What's On This Page?
ToggleWhen you see or smell weird things it can be scary and unsettling. It is sometimes caused by temporal lobe seizures or migraines. The seizures are not the type that you might be thinking of that you see in movies, or in people with epilepsy meaning there are no convulsions or falling to the floor. They are more subtle than that, sometimes you do not even realize it’s happening to the person.
People with temporal lobe seizures may get episodes where they smell something bad, or they close their eyes and they see flashing lights.
The first time I heard of a person smelling something “bad” that wasn’t actually there was when I worked in long-term care facilities in the 1990s. I knew several patients that would say they smelled “burned rubber” “mold” or “something rotten” in the room, and asked if I smelled it too. I did not.

These people were perceiving the smell of something that simply wasn’t there. Two of the three also had visual problems primarily upon closing their eyes. They would see flashing lights of different colors. It didn’t happen all the time, but it happened enough to cause concern, leaving the patient feeling very unsettled.
They did not have seizures, they just saw or smelled weird things and it was not like a hallucination that a mentally ill patient might have.
I worked with the physicians for these facilities to make sure that the patients were well taken care of. Sometimes we would use carbamazepine, and sometimes phenytoin. These drugs belong to the category of anti-epileptics and they reduce the frequency of temporal lobe seizures which is one cause of these symptoms.
Phantosmia
Phantosmia is the medical term for the perception of an odor that is not actually present. It is also known as an “olfactory hallucination.” The phantom odor can be perceived as pleasant or unpleasant and can vary in intensity. It may occur in just one nostril, or it could be bilateral (as it often is with some schizophrenic patients).
To be clear I should distinguish phantosmia from another syndrome called parosmia, which is where there is actually an odor present, but it is perceived in a distorted way. With phantosmia, there is no odor present.
Some possible causes of phantosmia include:
- Upper respiratory infection or sinusitis
- Head injury or trauma like a TBI
- Exposure to certain chemicals or toxins
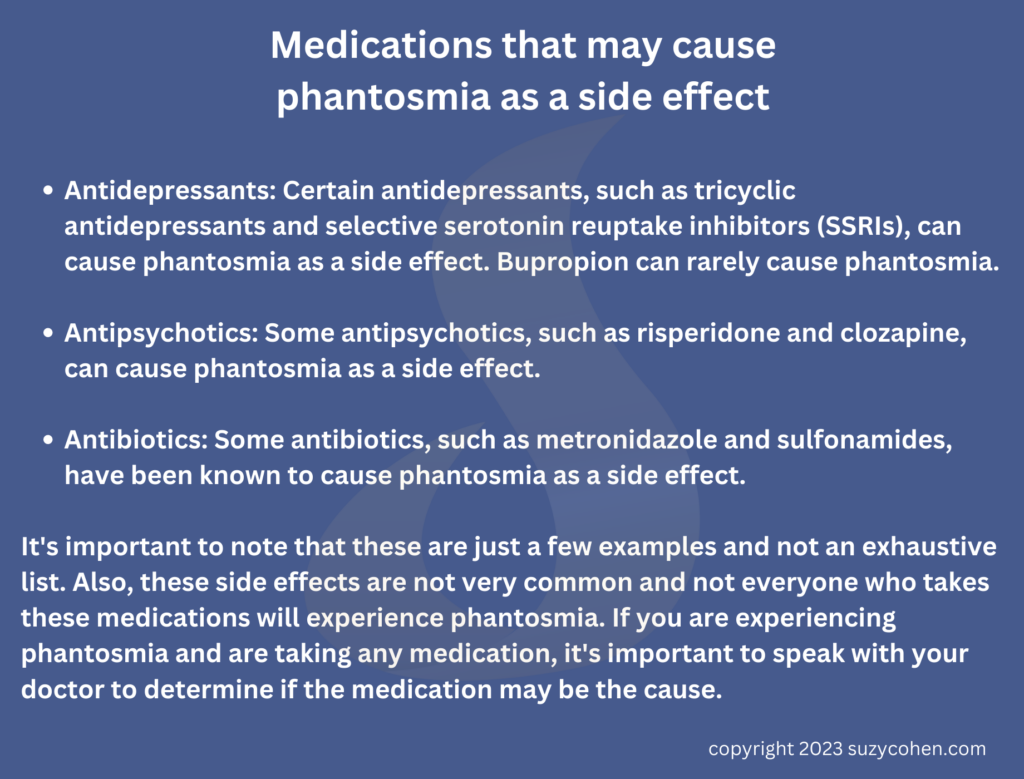
- Certain medications
- Neurological disorders such as Parkinson’s disease or multiple sclerosis
- Certain types of tumors (olfactory neuroblastoma)
- Certain types of olfactory nerve damage or dysfunction
- Infections
If you are experiencing phantom odors and it is affecting your quality of life, I recommend you see a specialist in the ear, nose, and throat (ENT) for evaluation in case the nasal passages are inflamed, or in case it is an infection. I wrote an article recently about a SINUS FUNGAL BALL infection.
