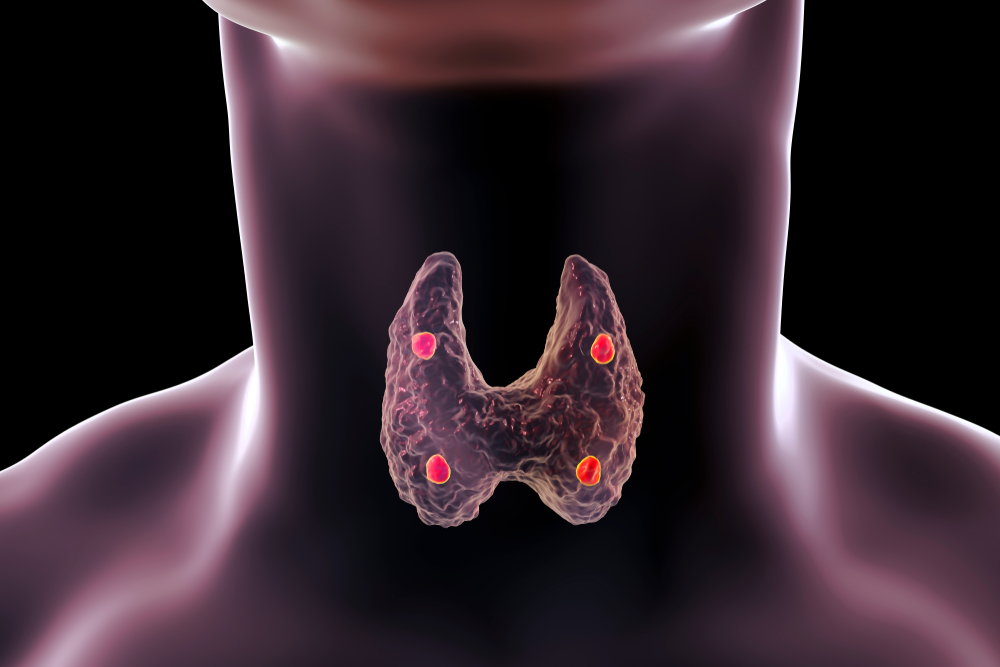
Parathyroid glands are part of the endocrine system that regulate the body’s calcium levels. Located in the neck, behind the thyroid, these four small glands produce Parathyroid Hormone which controls calcium levels in the blood, bones, and throughout the body.
I found out I had the disorder of hyperparathyroidism when a routine blood test found elevated levels of parathyroid hormone (PTH).
Parathyroid glands have NOTHING to do with your thyroid gland. It’s just a name.
The parathyroid glands are named for their location relative to the thyroid gland, rather than their function. The prefix “para-” in Greek means “alongside” or “near”, and these glands are called “parathyroid” because they are located near the thyroid gland in your neck.
The thyroid gland primarily regulates THYROID hormones.
The parathyroid glands regulate CALCIUM and PHOSPHOROUS in your body.
The parathyroid glands secrete a hormone called Parathyroid Hormone which I will now call PTH for short. This hormone controls calcium and phosphorous which is essential for our nervous and muscular systems to function properly. These two minerals provide the ‘electrical’ spark to make your muscles move, plus they’re needed to keep your bones strong.
Parathyroid disease
Elevated levels of PTH always mean there is parathyroid disease. It’s also known as hyperparathyroidism, and a tumor always causes it in one or more of your parathyroid glands. This results in excessive production of PTH which is measurable in the blood.
Here’s the thing though, there are some rare instances where you could have hyperparathyroidism, but your PTH may not be elevated! Weird, and luckily unusual. Most of the time it’s straightforward, and if you do have hyperparathyroidism you also have elevated PTH.
When PTH goes up in the bloodstream, this can lead to high calcium levels in the blood, affecting various body systems, notably the nervous system and it can cause weakness and cardiac problems. The term for high calcium is hypercalcemia. I wrote a blog about this which you should read soon. It’s called, Calcium and Hypercalcemia Treatment Options.
Calcium imbalance (particularly hypercalcemia) can also weaken bones and result in kidney stones. This confuses people because they think that the more calcium the stronger the bones.
Shouldn’t hypercalcemia give you super-strong bones? No.
