What's On This Page?
Toggle Are you taking EPA meaning fish oils? It’s a wonderful adjunctive remedy that even the American Heart Association lists on their website. And the focus of today’s article is how taking EPA can help your statin work even better! It’s not a substitute, it’s something to be used along with.
Are you taking EPA meaning fish oils? It’s a wonderful adjunctive remedy that even the American Heart Association lists on their website. And the focus of today’s article is how taking EPA can help your statin work even better! It’s not a substitute, it’s something to be used along with.
We know statins deplete CoQ10, it’s well-documented as happening since it’s part of the mechanism of action whereby cholesterol production is hindered in a metabolic pathway. Does your brain pay any price for less CoQ10? Of course, it’s a fatty organ that relies on CoQ10.
Your brain ‘on statins’ is bound to suffer due to the well-documented depletion of Coenzyme Q10, and so the search for natural ways to reduce cholesterol (or maybe just leave it alone!) continues.
It was on September 1, 1987, that lovastatin (Mevacor) became the first statin to gain FDA approval. Since then, hundreds of clinical trials have been conducted on statins, as well as other agents that augment the statin’s cholesterol-lowering effect.
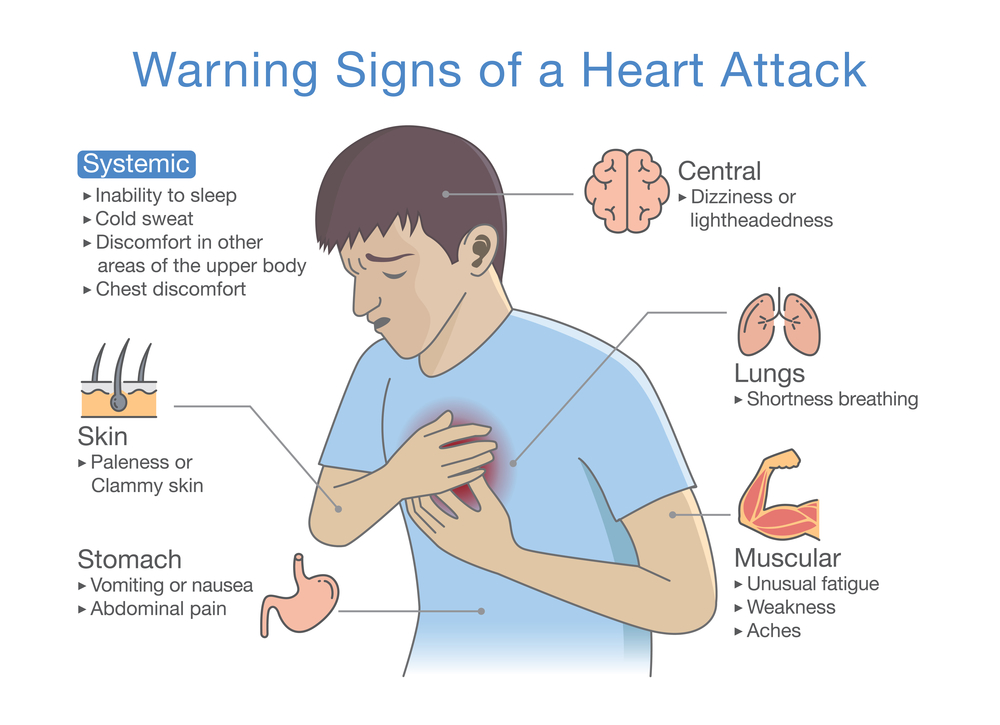
⚠️ Over 15.5 million Americans have CAD, Coronary Artery Disease. Every 42 seconds a person has a heart attack (termed myocardial infarction or MI). A full 1/3 of these people die. These are numbers we need to take seriously.
