What's On This Page?
ToggleWhen someone you love abuses alcohol, cannabis, or other substances, it can feel like living inside a storm without shelter. You’re worried sick, sleep-deprived, and walking on eggshells. Your loved one might drive recklessly, mock your concern, or detach emotionally. Your instinct is to warn, nag, negotiate, or plead. But as many parents and spouses discover, that almost always backfires.
I once heard from a recovered ‘user’ that the only thing powerful enough to motivate change is fear – fear of what life will look like if the behavior continues. But worry alone is not a sustainable recovery plan. Compassion, connection, and practical strategies matter just as much. I don’t think my brother had that much fear (in order to change) because he passed away from cancer, never having fully recovered from his drug abuse and alcholism. If you want to read my tribute to him, and get help for yourself before it’s too late, that article is archived here, My Brother Was a Secret.
What a Recovered User Told Me
One of the most eye-opening conversations I’ve had was with someone in long-term recovery. He explained that not everyone can learn from someone else’s story — some have to walk through the fire themselves. In his words:
Some people are able to learn from other people’s experiences and what they share, while some of us have a lot of trouble doing that. We kind of do a cost–benefit analysis and decide that continuing to use has a net benefit — for all the reasons you mentioned, like hiding pain or numbing stress — so we keep going. The difficulty of quitting feels like an impossible barrier, so it adds to the ‘cost’ of stopping. Anything you can do to increase the benefits of not using, and lower the perceived costs of quitting, helps. But if someone can’t learn from others, they may need to go through it themselves.
That perspective hit me kinda hard. It reframes substance use as a personal math problem… one where the “benefits” of using (relief, escape, coping) seem to outweigh the steep “cost” of quitting. It also explains why lectures or warnings don’t usually work. What does help is tipping the balance and showing him/her that life without substances can carry more joy, safety, connection, and meaning than the exhausting and expensive cycle of use.
Two books that helped shape my thinking are:
- Beyond Addiction: How Science and Kindness Help People Change — a sensible, hopeful guide for families who want to influence change without confrontation.
- How to Help the One You Love by Brad Lamm — written by a person who went through serious substance use disorder and later became a Certified Interventionist, educator, and author. His message is that recovery and reconnection are possible, and families can play a loving, non-confrontational role.
Connection Before Correction
If you take one principle to heart, let it be this: Your connection always precedes correction.
When someone feels attacked (and almost anything you say can feel like an attack), they shut down. When they feel cared for, and not judged, they’re more likely to open up. This can feel impossible to do but you CAN, and you will learn how if you want to maintain a portal of communication.
Connection can be as simple as sending a short text or emoji that communicates love without judgment:
- “Thinking of you. Love you.”
- “Good morning, I hope you find one thing today that makes you smile.”
- “No pressure to respond, just wanted you to know how much you mean to me.”
It may feel awkward at first, but these small gestures say, “I’m safe. I’m not here to judge you.” And that can be the first crack in the wall.
Curiosity, Not Confrontation
Instead of grilling your loved one about quitting, try curiosity (don’t expect an answer):
- “What do you like most about smoking?”
- “When you drink, does it help with stress from your clients?”
These aren’t trick questions. They give your loved one a chance to share their reality without shame. Over time, gentle conversations like this help them reflect on whether the substance is truly helping or just masking pain.
Why People with Addiction Feel the Need to Self-Medicate
Substance abuse isn’t about weakness or being “bad.” It’s often about self-medication. Many people are unknowingly trying to treat ADHD, anxiety, depression or some kind of childhood trauma (sometimes called complex PTSD or CPTSD). Read more at the website for The National Child Traumatic Stress Network.
The book I read called Re-Regulated explains how unresolved trauma rewires the brain into survival mode causing a person to have hypervigilance, emotional numbing, difficulty regulating stress. They become dysregulated when they’re triggered years later. Drugs and alcohol become shortcuts to relief, even though they create larger problems over time.
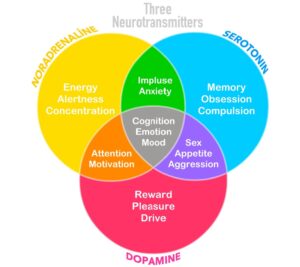
A Pharmacist’s Take: Dopamine and the Cycle of Relapse
From my pharmacist’s perspective, here’s what’s happening physiologically:
Drugs and alcohol hijack the dopamine system. Each use of the substance floods the brain with dopamine. The brain adapts by downregulating receptors as in ‘shrinking’ its natural ability to feel joy. This happens because the brain reduces its sensitivity to dopamine. So your brain doesn’t respond as strongly as it normally would to everyday rewards. Like, normal things that used to spark joy (like food, hobbies, or relationships) feel less satisfying. Unless there’s a new ‘hit’ of alcohol or drug, the brain is a bit numb.
That’s why quitting cold turkey can feel unbearable. Life suddenly seems flat and empty.
This isn’t a failure of willpower. It’s neurochemistry. And it’s why relapse is so common. The brain desperately seeks that dopamine hit from a drug, or adrenaline-producing activity.
The antidote? Healthy dopamine replacements. It will take time though. The brain doesn’t repair in a day or two unfortunately. But weeks or months, it will.
Beyond Addiction encourages families to guide loved ones toward new sources of pleasure: exercise, music, art, nature, laughter, friendships, or meaningful goals. These aren’t fluffy extras. They’re brain medicine.
