What's On This Page?
ToggleIf you’ve recently been told that your LDL, triglycerides, or overall cholesterol levels are creeping into an unhealthy range, it’s a wake-up call to adopt healthier habits for better cardiovascular health. As a pharmacist who understands both the conventional and natural sides of medicine, I want to empower you with actionable strategies that can make a difference in your lipid profile and overall well-being.
By the way, there are many synonyms for cholesterol, and I will be using some of these throughout my blog so I don’t have to say “cholesterol” a hundred times. You may have heard of it as one of these in the past.
Synonyms for Cholesterol
- Lipids
- Blood fats
- LDL/HDL (when specifying cholesterol types)
- Serum lipids
- Blood lipid levels
- Hypercholesterolemia (meaning your levels are above normal reference ranges)
Sometimes hypercholesterolemia has to do with hypothyroidism, and if that’s the case you need to be aware of this so you can treat the underlying cause. At the end of this article, I discuss the connection to your thyroid gland and answered a reader’s question. In the meantime, here are 10 ways to address your imbalanced serum lipid ratios:
1. Increase Soluble Fiber Intake
Soluble fiber binds with cholesterol in the intestines, helping to eliminate it before it’s absorbed into the bloodstream. This means eating more oats, beans, lentils, flaxseeds, and fruits like apples and berries. A meta-analysis published in the American Journal of Clinical Nutrition found that increased soluble fiber intake reduced LDL cholesterol by approximately 5-10% (Brown et al., 1999). Researchers found that increased soluble fiber intake reduces LDL levels. Specifically, the study found that an average intake of 2-10 grams per day of soluble fiber was associated with a modest reduction in LDLs (approximately 5-10%), depending on the type and amount of fiber a person consumed.
The precise reduction varies based on the type of soluble fiber (such as psyllium, pectin, oat bran, or guar gum) and the dosage, but overall the study concludes that increasing soluble fiber has a favorable effect on LDLs.

2. Incorporate Omega-3 Fatty Acids
Omega-3 fatty acids are found in fatty fish like salmon and sardines, as well as in flaxseed and chia seeds. These healthy fats reduce triglycerides and raise HDL (“good”) cholesterol while supporting heart health by reducing inflammation. Consuming fatty fish twice a week or supplementing with high-quality fish oil can make a noticeable difference.
3. Exercise Regularly – Aerobic & Resistance Training
Regular exercise is one of the most powerful lifestyle changes for cholesterol management. Combining aerobic activities (such as walking, swimming, or cycling) with resistance training helps raise HDL and lower LDL and triglycerides. Aim for at least 150 minutes of moderate exercise per week.
4. Reduce Refined Carbohydrates and Sugar
Diets high in sugar and refined carbohydrates can elevate triglycerides and lower HDL cholesterol. Replace processed foods, white bread, and sweets with whole grains like quinoa, brown rice, and oats. Emphasize a diet rich in whole foods like vegetables, legumes, nuts, and seeds to support better lipid ratios and levels.
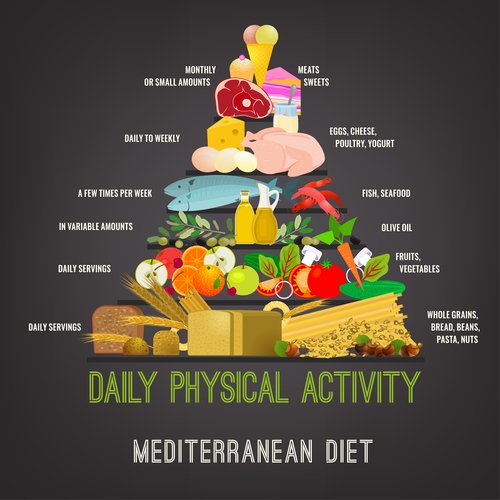
5. Adopt a Plant-Based, Mediterranean Diet
The Mediterranean diet emphasizes vegetables, fruits, whole grains, nuts, legumes, fish, and olive oil. This diet is rich in monounsaturated fats (from olive oil) and antioxidants, which help lower LDL cholesterol while maintaining a healthy balance with HDL. This way of eating is not just heart-healthy but also supports overall wellness and longevity.