We all want to find answers to these problems. There’s even an old folk remedy that some people swear by that has to do with taking a drink of water that includes a little cayenne pepper! I know, I know that sounds crazy doesn’t it. You can look it up yourself. I read that on “Dr Google” while I was researching its health benefits which might help you too. Try CLICKING HERE to read my article, Cayenne Pepper Stopped My Bleeding in 30 Seconds Flat!
So the important questions for a savvy person like you are these:
- Do statins reduce your risk for a heart attack?
- Do they prevent death?
- Do their side effects make drug therapy worthwhile?
- Is it indeed cholesterol that causes arterial plaque accumulation, eventually halting blood flow to the heart?
These are 4 important questions that you can pose to 50 different doctors, and you’ll get 50 different answers. The conventional method of treatment for high cholesterol is of course… none other than a statin!
Statins are widely advertised by their manufacturers, who harvest $25 billion in revenue annually. Their use in everyone, especially kids, is very controversial, and for good reason. Statins have the ability to cause serious nutrient depletions, what I call ‘drug mugging.’ The stolen nutrients are the following: CoQ10, selenium, zinc, vitamin D, E and copper.
For more on drug nutrient depletion, refer to my book, Drug Muggers, Which Medications are Robbing Your Body of Essential Nutrients and Natural Ways to Restore Them
It’s the loss of important nutrients in your body that contributes to dozens of symptoms and new diseases. Maybe you didn’t realize that… Yes, your body is running thousands of chemical reactions per second, and the only thing that binds to the cell’s receptor (naturally) is a vitamin, enzyme or mineral – not a drug. Drugs are made to temporarily fit a receptor and mimic the actions of natural nutrients you are born with.