A sinus fungal ball infection isn’t the only one either. There are several infections that can cause phantosmia – the perception of phantom odors. Lyme disease, an infection caused by a bacteria called Borrelia burgdorferi that is transmitted through tick bites, can cause an array of symptoms including phantosmia. Lyme is something that could in theory lead to intermittent bouts of phantosmia and photopsia.
Finally, meningitis is a serious infection of the membrane that covers the brain and spinal cord. It can cause inflammation in the olfactory nerve which can cause phantosmia but this is not something that would cause bouts of phantosmia that you have to deal with periodically, it’s a serious infection that you would know about and be hospitalized for!
Neuropathy Can Cause Bad Smells!
There is a potential correlation between phantosmia and neuropathy, as some studies have suggested that changes in the sense of smell can be an early sign of certain types of neuropathy.
Peripheral neuropathy, which is a type of neuropathy that affects the peripheral nerves, can cause damage to the olfactory nerve, which is responsible for the sense of smell. This damage can result in phantosmia, as well as other smell disorders, such as anosmia (loss of smell) or dysosmia (distorted sense of smell).
Additionally, some studies have suggested that phantosmia can be a symptom of other neurological conditions such as multiple sclerosis, brain tumors, and Alzheimer’s disease, which can cause neuropathy.
Small fiber neuropathy – which is a little different than peripheral neuropathy – can cause phantosmia.
The small nerve fibers, also known as C-fibers, innervate the olfactory nerve. The olfactory nerve is made up of specialized sensory cells called olfactory receptor neurons, which are located in the lining of your nasal cavity. These cells have small nerve fibers, called cilia which are hair-like structures, that project into the nasal cavity and detect odors. These cilia are responsible for transmitting the electrical signals to the brain that help you determine what an odor is.
Damage to small nerve fibers will result in a loss of or distorted sense of smell, including phantosmia. You may be interested in reading my article, Small Fiber Neuropathy Causes and Treatment.
It’s important to note that a correlation does not necessarily mean causation. Further evaluation by a neurologist is needed to determine if there is a direct relationship between phantosmia and neuropathy.
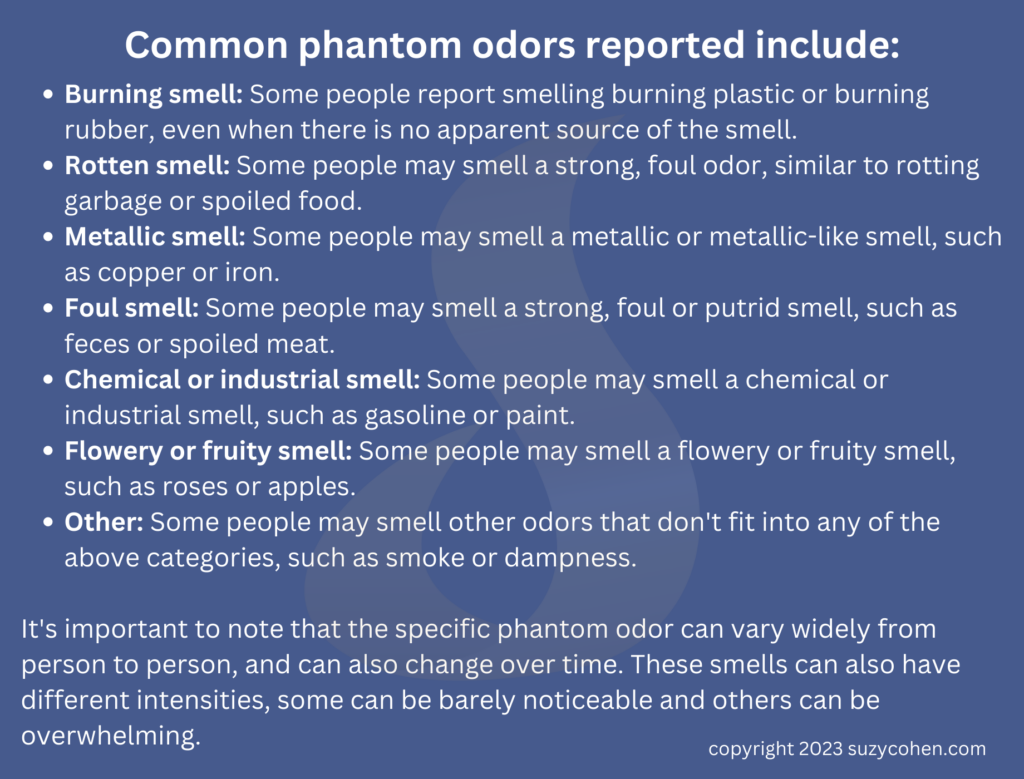
Examples of phantosmia odors can vary widely, but here are some of the reported odors:
- Burning smell
- Rotten food
- Metallic odor
- Foul smells like feces or something putrid
- Chemicals, gas or paint
- Flowery or fruity smell
- Smoke
