What's On This Page?
ToggleThe focus of this article is about taking a ratio of two numbers from your CBC blood test to determine your PLR. So pull up a copy of your latest CBC (Complete Blood Count) blood test and let’s get started. We’ll use it for Hashimoto’s detection. First, let me remind you what this condition is like.
Imagine your body as a bustling city, where every cell and organ plays a critical role in keeping the metropolis alive and thriving. At the heart of this city lies a small but mighty gland, the thyroid, diligently working to regulate the pace of life.
Now, picture Hashimoto’s thyroiditis as a silent but persistent intruder, slowly infiltrating the thyroid, causing chaos and disrupting the harmony of the city. This analogy brings us closer to understanding Hashimoto’s thyroiditis, a condition first described by Dr. Hakaru Hashimoto in 1912.
It’s a story of the immune system mistakenly turning against the body’s own tissues, leading to chronic inflammation of the thyroid gland. Commonly presenting as hypothyroidism (and sometimes with a swelling in the neck called a goiter), this autoimmune disorder has been increasingly diagnosed over the past 10 years.
Yet, the journey from recognizing the symptoms which often go under the radar until a goiter on your neck appears, to managing the condition is fraught with challenges and treatment considerations. Sometimes with Hashimoto’s, the thyroid levels swing very high, causing one to become diagnosed with Graves’ disease which is a condition of hyperthyroidism.
Understanding Hashimoto’s Thyroiditis
Hashimoto’s thyroiditis (what I abbreviate as “Hashi”) is the silent disruptor of the thyroid, the master gland of metabolism. Your thyroid gland is the thermostat of your body, regulating temperature, energy, and overall vitality.
In Hashi, your immune system, usually the bodyguard against invaders, mistakenly perceives your own thyroid cells as the foreign threat! And it is just doing its job to get rid of that threat! Unfortunately, this autoimmune response leads to the gradual destruction of the thyroid, akin to a slow-burning flame that eventually dims the light entirely! Detecting Hashi’s as soon as possible is important so recognizing symptoms is critical.
Hallmark of Hashimoto’s Thyroiditis
The hallmark of Hashi is the presence of anti-thyroid antibodies, which is found via a simple blood test. Your doctor is specifically looking for anti-thyroid peroxidase (Anti-TPO) and anti-thyroglobulin (Anti-TG), turning the body’s protective mechanisms into agents of destruction.
The result is a spectrum of thyroid malfunctions, from the initial thyrotoxicosis, where the gland releases too many hormones, to eventual hypothyroidism, where it can scarcely muster any at all.
But there’s one more ratio you can take, if you have a CBC blood test.
The Platelet/Lymphocyte Ratio (PLR) Connection
Scientists have revealed a novel marker recently, it’s the Platelet/Lymphocyte Ratio (PLR). This information was published in March 2023, in a paper entitled, A Novel Inflammatory Marker for the Diagnosis of Hashimoto’s Thyroiditis: Platelet-Count-to-Lymphocyte-Count Ratio.
This easily obtainable measure from a complete blood count offers a window into the systemic inflammation characteristic of Hashi’s. A high PLR is like a distress signal, indicating your body’s heightened state of alert and inflammation! It’s a red flag saying to start making some changes. I’ve listed a simple 5-step strategy plan below for you to consider.