So for sure, restoration of missing nutrients (due to poor diet) could help out, and could minimize the number of new diseases you get diagnosed with, as well as the risk for heart attack. You can read THIS ARTICLE I wrote about some of the most common drug muggers you should keep an eye out for.
Can Statins Contribute to Other Disorders?
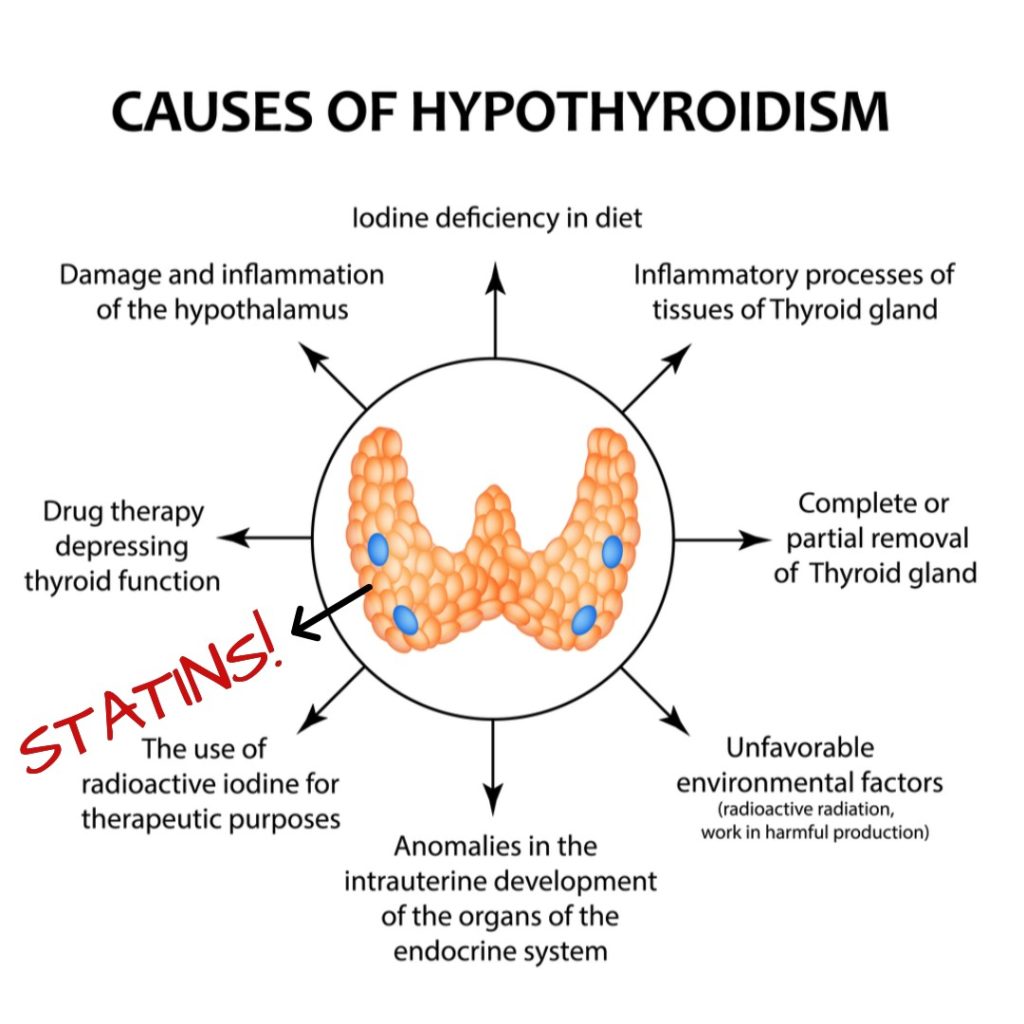
After about a year or two of taking a statin, many people realize they have a few more diagnoses for diseases, most common among them: Hypothyroidism, Alzheimer’s, diabetes, muscle aches/spasms, nerve pain and depression. See below for my thyroid graphic – it is not uncommon to develop that condition 6 – 12 months after starting a statin drug!
There are hundreds of different side effects due to the depletion of these important nutrients, and every medication you take depletes more nutrients. If you don’t recognize the side effects, you’ll be diagnosed with a new disease.
Today, however, I am not going to debate the use of statins, or discuss their side effects and nutrient depletions. I’ve done that in the past – you can READ THIS on the dangers of taking a statin. Or THIS ARTICLE about how statins may contribute to a drug-induced hyperglycemia. And use my search box to find other articles.
Even though many health practitioners and health bloggers have ‘statin intolerance’ the fact remains that 25% of Americans rely on their statin medication to prevent a heart attack. Simply put, 1 in 4 people are worried about getting a heart attack. There are millions of people who are taking statins, and not planning to get off anytime soon. This article is for you.
I can make your statin work better!
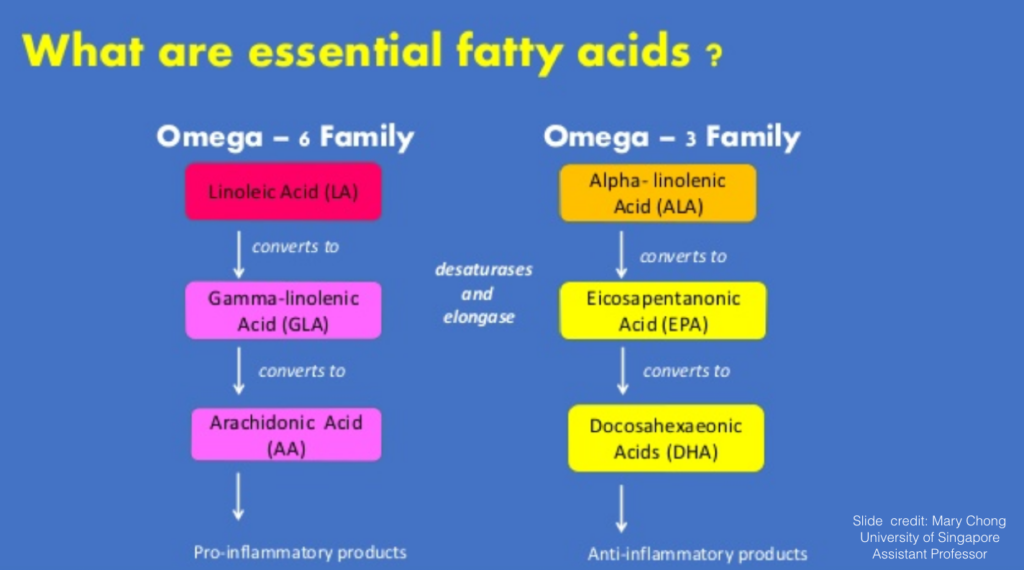
Fish oils play a role, but which one? Fish oils contain Essential Fatty Acids, or EFAs. Among the most famous EFAs are two called EPA and DHA. They have different roles, and can help you in so many ways. EPA converts to DHA in your body, and DHA is part of all your tiny cells.