So to clarify, hypercalcemia is elevated calcium in the blood, NOT the bones. In fact, with hyperparathyroidism, the bones dump calcium into the bloodstream, so they weaken! It is treated through surgery to remove the problematic gland which usually has an adenoma attached to it.
Few Key Differences Between Thyroid vs. Parathyroid Disease
Thyroid hormone is a totally different hormone versus parathyroid hormone (PTH). Totally and completely different.
Parathyroid disease impacts calcium levels, thyroid disease does not.
Thyroid hormone requires IODINE, selenium and other COFACTORS and HERBS.
Parathyroid hormone (PTH) requires none of the above – it does require 4 healthy functional glands.
Having thyroid disease does not automatically mean you will develop parathyroid disease, or vice versa. Neither has anything to do with the other.
The proximity in the body of the glands is the same, both the thyroid gland (you have one) and the parathyroid glands (you have four) are in the base of the neck below your Adam’s Apple.
As long as I am making clarifications, I want to give honorable mention to hypoparathyroidism (as in too little PTH). I want to tell you that hypERparathyroidism is FAR more common than hypoparathyroidism which is the medical term given to a person with decreased activity of parathyroid hormone. It rarely occurs, but you should at least know it exists.
About the Adenoma
It is a benign tumor that’s about the size of an olive that causes trouble and leads to elevated PTH and hypercalcemia. Removing this little troublemaker surgically always helps and brings the PTH down to the normal range.
But, guess what? In about 30% of cases, there’s more than one adenoma, so ensure your surgeon is thorough while he’s in there, and checks all your glands! For me, I had to have 3 of my 4 glands removed!
Despite the scary tumor talk, hyperparathyroidism isn’t cancer. It’s a hormone problem, though it can increase the risk of other cancers.
You may be wondering what makes a parathyroid cell go rogue and form a tumor? That’s still a bit of a mystery. But many times, it is genetic and this was the case for me with two close family members having had hyperparathyroidism, although I didn’t know this until after I had my own surgery. I found out after the fact.
When the adenoma grows, and the cells multiply like crazy, it causes the production of PTH which disrupts the balance of calcium in your body. READ THIS BLOG NEXT.
How Common Is It?
The incidence of hyperparathyroidism is 1 in 80 people in their lifetime (more than 1% of people). It’s higher in women above the age of 50 where the rate is more like 1 in 50.
It is only caught if you take a blood test and find out that your PTH is elevated, or your calcium is elevated. It’s a safe bet that most physicians are not testing the PTH too often, it’s just not part of a typical lab workup. But calcium is tested more frequently, so you might find out when they test that level. If it’s high, it’s quite possible if not likely that you have hyperparathyroidism, and you should go back and test your PTH levels along with the calcium.
Unfortunately, about 70% of patients with this condition do not know they have it!
They get a lab showing hypercalcemia (high calcium levels_ but their doctors don’t know what this means and so it gets ignored. Often, when something bad happens (kidney stones, bad osteoporosis, severe depression, intractable fatigue), and then maybe the doctor puts attention to the high calcium.
Hyperparathyroidism is pretty much a woman’s disease occurring in women 75% of the time, and only in men 25% of the time. Now let’s unpack the signs and symptoms which can sometimes be a bit of a whisper! The symptoms vary and differ each day.
They are different for each person. The symptoms are mostly tied to hypercalcemia. Most people with hyperparathyroidism don’t experience all of the symptoms below. And you don’t have to have super high calcium to have superbad symptoms!

It’s more about the duration of hypercalcemia versus the number itself. For me, mine was about 10.0 or 10.1, sometimes it dipped to 9.8 but the issue was that I had hypercalcemia for probably 10 solid years without realizing it! Contrast that with a woman my age who has a calcium level of 12.5 for example. My symptoms might be worse because I have had hypercalcemia for years, whereas the person with 12.5 levels might only have that for a month or two.
What I’m trying to say is that how high above normal the calcium has less to do with symptoms than the length of time it’s been elevated.
I can tell you firsthand you get used to some of these symptoms, it becomes your new baseline in life. You just adjust your entire life to the energy levels you have, you plan around the level of brain function you have, and the amount of sleep you get.
Only AFTER you have the surgery to remove the adenomas, and PTH goes to normal do you realize how significantly this disease has affected your life.