Photopsia
Photopsia is the medical term for the perception of flashing lights or sparks. It can also refer to visual disturbances that resemble flickering or flashing lights, flashers, and floaters. Here is a good article explaining more about PHOTOPSIA.
Photopsia can be a symptom of an underlying condition or disorder.
Some possible causes of photopsia include:
- Migraine headaches, especially when accompanied by other migraine symptoms such as a headache, nausea, and sensitivity to light.
- Ocular migraines
- Retinal detachment or other eye disorders such as retinal artery occlusion, retinal vein occlusion, and age-related macular degeneration
- Neurological disorders such as epilepsy, MS (multiple sclerosis), brain tumors, and more
- Side effects from meds like antipsychotics, antidepressants, and even some antibiotics
- Vitamin deficiencies, especially vitamin B12
- Alcohol or drug abuse
It’s important to note that in some cases, the cause of photopsia is not known. If you are experiencing photopsia please see a doctor or an ophthalmologist for further evaluation.
Vitamin Deficiencies that Lead to Photopsia or Phantosmia
Vitamin B12 is a water-soluble vitamin that is essential for the normal functioning of the nervous system and the production of red blood cells.
A deficiency in Vitamin B12 can cause a wide range of symptoms, including fatigue, weakness, constipation, loss of appetite, weight loss, nerve damage, and anemia. In some cases, a Vitamin B12 deficiency can also cause visual disturbances such as photopsia, as well as other visual symptoms such as blurred vision, double vision, and color vision changes.
Vitamin B12 deficiency is most commonly caused by a lack of intrinsic factor, which is a protein that is required for the absorption of Vitamin B12 from the gut. It can also be caused by a lack of Vitamin B12 in the diet, or by conditions that affect the small intestine, such as celiac disease, Crohn’s disease, or surgical removal of a part of your stomach or small intestine.
Those who follow a vegetarian or vegan diet have a higher risk of developing Vitamin B12 deficiency as natural sources of this vitamin are found mostly in animal-derived products.
Vitamin B12 is manufactured in the GI tract by your natural microflora (probiotics). You can also supplement with it and “methyl” B12 is methylated as opposed to “cyano.” There are other good forms of B12 such as hydroxy and adeno B12.
There are other vitamin or mineral deficiencies that can cause these olfactory and visual symptoms (or others that negatively affect the nervous system). For example, a deficiency in vitamin A can cause night blindness and dry eyes, and a deficiency in thiamine (vitamin B1) can cause peripheral neuropathy and olfactory dysfunction.