Clarify the Myths
- Humans don’t make fish oils, we must get it from our diet.
- Fish oils contain both EPA and DHA.
- Humans don’t make EPA.
- Humans can make DHA, but it’s limited.
- DHA is a fatty component of cell membranes, EPA is not.
EPA (and DHA) are ANTI-inflammatory whereas Arachidonic Acid (AA) is PRO-inflammatory
The highest concentration of DHA is in the retina (eye) and the brain.EPA and DHA are both equally effective at reducing triglyceride levels. Both of these turn on a light switch in your body called “Peroxisome proliferator-activated receptor or “PPAR alpha.” When the PPAR switch is hit, a bunch of proteins start chemically speaking to each other, and chemical signals (in the form of enzymes like Pac-Man) are sent out to eat up the bad triglycerides and get rid of them.
DHA can increase LDL particle size a little bit better than EPA can, and you want that. The more dense LDL is, the more dangerous, so if DHA can “inflate” the LDL globules, it’s useful.
JELIS Study
JELIS Study
The results are in from the first large-scale, prospective, randomized trial that combined a statin with 1800 mg of EPA. The “Japan eicosapentaenoic acid (EPA) Lipid Intervention Study,” or JELIS Study, was conducted to evaluate and substantiate previous evidence of the benefits of fish oils.
Remember, Japan is an island nation, and its residents consume a diet that is rich in seaweed, fish, shellfish, squid and other marine life. The Japanese researchers have led many of the best trials using fish oils. On average, Japanese people eat about 3 ounces of fish each day, while typical Americans eat fish perhaps twice a week.
The purpose of the JELIS Study was to find out if EPAs would enhance a statin, or if a statin alone was enough. They were evaluating the clinical effectiveness of EPA oil in hypercholesterolemia patients that were also taking statins. Every person in the study was on a statin.
The investigators found men and women whose total serum cholesterol was ≥250 mg/dL. Those were the only people eligible. They were able to garner a total of 18,645 people (mean age, 61 years and 31% of which were male). Some of the folks had hypertension, diabetes or CAD. In other words, they had other issues, not just high cholesterol.
Every person in the study was on a statin. They were taking either pravastatin 10mg (trade name Pravachol), or simvastatin 5mg (trade name Zocor).
Some of the study participants were ALSO taking an EPA formulation called Epadel. This next part might make you scratch your head, but after you do that, please keep reading. The JELIS study was actually funded by Mochida Pharmaceutical, and they make Epadal (the EPA drug used in this study).
So it could be argued that there was a conflict of interest being that the maker funded a study on their own EPA drug, which is a slightly morphed version of regular fish oil supplements. Can you believe their results since the JELIS trial was self-funded?
I understand the benefits of EPA (and DHA) and the mechanism of action by which fish oils work, so my expectation is that there would be good results on these agents, regardless of who funds the study. And they spent a lot of money too, there were over 18,000 people involved! If their study was to simply promote their own drug, they could have used 250 people and drawn the same conclusion and spent far less! Just my opinion.
Just FYI, only two prescription formulations of highly purified EPA (without DHA) are currently approved in the world. One is called Epadel and the other is Vascepa in the United States.