Symptoms of Hyperparathyroidism
Fatigue
Shortness of breath
Apathy
Forgetfulness
Weight gain
Feeling unwell
Insomnia
Irritability
Feeling foggy
Kidney stones
Heart flutters
Irregular liver tests
Headaches (READ THIS NEXT)
Bone pain
Reduced libido
Gastric reflux
Swallowing pain
Delving Deeper into Symptoms
Do you feel like you’re carrying weight, or easily exhausted? That’s the main symptom, alongside a vague feeling of “unwellness” that’s hard to pinpoint. It’s like a fog settling over your daily life, pulling your interest away from things you used to love, scattering your focus, and possibly stirring up the blues or unease. I’d say this was the main thing for me.
Fatigue is the leading symptom, affecting over 82% of patients. Most describe a shift in their energy levels that they can’t explain, often dismissed by doctors until hyperparathyroidism is diagnosed.
Bone pain is another major complaint due to the disease-causing calcium to be drawn from the bones, resulting in osteoporosis or osteopenia, and even small internal bone hemorrhages. A DEXA bone density scan helps determine the extent of calcium loss, and surgery becomes a necessary treatment, especially when bone density decreases significantly.
Your bones may speak up too, with discomfort, especially in your hands, feet, arms, and legs. Trouble catching those Z’s at night and needing daytime naps might creep in. Even your mood may shift, with irritability and memory lapses making you feel a bit off-kilter.
Physical signs may also include gastric reflux, a dip in libido, and even thinning hair, often noticed by middle-aged ladies. And let’s not forget the more serious issues like kidney stones, kidney disease, high or fluctuating blood pressure, headaches, heart flutters, and irregular liver tests.
Depression is also prevalent among hyperparathyroidism patients, with almost 48% reporting symptoms or being on antidepressants. After the surgical treatment of the condition, many patients can be weaned off these medications, often leading to a significant improvement in their mood.
Hyperparathyroidism can cause acid reflux (GERD) as well, due to the elevated calcium levels triggering increased acid production. This issue typically resolves after surgery
Constant exposure to high calcium levels due to overactive parathyroid glands may cause kidney stones. In severe cases, extensive calcium deposition can cause kidney failure. Around 24% of patients with hyperparathyroidism develop kidney stones.
Hyperparathyroidism can cause heart problems, including high blood pressure, arrhythmias (racing heart), and atrial fibrillation (racing heartbeat). About 6% of patients discover their parathyroid issue after experiencing cardiac symptoms. Removing the growing (benign) tumors can often resolve these heart-related issues, or stop it in its tracks. Left ventricular hypertrophy or LVH is really the specific problem for most people.
Patients with primary hyperparathyroidism may show a high incidence of left ventricular hypertrophy, cardiac calcification, and/or aortic and mitral valve calcification. Post-surgery, with normalized calcium and PTH levels, the progression of heart disease is halted, reducing the risk of severe valve stenosis.
Recurrent headaches may occur, especially among young people. This is often attributed to high calcium levels in the blood. Removal of the faulty gland(s) usually resolves these headaches. I didn’t have them personally, but they can be common in terms of symptomatology. You might be interested in my article about HEADACHES.
Patients often experience recurrent headaches, primarily due to elevated calcium levels. Hyperparathyroidism has a notable impact on life expectancy, with studies suggesting that those living with the disease for over 15 years have a life expectancy of about 5 years less than their peers.
Removal of the parathyroid tumor often resolves these complications, making it a key treatment strategy. Despite being a non-cancerous condition, its overall impact on the body is substantial, warranting prompt medical attention.
Resolution of hyperparathyroidism requires surgery and removal of the adenoma, it does not require removal of the thyroid gland which is not related at all. If you’d like to watch my journey, I started recording a VLOG right after I had the surgery (in 2022). I’ve finally uploaded it and you can WATCH IT HERE.
For the best information on the Internet, I recommend you visit PARATHYROID.COM
Stay strong and seek treatment if you need it. Once you are treated, you will wish you did it years ago. I believe in you. You’ve got this!

Suzy Cohen, has been a licensed pharmacist for over 30 years and believes the best approach to chronic illness is a combination of natural medicine and conventional. She founded her own dietary supplement company specializing in custom-formulas, some of which have patents. With a special focus on functional medicine, thyroid health and drug nutrient depletion, Suzy is the author of several related books including Thyroid Healthy, Drug Muggers, Diabetes Without Drugs, and a nationally syndicated column.