A deficiency in copper, ZINC, and MAGNESIUM can also cause neurological symptoms, including visual disturbances. Additionally, deficiencies in iron, folate, and VITAMIN D can contribute or cause anemia, which is also associated with visual disturbances and various other neurological symptoms.
High doses of vitamin B6 can potentially cause neurological symptoms like seizures or problems in the temporal lobe. More is not better. However, this is typically only seen with very high doses of these vitamins, which are much higher than the recommended daily intake, usually injections or multiple tablets. It is important to follow recommended dosage guidelines on your label and consult with a healthcare professional before taking any dietary supplement, especially if you are pregnant or have a medical condition.

Diagnosis & Treatment of Temporal Lobe Seizures
It is important to note that these deficiencies would have to be pretty severe in order to cause chronic bouts of phantosmia and photopsia. It’s more likely that the cause is temporal love seizures, and it’s important to consult with a neurologist to get a proper diagnosis. They will of course send you out for blood tests to check for deficiencies in vitamins and minerals as part of the initial workup.
An EEG (electroencephalogram) is a test that records the electrical activity of the brain, and it is commonly used to diagnose seizures, including those involving the temporal lobe. An EEG can show the characteristic abnormal electrical activity that occurs during a seizure, called a seizure discharge or spike-and-wave pattern. This abnormal activity can be seen in the temporal lobe or other regions of the brain depending on the type of seizure.
Temporal lobe seizures are typically treated with medication, specifically antiepileptic drugs (AEDs). The goal of treatment is to reduce the frequency and severity of seizures and to prevent the development of other seizures. There is more you can read about in this MAYO ARTICLE.
The most commonly used antiepileptic drugs for temporal lobe seizures include:
- Carbamazepine (Tegretol)
- Valproic acid (Depakene)
- Lamotrigine (Lamictal)
- Phenytoin (Dilantin)
- Levetiracetam (Keppra)
- Topiramate (Topamax)
- Zonisamide (Zonegran)
It’s important to note that the specific antiepileptic drug and dosage will depend on the individual’s needs and the type of temporal lobe seizure they are experiencing, as well as age, kidney/liver function and other medications that are being taken at the time. Your practitioner will work with you to find the best medication or combination of drugs that will control (or at least minimize) your seizures with the least amount of side effects.
In some cases, if a person has not responded to multiple AEDs, or if the seizures are particularly severe and frequent, surgery may be considered. Surgery for temporal lobe seizures typically involves removing the part of the brain where seizures originate.
Other treatments that can also be helpful for people with temporal lobe seizures include:
- Vagal nerve stimulation (VNS) is a type of therapy in which a small device implanted under the skin in the chest sends electrical pulses to the brain via the vagus nerve.
- The ketogenic (“keto”) diet, which is a high-fat, low-carbohydrate diet can help reduce seizures in some people with epilepsy. Before you say you don’t want to give up bread, let me tell you I’ve seen this work in several patients who were very strict about their diet (ie no cheats).
One person was able to reduce the frequency from 4-5 seizures a week to about 1 every 3 months. The other person who converted to keto reduced seizures from once per month to one every 6 months. A low-sugar, low-carb (and high-fat) is healing to the brain and can be the first, the easiest, and the cheapest thing you can do to reduce seizure frequency! - Pancreatic conditions indirectly play a role. Seizures and problems of the temporal lobe are not directly caused by pancreatic atrophy, however, there may be a correlation between the two conditions. Seizures can be caused by a variety of conditions, including metabolic imbalances and nutritional deficiencies, which can result from chronic pancreatitis, a condition in which the pancreas becomes inflamed and damaged over time, leading to pancreatic atrophy.Additionally, there are also some cases where people with chronic pancreatitis and pancreatic atrophy also have a coexisting neurological disorder or an autoimmune condition that impacts the temporal lobe and triggers seizures. It is important to consult with a healthcare professional if you have been diagnosed with pancreatic atrophy or chronic pancreatitis and if you are experiencing seizures or problems of the temporal lobe, as there may be other underlying causes that need to be addressed.
- Antibiotics for infections may be needed.
- If the cause of phantosmia is related to neurological causes, or small fiber neuropathy (or diabetes), Alzheimer’s disease or Parkinson’s disease, then medications for those conditions will be warranted.