REDUCE-IT Study
Vascepa (icosapent ethyl) is a pure EPA ethyl ester derived from fish oil. It’s a medication manufactured by a company called Amarin, and their personally funded trial called REDUCE-IT showed unprecedented results last year!
They saw a 25% reduction in first time major adverse cardiovascular events (ie. like a heart attack for example.) Isn’t that incredible? Researchers saw a 25% reduction in cardiovascular death, nonfatal MI, stroke and unstable angina! As you can imagine, Amarin’s stock soared right after that was published.
The makers of this drug would argue that it’s different than regular fish oils sold at health food stores, and yes, that is a true statement. You will not find “icosapent ethyl” in any health food store. This is the generic version of Epadel and Vascepa. These drugs start out as fish oil, then they get purified and chemically altered to form a new type of fish oil that gets patented, and sold as a drug.
It’s a little confusing at times. Keep in mind that both EPA and DHA are in regular supplements, so if you look at your fish oil at home, you’ll see both EPA and DHA listed on the Supplement Facts box. Just FYI, the two trials I mentioned above were essentially self-funded using medications that they themselves manufacture, not fish oils from a health food store.
I don’t know if you need Epadel, or Vascepa… or any prescriptionized fish oil. You can certainly have a discussion about this point with your own physician since these were the medications tested in the JELIS and REDUCE-IT trials, respectively.
You’ve probably noticed that the type of fish oil utilized in the study was pure EPA, not DHA. I just want to make that distinction. Theoretically, if you were trying to mimic this study, you could use a very high EPA (low DHA) brand.
Don’t be afraid of the DHA, that is what EPA converts to in your body.
Anyway, you can guess what happened. Lots of good things! The baseline total cholesterol for those 18,645 people was 275 mg/dL (on average), and their LDL (“bad”) cholesterol was 180 mg/dL. I’ve created a graphic here to show you the biomarkers they measured, the normal reference range, the baseline of the patients involved in the study, the reductions experienced by “Statin Only” and the reduction with “Statin plus EPA.” The reductions were the same in both groups.
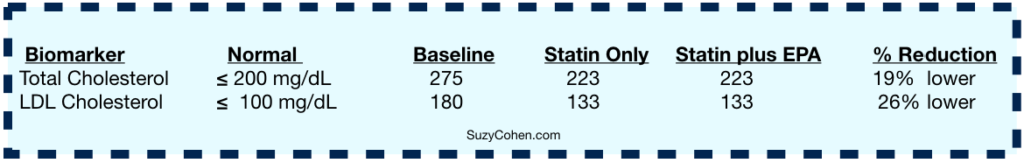
By the end of the study, both of those biomarkers came down. No surprise there, because we know that that is the job of a statin drug. And every participant was taking one. It didn’t matter if you took just a statin, or a statin and EPA fish oil… the same reductions were seen in both of those groups, and the cholesterol and LDL was reduced by the same amount. Triglycerides (not shown on my graphic above) were also reduced by the end of the JELIS study by 10% in the EPA group and 5% in the control group. No changes in HDL were noted.
This Part Was Unexpected
After 4 1/2 years, the most dangerous problems and potentially catastrophic consequences were significantly lower in a lot of the people who took EPA along with their statin. (The REDUCE-IT Trial showed similar results, as described earlier).
Their incidents were reduced in some cases by up to 28% – for example, in the group of people with unstable angina. The better outcomes varied among the groups, depending on the specific problem of course, and the person.
Dangerous Problems
Sudden cardiac death
Fatal MI (myocardial infarction)
Nonfatal MI
Unstable angina pectoris
Coronary Artery Bypass Graft (CABG)
Percutaneous Coronary Intervention (PCI) = Angioplasty with StentSide
Effects
Everyone experiences side effects when they take medication. In this landmark study, the group on the high-dose EPA fish oils did experience a few more problems such as GI side effects, skin rashes (allergy) and abnormal liver function tests.
