What's On This Page?
ToggleWith many adults encountering shortness of breat at some point in their lives, whether due to exercise, high altitudes, pregnancy, illness, asthma or temporary stress I think today’s article will lend insight and help you take care of yourself.
Navigating the maze of what might be causing your shortness of breath is like piecing together a puzzle but it’s critical to figure out the root cause in order to get the right treatment. Maybe you’re wondering what it is. Let’s start there.
Imagine you’re climbing a steep hill, and with every step, your chest tightens, demanding more air than you can gulp down. This feeling, even when you’re not hiking a mountain or biking, but perhaps just walking across the house or sitting still, is what many describe as shortness of breath, medically known as dyspnea.
There’s the situation of overbreathing too, have you heard of that word before? It can occur during times of anxiety, panic attacks, physical exertion and high altitude. The relationship between overbreathing (often referred to as hyperventilation) and shortness of breath can seem like a “chicken or the egg” scenario. In reality, it’s a bit of both, as the two can be both a cause and effect of each other, depending on the situation.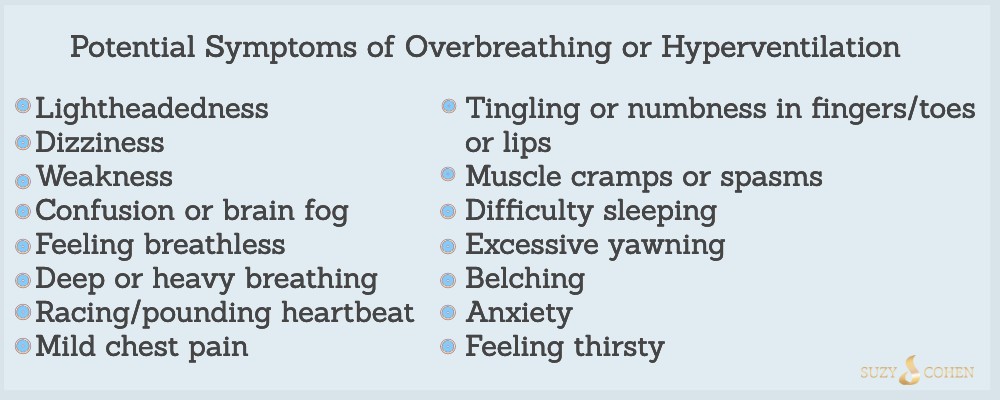
It’s a sensation of uncomfortable breathing, a feeling that you’re not getting enough air, or sometimes it feels like you’re suffocating, but it is different than air hunger.
It may be short-term if it’s associated with exercise, or with bronchitis, but for many of you it is persistent. It indicates that your body isn’t exchanging oxygen and carbon dioxide efficiently inside your lungs.
Introduction to Shortness of Breath
Shortness of breath is a common symptom that can range from mild and temporary to severe and long-lasting. It’s not a disease in and of itself, but rather a red flag from your body, signaling that something’s amiss in either your respiratory system or cardiovascular system. Some people have found that drinking grape juice helps! I don’t know if it would be useful or not, but certainly can’t hurt… and it’s delicious. I wrote about it in my article entitled, How Grape Juice Helps Shortness of Breath and Heart Disease.
How Often Does It Occur?
The occurrence of shortness of breath varies widely among people depending on the cause. It also depends on factors such as age, fitness level, underlying health conditions, past medical history and environmental exposures.
I’d say mild shortness of breath is a relatively common experience, I’ve had it myself when I was pregnant 30-something years ago and I didn’t know I was (iron) anemic, and I was running errands around Florida in 95-degree heat! It felt very uncomfortable, and it was scary.
Disorders and Conditions Associated with Shortness of Breath
1. Respiratory System Disorders: Conditions like asthma, chronic obstructive pulmonary disease (COPD), pneumonia, COVID-19, a lung abscess, pulmonary embolism, pleurisy, and lung cancer can directly impact your lungs’ ability to function, leading to gasping for air feeling.
In this category, I should include pertussis (whooping cough), and cystic fibrosis, a genetic disorder that turns mucus into a sticky trap, hindering breathing. Pulmonary edema can occur with viral lung infections as we saw with the pandemic. The lungs may start to fill with fluid and making breathing a struggle.
Speaking of the pandemic, I have a new ebook that I recently unveiled. It’s about Long COVID and you can get it emailed right now if you download it HERE.
The treatment for this is to clear the infection and consider asthma drugs such as inhalable steroids and bronchodialators. Watch my VIDEO on this top. Alternatively, you can take 5 to read my article asthma meds HERE.