It’s important to note that not all people with temporal lobe seizures will require surgery. The best treatment option will depend on the individual’s specific situation and the type of seizures they are experiencing.
What About America’s Favorite Recreational Plant Marijuana?
Cannabidiol (CBD) is one non-psychoactive portion of the marijuana plant. It is a chemical compound that reduces pain and inflammation. It does not make you high. Today you can find CBD all over the place, especially in creams for arthritis. Some research suggests that CBD may have therapeutic potential for treating certain types of seizures, including temporal lobe seizures.
A study from 2018, published in The Lancet Neurology, found that CBD-enriched cannabis extract, when added to traditional antiepileptic therapy, resulted in a significant reduction in the frequency of seizures in people with treatment-resistant epilepsy, including temporal lobe epilepsy.
Another study from 2017, published in the Journal of Clinical Pharmacy and Therapeutics, found that CBD may have anticonvulsant properties, and could be useful in the treatment of temporal lobe seizures.
However, it’s important to note that more research is needed to fully understand the effects of CBD on temporal lobe seizures, and the studies conducted so far have been small and mostly open-label, which means that the results may be influenced by placebo effect or bias.
It’s also important to note that CBD is not yet FDA-approved for the treatment of seizures and its use is widespread, but still considered experimental by conventional physicians. So it’s important to consult with a neurologist or physician who is skilled in using this treatment before pursuing CBD as a treatment option — just to understand the legal and safety implications of using it in your state, for your particular seizure disorder.

Summary
In summary, a temporal lobe seizure is a type of seizure that originates in the temporal lobe of the brain and can cause a variety of symptoms such as sensory disturbances, emotional changes, auditory or visual symptoms, difficulty speaking, confusion, and memory loss. They are typically treated with antiepileptic drugs and in rare cases (if the seizures are particularly severe and frequent), surgery may be considered.
Phantosmia is the perception of an odor that is not actually present and can be caused by various things such as upper respiratory infections, head injury, exposure to certain chemicals or toxins, certain medications, neurological disorders, certain types of tumors, olfactory nerve damage or dysfunction and depression or anxiety.
Photopsia is the perception of flashing lights or sparks, it can be caused by migraine headaches, retinal detachment or other eye disorders, neurological disorders, side effects of certain medications, and vitamin deficiencies, specifically of vitamin B12, long-term alcohol or drug use.
In addition, a deficiency in Vitamin B12 can cause visual disturbances such as photopsia, as well as other visual symptoms such as blurred vision, double vision, and color vision changes. Deficiencies in Vitamin A, thiamine, copper, zinc, magnesium, Iron, Folate, and Vitamin D can cause neurological symptoms as well.
Temporal lobe seizures are one common cause of symptoms like phantosmia and photopsia. Getting proper treatment for the condition can limit the frequency of episodes that you have. Seeing an ophthalmologist, ENT doctor, and neurologist is important in order to have a complete workup. Usually, anti-epileptic drugs are used if the person is found to have temporal lobe seizures. Diet is critical and so is the evaluation of vitamin and mineral status.
Symptoms of a temporal lobe seizure can include:
- Sensory disturbances, such as a sudden, strange smell or taste
- Déjà vu or hallucinations
- Emotional or mood changes, such as fear or unexplained anxiety
- Auditory symptoms, such as hearing noises, or voices
- Visual symptoms, such as seeing flashing lights or hallucinations
- A feeling of rising or falling similar to a drop attack
- Numbness or tingling in your face or body
- Difficulty speaking or being able to articulate words
- Difficulty understanding speech or temporary confusion
- Loss of consciousness
- Memory loss or feeling bewildered after the episode
It’s important to note that these symptoms can vary widely and may not all be present during a single seizure. It is important to consult a doctor if you suspect you or someone you know may be experiencing seizures.

Suzy Cohen, has been a licensed pharmacist for over 30 years and believes the best approach to chronic illness is a combination of natural medicine and conventional. She founded her own dietary supplement company specializing in custom-formulas, some of which have patents. With a special focus on functional medicine, thyroid health and drug nutrient depletion, Suzy is the author of several related books including Thyroid Healthy, Drug Muggers, Diabetes Without Drugs, and a nationally syndicated column.