I’m not trying to talk you out of EPA (or any fish oils) I just want you to be aware. And it would make sense too, after all, 1800 mg is A LOT of EPA! That’s like 4 or 5 times higher in the JELIS subjects, than in Americans who are taking these supplements! And remember, the JELIS subjects lived in Japan, where fish is the staple food, so they eat more EPA than Americans do. The REDUCE-IT Trial gave their participants 4000 mg (4 grams) EPA with a statin! That’s a huge amount of EPA!
If you look at labels for fish oil supplements, they are often in the range of 300 to 500mg EPA and/or DHA per soft gel.
I’m not advising any doses for any of you. I’m just giving you information, so please research and ask your doctor what is right for you when it comes to ANY changes in your drug/supplement regimen. And especially when it come to dosages.
That much EPA is not right for everyone and might cause problems for you, especially because fish oils are blood thinners and in combination with anticoagulants… it could cause itching, liver dysfunction, easy bruising, and hemorrhaging.
Statins are Drug Muggers of Omega 3 Fatty Acids
The part that is the most confusing variable here, and the big shocker is that statins are now thought to dampen the benefits of fish oils (essential fatty acids or EFAs). This little tidbit of information is not known by a lot of people, but it’s a very strong possible event that was shown 5 years prior when this ARTICLE was published in BMC Medicine.
The article states, “Statins favor the metabolism of omega-6 fatty acids (n-6), which in turn inhibits n-3 and, contrary to n-3, they increase insulin resistance and the risk of diabetes.”
There’s more.
Statins enhance production of arachidonic acid (AA), and that is an inflammatory compound!
The ratio of EPA to AA is critical. You want the EPA to be higher than the AA. But maybe not forever, which is why I worry about taking TOO MUCH, and too high of a dose, such as those in the trials. Ideally, if you’re measuring your labs, you want the ratio of EPA to arachidonic acid, (EPA/AA) to
be > 0.75.
Statins inhibit 3-hydroxy-3-methylglutaryl (HMG-CoA) Reductase, a step in cholesterol synthesis, so cholesterol is not formed as quickly; that’s how CoQ10 gets depleted from one’s body, causing muscle aches/spasms and pain. But the point I’m making today is that statins appear to ENHANCE production of arachidonic acid (AA). This stimulation is independent of HMG-CoA reductase mechanism of action which lowers cholesterol.
So if statin medications raise AA, and EPA lowers that, it makes you wonder how much BETTER the study trial results would have been… and how much better the people’s results would have been… if there was an arm of the trial that was EPA only, without a statin.
The statin raises AA, and EPA reduces it. They argue with each other in yet another way.
EPA is an inhibitor of delta 5-desaturation which reduces inflammation. Statins enhance this pathway according to THIS STUDY.
The ratio of EPA to AA in your body is very important – that’s the message I’d like to get out there. You want the EPA to be higher than the AA so taking a high EPA fish oil is what works.
What does this mean for you?
The implications of The JELIS and REDUCE-IT Studies mean that a combination of EPA plus a statin could produce a greater reduction in major coronary events. No one is saying this combo necessarily prevents a heart attack. Simply put, the fish oil with the drug work better together at minimizing the risk of dangerous complications of heart disease, and for that matter, diabetes, hypertension and hypercholesterolemia.
The question everyone wonders is WHY?
Why do fish oils appear to help reduce major coronary complications? It didn’t have much to do with the statin, which lowers cholesterol. So what other mechanism was it?
EPA increases PGI3 (Prostaglandin I3) which not only inhibits platelet aggregation (keeps the blood thin) and vasoconstriction (keeps vessels wide open), but also is assumed to reduce cardiac ischemic injury and arteriosclerosis.
The beneficial effects of EPA in reducing cardiac complications could be mediated by several biological actions, one of which comes from the ramped up production of PGI3, and the regular effect we know of which is lowering triglycerides.
Compared with DHA, EPA administration increases the EPA/AA ratio and likely the progression of CVD. There is more about EPA/AA and mechanisms in this STUDY, published in the Journal of Atherosclerosis and Thrombosis. Ideally, to reduce cardiac complications, the literature suggests that you shoot for the ratio of EPA to arachidonic acid, (EPA/AA) to be > 0.75.