The Study at Hand
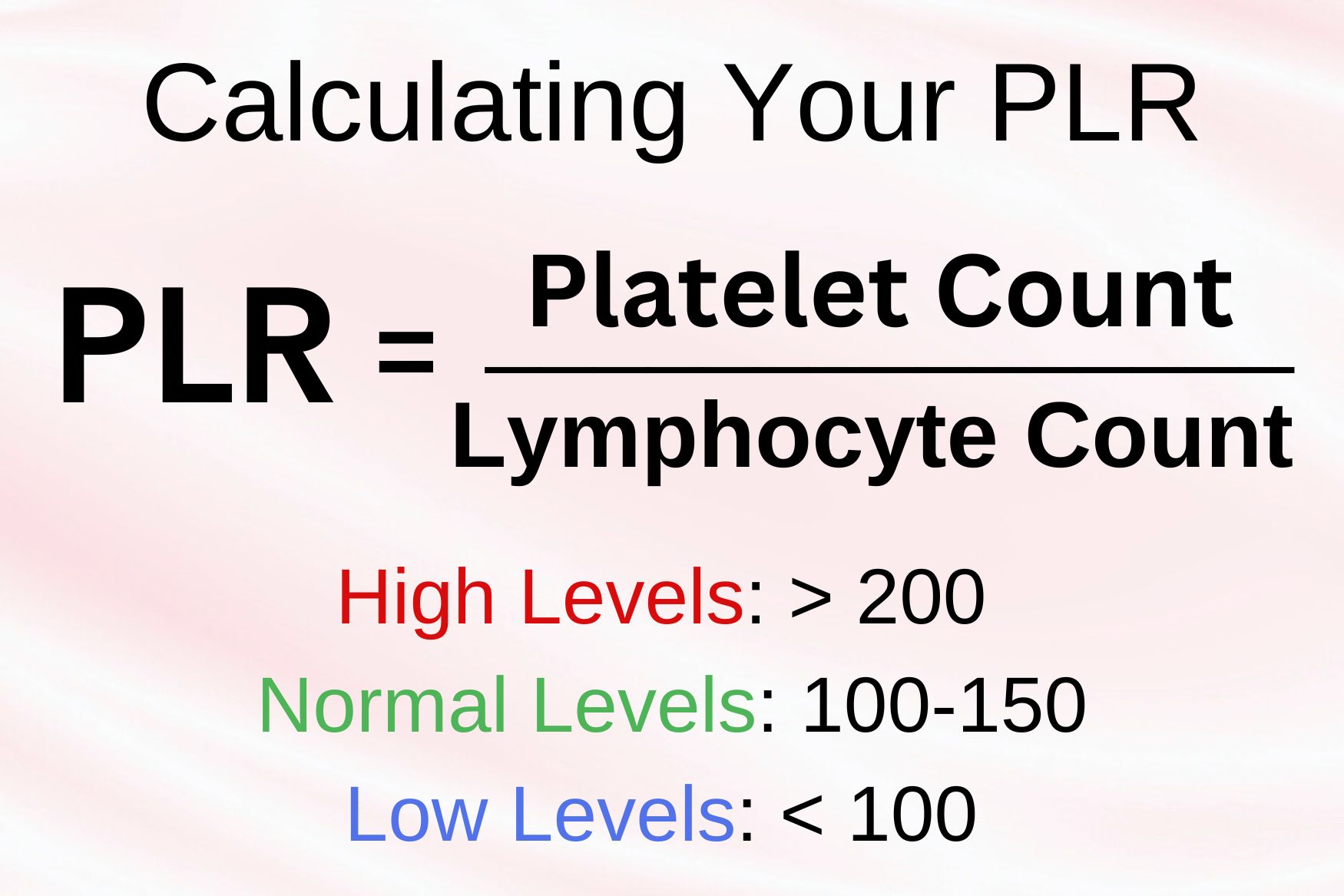
A recent study embarked on a mission to explore the PLR in patients with Hashi, seeking to illuminate the relationship between this inflammatory marker and the thyroid’s autoimmune assault. The study grouped subjects into euthyroid, hypothyroid-thyrotoxic, and control groups, diving deep into the comparison of their PLR values. The “P” means platelets and the “L” means lymphocytes, and the “R” means ratio.
The findings could pave the way for novel diagnostic and therapeutic approaches, offering hope to those navigating the turbulent waters of Hashimoto’s thyroiditis. You probably know that the word lymphocyte refers simply to white blood cells in our body. Those are important immune system cells that fight for you. And there are B lymphocytes and T lymphocytes. But the PLR is easy, you do NOT have to know that, you just use the number shown on your blood test which is a total.
How to Calculate Your PLR
For those wondering if there is a silent battle brewing within your thyroid, and symptoms related to this, get the two very specific thyroid antibody tests (Anti-TPO and Anti-TG), to offer clarity. But also get a CBC so you can calculate your PLR and see where it is. It’s easy to do. And it is important to calculate it. You can do it right now yourself.
The biomarkers are not special, they are measured in every single CBC blood test you’ve ever taken, but what’s groundbreaking is that we now know the ratio of platelets to lymphocytes is revealing. A CBC is quick, sometimes with same-day results, and it’s very affordable to pay for. You can even order this blood test yourself, HERE’s HOW.
Let’s walk through a hypothetical scenario of calculating the PLR with pretend lab results.
Hypothetical Lab Test Results
- Platelet count: 250,000 per microliter (μL)
- Lymphocyte count: 2,000 per microliter (μL)
Calculating PLR:
The PLR is calculated by dividing the platelet count by the lymphocyte count. Using the above figures, it would be 250,000 divided by 2,000 which equals 125. Remember this number.
Interpreting PLR Values
- Normal PLR: There isn’t a universally agreed-upon “normal” range for PLR as it can vary based on the lab and the population. However, for the context of this explanation, let’s consider a PLR in the range of 100-150 as within normal limits.
- High PLR: A high PLR might indicate a higher level of systemic inflammation. In the context of Hashimoto’s or other inflammatory conditions, a PLR significantly above 150 could suggest an elevated inflammatory state. For example, a PLR of 200 and above might be considered high.
- Low PLR: A lower PLR, let’s say, below 100, could indicate a relatively lower level of systemic inflammation. However, it’s essential to note that a low PLR is not specifically diagnostic and should be interpreted in the context of other clinical findings and tests.
Application in Hashimoto’s Thyroiditis
In people with Hashimoto’s Thyroiditis, monitoring PLR could provide insights into the inflammatory status and potentially the progression or management of the condition. A higher PLR might prompt further investigation or more aggressive management strategies, or dietary changes to address the underlying inflammation before it progresses into a full-blown condition.