2. Cardiovascular Issues: Heart failure, cardiomyopathy, or a heart attack can hinder your heart’s ability to pump blood efficiently, affecting your lungs’ oxygen supply and causing shortness of breath.
This is also a good time to mention deconditioning, as in skipping the gym! If you’re out of shape, your heart won’t be able to handle a lot at first, and it will make you pant with the slightest exertion.
The treatment for this is to address the heart problems and doctors do this using various medications including ACE inhibitors, nitroglycerin and other vasodilators. They also may employ natural CoQ10 (or Ubiquinol) as well as hawthorne. Read my article on 8 Natural ACE inhibitors. And, for those of you who want to watch an old video of me talking about taurine, magnesium and other heart healthy nutrients, CLICK HERE. Ok, so that video will satiate anyone’s morbid curiosity of how I looked 11 years ago when I did TV! Is it cringe-worthy, or did I read the prompter okay?? 😂
3. Anemia: A blood condition, marked by a lack of healthy red blood cells, can make you feel breathless since there’s not enough oxygen being transported throughout your body. You can easily find out if you’re anemic by taking a blood test. You’d order a CBC (complete blood count), hemoglobin and ferritin levels to get a pretty good screening. Did you know that: You Can Order Your Own Blood Tests.
The treatment for this is to address the abnormalities found in the blood test. For example, a 90 day course of iron supplementation or TMG acid supplements may be useful if it’s iron deficiency anemia, or maybe some B12 if it is pernicious anemia. You may be interested in reading my other article, Energy Hacks for Tired People.
4. Anxiety and Panic Disorders: Psychological factors can also manifest physically, with shortness of breath being a common symptom during panic attacks or periods of intense anxiety.
5. Obesity: Carrying significant excess weight can strain your heart and lungs, making even minimal exertion feel like a marathon.
6. Environment: Shortness of breath can also be influenced by environmental factors, such as exposure to allergens, pollutants (ie asbestos, benzene), and mold exposure.
Since I live in Colorado at high altitudes, I sometimes see people suffering after their plane lands, or when hiking. It’s because the air is thinner here and oxygen levels are lower. One last environmental toxic exposure that comes ot mind is radon. It’s a radioactive gas that can sneak into homes, potentially leading to lung problems over time. You can buy home test kits to check your house for radon.
7. Pets: Some individuals with pet allergies (particularly those with chronic asthma) may experience symptoms similar to those of hay fever, such as a runny or congested nose, sneezing, itching or watering of the eyes, and difficulty breathing.
8. Sleep apnea: It’s like your body forgets to breathe while you’re sleeping, leaving you gasping for air. This condition can lead to daytime fatigue and exhaustion. The treatment for this varies, and your doctor knows best. They use things like a CPAP machine, oral appliances, nerve stimulation, weight loss, and sometimes surgery.
9. Acid reflux: It’s not just about heartburn – it can also lead to breathing difficulties that feel like asthma. But here’s where the plot thickens because if you treat the acid reflux with a medication (versus a change in your diet), and you take an acid-blocking medications (prescription or OTC doesn’t matter)… then your acid levels go down.
There will be less chest pain and less risk for shortness of breath. Buuuut, for vitamin B12 to be absorbed, it must be released from food through the action of your stomach acid!
10. Autoimmune disorders: There are many autoimmune conditions that lead to interstitial lung involvement, making breathing a bit of a task. The lung involvement may not occur right at first, but over time it may manifest.
Among the most common autoimmune disorders that are associated with shortness of breath: Dermatomyositis, Polymyositis, Lupus, rheumatoid arthritis, sarcoidosis, Sjogren’s syndrome, scleroderma and mixed connective tissue disease. The treatment for autoimmune is complex and includes medication, lifestyle changes and diet.
11. Infections: Histoplasmosis is a fungal infection that’s got a thing for the lungs, causing SOB. Many people have Lyme disease from a tick bite. They may not even know they have Lyme but regardless of that, this infection and it’s other tick-borne co-infections are tricky because they involve the heart, often leading to shortness of breath, chronic fatigue and muscle weakness.
I wrote an article about this topic: Lyme Disease and Bartonella is More Common Than You Think.
Another infection called Legionnaires’ disease (caused by Legionella bacteria) also impacts the lungs.
I was just 11 years old and remember the television news for months going on about Legeionnaire’s disease. The outbreak happened in 1977 when people attended an American Legion convention in Philadelphia and the hotel’s air condition system spread the pathogen throughout the building! Over 180 people got sick, and 29 died from the condition which is caused by bacteria named Legionella pneumophila.