You want the EPA level to be greater than the AA, and the ratio of those two biomarkers to be greater than 0.75.
It’s the ratio of these two biomarkers (AA and EPA) that is more predictive (at least in my opinion) of a heart attack, than cholesterol. CRP plays a role and I will write about that soon. CRP stands for Creactive Protein.
See the graphic below. The omega 6 fatty acid “Arachidonic Acid” is pro-inflammatory when it is produced or eaten in excess. You make it naturally in your body. EPA is an omega 3 fatty acid. It is anti-inflammatory and is not made in the body – you take it in supplemental form, or from eating foods high in omega 3 fats.
The lead investigator, Professor Yokoyama, MD, PhD, spent some time pondering why EPA has this astounding effect. After adjusting for age, genes and other prevention strategies, he found an inverse correlation between the risk of major coronary events to the ratio of EPA to Arachidonic Acid. In the literature, you see research about EPA/AA ratios.
Professor Yokoyama suggested that the benefits of EPA (with statins) were present due to the anti-thrombotic and anti-inflammatory effects of the agent… again, due to improving the EPA/AA ratio, which then goes on to “increase the stability of the atherosclerotic plaque.”
The President of the American Heart Association, Robert Eckel, MD (University of Colorado Health Sciences Center, Denver) makes a good point. He suggests that the JELIS Study results might be hard to transpose onto a Western population. He has stated, “An important consideration is that the dose of omega-3 fatty acids, 1800 mg a day of highly EPA, is more than the standard over-the-counter supplement [in the United States].”
The American Heart Association
The American Heart Association’s official stance on the topic of heart disease and Omega 3 EFA intake is basically this: A dietary approach to increasing omega-3 fatty acid intake is preferable to supplements, but this may not be possible for patients with CAD, who need to increase their intake to about 1000 mg per day for CHD [Coronary Heart Disease] risk reduction.
The AHA statement emphasizes the need for “high-quality omega-3 fatty acid supplements, free of contaminants.”
The AHA does not endorse any specific medication or supplements. What you take is up to you and your practitioner.
If you take a statin medication right now, ask your doctor if he/she thinks a high-dose EPA fish oil supplement would be the right thing for your situation. There are brands sold at health food stores, and online that are high quality.
The question may come up from some of you: What if I take fish oil that contains DHA?
The JELIS Trial and the REDUCE-IT Trial used an EPA-only drug, Epadel and Vascepa, respectively. These are purified fish oils that require prescription and do not contain any DHA. That does not make DHA a bad supplement to include, nor does it mean you should be worried.
Add more EPA – It Can Help Your Statin
You can add more EPA to your regimen, or alternate every month if you’d like. You can talk to your doctor about the medications. Keep in mind the studies were conducted by the drug maker themselves, so they used their own medication version of fish oil. That doesn’t mean the brand you take is necessarily wrong for you, especially if you’re feeling strong and healthy, and your triglycerides and ratios are good.
You can ask about the ethyl ester EPA medications if you prefer… if only for insurance purposes, or because that’s what was used in the clinical trials.
The take-home point is that statins alone may not be enough to protect you from heart disease.
People ask what I think all the time. If you really want to know, I think that lifestyle changes (less alcohol/nicotine/junk foods), consumption of lean, clean ‘real’ food and mild exercise are my #1, #2 and #3 recommendations for people with hypertension and hypercholesterolemia.
Supplements too! I’m a believer in fish oil, I personally take different brands, including my own. I think there’s a place for high-EPA fish oils, and high-DHA fish oils, as well as combinations.
Besides fish oils, there are other essential fatty acids that have amazing benefits too. They won’t all have DHA or EPA like fish oils, but they have other benefits. Read my article HERE about my favorite essential fatty acids.