Treatment Options and Natural Support for Substance Abuse
While there’s no magic pill, some medical and holistic options can help:
- Antabuse (disulfiram): This causes an unpleasant reaction with alcohol, though adherence is often a challenge because of that. No cheats can happen without a highly unpleasant reaction so lots of times people don’t stay compliant.
- Naltrexone: Reduces cravings for alcohol and opioids by blocking reward pathways. Low-dose naltrexone (LDN) also shows promise.
- Acamprosate: Helps rebalance brain chemistry in alcohol dependence.
- Herbal supports: Milk thistle (for liver health) or kudzu (studied for reducing alcohol cravings). These aren’t cures, but they may support recovery.
Underlying ADHD or mood disorders need support too:
- MAGNESIUM: Sometimes nicknamed the body’s “chill pill.” Chelated forms or magnesium L-threonate are better absorbed into the brain than the cheaper drugstore versions. I have MagFocus® a patented, high-quality (easy-on-the-tummy) form of mag threonate at my SHOP.
- Omega-3 fatty acids (DHA/EPA): Shown to help with attention and mood regulation.
- ZINC: Supports healthy neurotransmitters. Read this article too: The 6 Reasons Caffeine Helps ADHD
- B vitamins (especially B6 and B12): Critical for neurotransmitter balance. Here’s a mitochondrial-loving form that works: Mito B Complex
- Sleep and exercise: Simple, often overlooked tools for calming the nervous system. As for exercise, it can be either relaxing (like yoga or tai chi, or more active like jiu jitsu, cycling or weight lifting for example)
- Glycine: You can buy supplements of this online or at health food stores. A fascinating animal STUDY looked at how the amino acid glycine interacts with the brain’s reward system. Alcohol stimulates dopamine release in the nucleus accumbens — the brain’s pleasure hub — partly through glycine receptors. When researchers gave rats glycine, it raised glycine levels in the brain, and in a subgroup of “dopamine responders,” dopamine shifted too. The most encouraging finding? The rats drank less alcohol and showed less preference for it after glycine treatment. This suggests that raising glycine levels (whether through direct supplementation or medications that affect glycine transport) might one day become a new way to help people with alcohol use disorder.
Therapy can be healing, but sometimes reliving trauma out loud retraumatizes instead of helping. Thankfully, many therapists now use gentler methods that regulate the nervous system without forcing patients to rehash painful memories.
Boundaries Without Ultimatums
Loving connection doesn’t mean ignoring danger. Boundaries protect you, too. For example, it’s totally in bounds to say, “I won’t get in the car with you if you’ve been drinking.” or “I love you, but I can’t let the baby ride with you if you’ve been smoking.” Clear, calm boundaries aren’t ultimatums. They’re safety nets. They prevent potentially catastrophic injuries too.
Encouragement for Families
If you’re the parent or spouse of someone struggling with addiction, you probably feel powerless. But you’re not. Every time you set a boundary, send a gentle text, or choose compassion instead of criticism, you’re doing something.
It may not look like progress, but connection is never wasted. You’re keeping the bridge intact, so your loved one knows where to turn when they’re ready. And you’re protecting your own health along the way.
You can’t force someone to change, but you can make it more possible for them to want to.

Resources to Explore
- Beyond Addiction — Foote, Wilkens, Kosanke
- How to Help the One You Love — Brad Lamm
- Re-Regulated — on childhood/complex PTSD
- Radical Acceptance — Tara Brach
- The Anxious Generation — Jonathan Haidt
- Don’t Let Your Kids Kill You — Charles Rubin
- SMART Recovery Family & Friends
- Al-Anon and Nar-Anon support groups
Final Thought
If you’ve lived this storm, you’re not alone. Thousands of parents and spouses wake up every day with the same fear — and keep showing up anyway. That persistence, that love, is more powerful than you realize.
If you or someone you know is struggling with substance abuse or a health disorder, call the SAMHSA National Helpline: 1-800-662-HELP (4357) or visit: https://www.ssamhsa.gov for free, confidential treatment referral and information, 24/7.
And if you’ve found strategies or resources that helped you, I’d love to hear them. Feel free to email scriptessentials@gmail.com I may share a few responses in future blog posts to give other families hope. If you’d prefer not to use your real first name, feel free to sign with an alias.
Shared Wisdom from Our Readers
Regarding a resource:
Thank you, Suzy! I have a daughter who struggles with alcohol abuse. She’s in her mid-30’s. Neither of us could connect with the Alcoholics Anonymous programs. In searching for help we both needed, we found SMART for Friends and Family. Game changer!!! Not only do we benefit from in-person meetings, but we can go on-line to find national meetings for support. Thank you for using your platform to promote options for care. I never knew how important self-care was until this. From Deb
I had a thyroid doctor (alternative of course) that told me he had never treated an alcoholic who didn’t have a thyroid problem. He was also a sports medicine doctor and found that treating the thyroid removed the pain. I also wonder what the connection is between the MTHFr defect and addictions (would taking methyl-folate and B12 help?) I have several in my extended family who have depression (and we do have the MTHFR defect in our genes). From Lynn

Suzy Cohen, has been a licensed pharmacist for over 30 years and believes the best approach to chronic illness is a combination of natural medicine and conventional. She founded her own dietary supplement company specializing in custom-formulas, some of which have patents. With a special focus on functional medicine, thyroid health and drug nutrient depletion, Suzy is the author of several related books including Thyroid Healthy, Drug Muggers, Diabetes Without Drugs, and a nationally syndicated column.