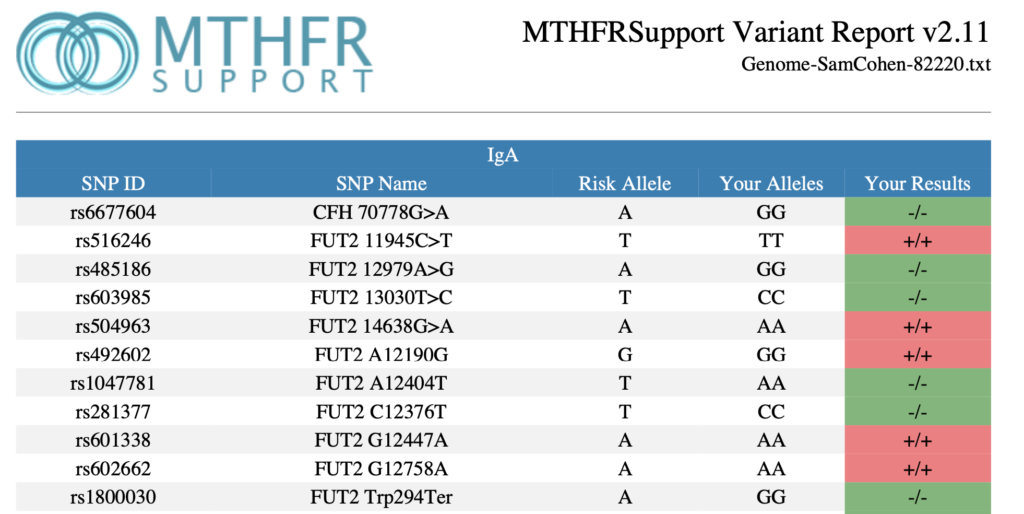
11. Vitamin B12 Deficiency: B12 is crucial for making red blood cells. Low levels? It’s like your body’s running low on its oxygen delivery fleet. For doctors and geneticists, there are various polymorphisms that you can look for in your patients that might point to trouble with B12 production and/or assimilation. I’d look for gene SNPS in the FUT2, TCN1 (transcobalamin 1), TCN2, CUBN, and MTHFR. You can read more about MTHFR here, Methylation Leads to 100s of Diseases.
12. Zinc Deficiency: Zinc plays a role in maintaining healthy immune function. Low levels might leave you more susceptible to respiratory infections. The treatment for zinc deficiency is zinc supplementation. You can find a high-quality brand of this HERE.
13. Magnesium Deficiency: Magnesium helps with muscle and nerve function; low levels can lead to respiratory muscle weakness. People with low RBC (red blood cell counts) which accompanies iron deficiency, also often have a magnesium deficiency. The treatment includes magnesium supplementation.
14. Carbon Monoxide Poisoning: It’s a silent but deadly gas that competes with oxygen, making you gasp for air. We had an idiot install our furnace downstairs and tiny amounts of CO gas were leaking from it for months, causing our smoke alarms (which are new and have a CO2 detector on them) to go off because the sensor was triggered.
15. Hypothyroidism: Last but not least, a deficiency of thyroid hormone (or inability to activate it) can cause chronic fatigue and shortness of breath with exercise. For that matter, you may have an inability or decreased ability to do any kind of exercise. This condition is sometimes associated with low Vitamin B12, iodine deficiency, and iron deficiency anemia. The treatment is medications that provide thyroid hormone, or supplements which can improve T3 conversion.
Mold Exposure and Shortness of Breath
Having lived in Florida and seen a lot of people with mold exposure, this issue can invade a home when you least expect it. I recall one apartment me and my family lived in for 6 months that had a guest room (which we used) where one wall was entirely black and this mold climbed 3 to 4 feet up the wall! The landlord wouldn’t fix it, and wouldn’t let us leave.
Nothing happened to us luckily, but it is disgusting to even think about. Many people are sensitive and can become diasbled from such an exposure. Mold spores float around and decide to land and multiply in damp areas, they can become more than just an unsightly nuisance, they can destroy your health!!!
For many, mold triggers allergic reactions, including sneezing, runny nose, coughing, red/watery eyes, and/or skin rash. And naturally, it can lead to respiratory issues like wheezing and shortness of breath, especially in those with asthma or allergies.
Identifying mold in your home is critical. You must play detective and eliminate it. and Eliminate: Play detective and look in the common spots like bathrooms, kitchens, basements, and around windows. Once you find it, use a special mold cleaner, or hire a professional. Of course, wear a mask, and be very careful.