My blog is just my opinion, and not intended as medical advice. Let me put it all together now with some current thoughts (now in 2024).
Updating our understanding of the interaction between statins, arachidonic acid (AA), and eicosapentaenoic acid (EPA) is crucial, so let me summarize it now.
Statins are blockbuster drugs, always at the top of worldwide sales. They are known primarily for their role in lowering cholesterol by inhibiting the enzyme 3-hydroxy-3-methylglutaryl-coenzyme A reductase (which is abbreviated HMG-CoA reductase), and these drugs have complex biological effects beyond simple cholesterol management.
It’s well-documented that while they reduce the synthesis of cholesterol in your body, statins paradoxically increase levels of arachidonic acid, a precursor to various eicosanoids, which are potent mediators of inflammation.
Recent research suggests that the increase in AA induced by statins could be linked to enhanced phospholipase A2 activity, an enzyme responsible for the cleavage of fatty acids from the cell membrane phospholipids, thus freeing AA. This mechanism is independent of the cholesterol-lowering action of statins and highlights a potentially pro-inflammatory side effect of statin therapy that could undermine (or at least compete with) its cardiovascular perks.
Importance of the EPA/AA Ratio
The balance between omega-3 fatty acids like EPA and omega-6 fatty acids like AA is critical in managing inflammation. Unfortunately, only the very, very best doctors understand this and treat patients accordingly. That’s why I wrote this blog, I want YOU to have the information.
EPA serves as a competitive inhibitor of AA metabolism, thereby reducing the formation of inflammatory eicosanoids derived from AA. The ideal EPA/AA ratio in blood lipid profiles is now considered a significant biomarker for inflammation and cardiovascular risk. It can be measured with a blood test.
Recent findings recommend maintaining an EPA/AA ratio greater than 0.75 to effectively counteract the pro-inflammatory effects of AA. This ratio is achievable through dietary changes (increasing intake of EPA-rich foods like fatty fish) and supplementation with high-quality fish oils. However, as pointed out, excessively high doses of EPA—such as those used in clinical trials—might not be necessary or beneficial long-term. Monitoring this ratio through regular blood tests can help tailor individual dietary and supplement plans to optimize your heart health.
Revisiting Clinical Trial Designs
Reflecting on past clinical trials which I discussed above, involving statins and EPA, it’s evident that isolating the effects of EPA could provide clearer insights into its benefits. Most trials have traditionally tested combinations! Meaning combinations of a statin medication with or without omega-3 supplements, but few have examined the impact of high-dose EPA alone in the absence of statins. Such studies could potentially demonstrate how EPA alone might influence AA levels and overall inflammation.
CoQ10 Depletion and Muscle Health
The relationship between statin use and CoQ10 depletion remains a critical concern, as CoQ10 is vital for energy production and muscle health. Statin-induced muscle pain and spasms could be mitigated by supplementing with CoQ10, or its more biologically active relative “Ubiquinol.” Taking this nutrient will help prevent uncomfortableside effects, especially those related to muscles, mood and energy. I never like to hear of someone taking a statin without ubiquinol! I assume they might be very tired, hypothyroid, probably forgetful, sad and riddled with pain or muscle spasms/cramps.
Conclusion
As we continue to explore the complexities of statins, EPA, and AA, it’s clear that a more personalized approach to managing these interactions is necessary. Adjusting EPA intake to manage the EPA/AA ratio effectively, considering CoQ10 supplementation for those on statins, and advocating for clinical trials that isolate the effects of EPA are all strategic moves toward reducing inflammation, and ultimately optimizing your heart health.

Suzy Cohen, has been a licensed pharmacist for over 30 years and believes the best approach to chronic illness is a combination of natural medicine and conventional. She founded her own dietary supplement company specializing in custom-formulas, some of which have patents. With a special focus on functional medicine, thyroid health and drug nutrient depletion, Suzy is the author of several related books including Thyroid Healthy, Drug Muggers, Diabetes Without Drugs, and a nationally syndicated column.