Important Considerations
- The values and ranges provided here are hypothetical and used for illustrative purposes. Actual normal, high, and low ranges can vary based on the testing laboratory and the specific population.
- The interpretation of your PLR should not be done in isolation but along with a more comprehensive clinical evaluation, medical history, symptoms, other lab tests, and genetics.
How to Keep Your Platelets and Lymphocytes Healthy
You may be wondering what I was wondering which is if your platelets and lymphocytes are part of the clue to wellness, how do you keep those blood counts looking healthy?
And as you probably guessed, certain nutrients, herbs, and lifestyle factors can positively impact these blood components, while others might have a detrimental effect. Here’s an overview of what can help or hurt your platelet and lymphocyte counts.
Supplements for Platelet and Lymphocyte Health
Vitamins and Minerals
Vitamin C: An essential nutrient that can help with platelet production and function. It also supports the immune system, potentially aiding in healthy lymphocyte levels. I have a wonderful 100% natural Vitamin C product AVAILABLE HERE.
Vitamin K: Important for blood clotting and platelet formation. Leafy greens are a great source of Vitamin K.
Iron: Essential for the production of hemoglobin, which is crucial for platelet production. Iron deficiency can lead to thrombocytopenia (low platelet count).
Folate (Vitamin B9) and Vitamin B12: Both are crucial for DNA synthesis and the production of red blood cells, which can influence platelet production. A deficiency in either can affect platelet count.
Zinc: Plays a role in maintaining the health of the immune system, potentially influencing lymphocyte function and levels. Interested in a high-quality gentle CHELATED ZINC to help optimize your levels?
Herbs
Papaya Leaf Extract: Some studies suggest that papaya leaf extract can help increase platelet count, particularly beneficial in conditions like dengue fever where platelet count drops significantly.
Echinacea: Known to potentially boost white blood cell (lymphocyte) count and improve immune response.
Astragalus: May help improve immune function and has been traditionally used to boost the body’s defense mechanism, potentially affecting lymphocytes positively.
Problematic Things for Your Platelet and Lymphocytes
Alcohol Consumption: Excessive alcohol intake can suppress bone marrow function, leading to decreased platelet production and potentially impacting lymphocyte levels.
Smoking: Smoking tobacco can negatively affect both platelet and lymphocyte counts, among its other detrimental health impacts.
High Unhealthy Fats: Diets high in unhealthy fats may lead to inflammation and could potentially affect the body’s ability to produce and maintain healthy platelet and lymphocyte counts.
Certain Medications and Conditions
Chemotherapy and Radiation Therapy: These treatments can significantly reduce platelet and lymphocyte counts as they target rapidly dividing cells, including those in the bone marrow.
Autoimmune Disorders: Conditions like lupus can lead to reduced platelet production due to the body’s immune response against its own cells.
Infections: Certain viral or bacterial infections can temporarily decrease lymphocyte count or affect platelet production.
5 Step Strategy List to Reduce Inflammation
- Engage in Regular Monitoring and Medical Consultations: Stay Proactive with Thyroid Function Tests
- Adopt a Thyroid-Friendly Diet
- Reduce Inflammatory Foods: Limit foods that can exacerbate inflammation, such as processed foods/sugar.
- Increase Anti-inflammatory Foods: Incorporate foods rich in omega-3 fatty acids, antioxidants, and selenium (found in Brazil nuts, fish, and fresh vegetables) to support thyroid health and reduce inflammation.
- Prioritize Stress Management and Mental Well-being through Exercise, Hobbies or Mindfulness
It’s not a strategy, because it’s really hard to just “do” but I recommend sleep! If you have the option to go to bed earlier, and improve your sleep hygeine to get more sleep, try your best. Aim for 7-9 hours of quality sleep per night to support overall health, including thyroid health. If you need help sleeping longer, or falling asleep faster, consider Sleep Script Tranquility Caps.
Summary
Hashimoto’s thyroiditis, affects millions of people every year, and each journey is unique. Through the lens of the Platelet/Lymphocyte Ratio or PLR, we glimpse into the body’s complex response to autoimmune thyroiditis, finding opportunities for early intervention.
As we continue to unravel the mysteries of HT, let’s remember the power of knowledge, vigilance, and hope in navigating the path to wellness. Armed with awareness and the right tools, the road to managing Hashimoto’s thyroiditis becomes a journey of empowerment and healing.

Suzy Cohen, has been a licensed pharmacist for over 30 years and believes the best approach to chronic illness is a combination of natural medicine and conventional. She founded her own dietary supplement company specializing in custom-formulas, some of which have patents. With a special focus on functional medicine, thyroid health and drug nutrient depletion, Suzy is the author of several related books including Thyroid Healthy, Drug Muggers, Diabetes Without Drugs, and a nationally syndicated column.