Control humidity if it’s possible. If you live in the south, it’s not possible, but I still feel the need to tell you to keep your humidity levels in check (ideally between 30% and 50%). And finally, ventilate your home to keep moisture down. This means using exhaust fans, opening windows if weather permits and making sure your bathrooms and kitchen have proper venting. Hire a contractor to fix leaks and broken pipes in and around your roof.
Consult a professional for repairs of your home, and repairs of your body. Having mold illness is dangerous and should not be self-treated.
Gene SNPs and Vitamin B12 – Physicians Please Be Aware
When it comes to the genetic influences on vitamin B12, several SNPs can impact how this vital nutrient is absorbed, utilized, and metabolized in the body. If you are a doctor who specializes in interpreting 23andme reports, or other genetic reports, here are a few key polymorphisms you need to know:
FUT2 (Fucosyltransferase 2): The FUT2 gene influences the secretion of certain blood group antigens in bodily fluids and mucosa. Variants of this gene, particularly the rs601338 SNP, have been associated with altered B12 levels. People with certain FUT2 variants are “non-secretors” and may have a higher risk of vitamin B12 deficiency due to changes in the gut microbiome that affect B12 absorption.
Take a look at the screenshot here for my hubby who has multiple homozygous FUT2 gene SNPs. He sometimes gets a methyl B12 shot (not cyano) and also takes my Mito B Complex which contains both the methyl B12, and the mitochondrial “adeno” form of B12. Probiotics are part of his routine because those help you make your own B12.
MTHFR (Methylenetetrahydrofolate Reductase): While not directly related to B12 production, the MTHFR gene plays a crucial role in the metabolism of folate and homocysteine, substances closely linked with B12.
SNPs in MTHFR, such as C677T (rs1801133) and A1298C (rs1801131), can affect homocysteine levels and folate metabolism, indirectly influencing B12 utilization due to the interdependence of these nutrients in the methylation cycle.
TCN1 (Transcobalamin I): This gene encodes a protein that binds vitamin B12 in the blood and helps transport it to tissues. Variants in TCN1 could impact the efficiency of B12 transport and its availability to cells. If you have a patient who’s homocysteine is high, you might interested in my other article MTRR and Homocysteine which delves deeper into this connection regarding vitamin B12. It could shed light on the issue, and fix it once and for all.
TCN2 (Transcobalamin II): Similarly, TCN2 is responsible for producing transcobalamin II, another protein that binds and helps deliver B12 to cells. Variants in the TCN2 gene can affect the body’s ability to use vitamin B12 effectively.

CUBN (Cubilin): CUBN encodes a protein involved in the absorption of vitamin B12 in the intestine. Mutations in this gene can lead to impaired absorption and B12 deficiency.
Understanding the dance between nutrients like phosphatidylcholine and vitamin B12, and the genetic backdrop against which this occurs, highlights the beautifully complex interplay that sustains our health. If you’re navigating through issues related to vitamin B12, considering both nutritional intake and genetic predispositions can offer a more comprehensive approach to managing your well-being. Always consult with a healthcare provider or a genetic counselor to understand the implications of these interactions for your health.
Summary
Diving into this list might feel overwhelming, but it’s a reminder of how interconnected our health is with our environment, lifestyle, and nutrition. If shortness of breath is cramping your style, it might be worth considering these potential culprits.
And remember, while Dr. Google has its charms, nothing beats a real conversation with a healthcare practitioner, or maybe two, even three. I like opinions, I think you should get several opinions if you have unexplained shortness of breath. Doctors can help you navigate through this list and find out what’s really going on. Keep listening to your body—it’s the best health advisor you’ve got!
If you’re experiencing shortness of breath, especially if it’s new, worsening, or interfering with your daily activities, it’s essential to consult a healthcare professional. They can help unravel the mystery behind this symptom, whether it’s a sign of something minor or an indicator of a more serious health issue. Understanding shortness of breath is the first step towards breathing easier, both literally and figuratively. Remember, your health is a story where you’re the main character, and taking proactive steps to address symptoms like these ensures your story is a long and healthy one.
And remember, it’s always better to get checked out and breathe easy knowing you’re taking care of yourself. Stay healthy, stay curious, and let’s keep that breath flowing smoothly!

Suzy Cohen, has been a licensed pharmacist for over 30 years and believes the best approach to chronic illness is a combination of natural medicine and conventional. She founded her own dietary supplement company specializing in custom-formulas, some of which have patents. With a special focus on functional medicine, thyroid health and drug nutrient depletion, Suzy is the author of several related books including Thyroid Healthy, Drug Muggers, Diabetes Without Drugs, and a nationally syndicated column.