6. Incorporate Phytosterols and Stanols
Phytosterols and stanols are naturally occurring compounds in plants that resemble cholesterol and block its absorption in the intestines. Foods like nuts, seeds, whole grains, and fortified products contain these compounds. A daily intake of around 2 grams of phytosterols and stanols can lower LDL cholesterol by about 10%.
7. Consider Red Yeast Rice Supplementation
Red yeast rice contains compounds similar to statin drugs, making it a natural option to reduce LDL cholesterol. However, it should be used under the guidance of a healthcare professional, as it can have effects similar to statins and may interact with other medications.
8. Eat Antioxidant-Rich Foods – Berries, Green Tea, and Dark Chocolate
Antioxidants help protect cholesterol from oxidation. This is a major step in plaque formation and artery hardening and that’s why I am always suggesting antioxidants. They help prevent us from ‘rusting.’ Berries like blueberries and strawberries, green tea (rich in catechins), and dark chocolate (loaded with flavonoids) are potent sources of antioxidants that support heart health and help with hypercholesterolemia.
9. Manage Stress Through Meditation and Yoga
Stress can raise serum lipids and triglycerides through its influence on fat metabolism. Practices like meditation, deep breathing, and yoga are powerful tools to reduce cortisol (the stress hormone) and improve lipid profiles. Even a daily practice of 10-15 minutes can have a positive impact on cholesterol levels and overall heart health.
10. Balance Key Minerals – Magnesium, CoQ10, and Vitamin D
Deficiencies in certain nutrients can impact cholesterol levels. Ensuring adequate intake of these minerals is crucial:
Magnesium: Magnesium plays a vital role in heart health, normal cholesterol levels, and blood pressure regulation. My Magnesium Glycinate is especially beneficial, as this form is highly absorbable and gentle on the stomach. It helps support muscle function, cardiovascular health, and calms the nervous system. If you’re dealing with statin-induced muscle cramps, chelated magnesium glycinate is a great option to support muscle health.
CoQ10: Coenzyme Q10 (CoQ10) is crucial for cellular energy production, especially in the heart and muscles. Statin drugs can deplete CoQ10 levels, potentially causing muscle pain or weakness. For those on statin therapy, supplementing with CoQ10 (preferably as ubiquinol, its active form) is highly recommended to maintain healthy energy levels and heart function.
Vitamin D: Vitamin D is essential for heart health, lipid regulation, and calcium-magnesium balance. Low levels are associated with increased cholesterol and poor cardiovascular outcomes. My Vegan Vitamin D is plant-based and a great option for those following a vegan lifestyle or seeking a clean source. By supplementing with this bioavailable form, you can support immune function, mood, and heart health without any animal-derived ingredients.
Medications That Can Raise Cholesterol Levels
Certain medications, commonly prescribed for various conditions, are known to raise cholesterol levels! A lot of folks don’t realize that, so since I am a pharmacist, I thought it was a good idea to write this next section for you. Checking your medicine cabinet for these medications can help you identify potential contributors to your cholesterol levels.
I’m not telling you to stop them, but I am suggesting that you discuss with your physician that they may be contributing to your current problem, which might be leading to a new medication for the side effect. You don’t want to be a dog chasing its tail.
- Beta-blockers: Used to treat high blood pressure and heart conditions, some beta-blockers can increase triglycerides and lower HDL cholesterol.
- Diuretics (Thiazides): Often prescribed for hypertension, these can elevate LDL cholesterol and triglycerides.
- Oral contraceptives and hormone replacement therapy (HRT): Estrogen-containing medications can raise triglycerides.
- Corticosteroids: These anti-inflammatory drugs, when used long-term, can increase triglycerides and LDL cholesterol. By the way, they can also do a number to your hip joint! Be wary of the fact that steroids (long-term use) can lead to avascular necrosis. No one talks about this until it’s too late.
- Immunosuppressants (like cyclosporine): Used to prevent organ transplant rejection, they can elevate blood fats.
- Anti-seizure medications (like carbamazepine): These can raise all of your lipids including your triglycerides levels.
If you are on any of these medications and notice changes in your cholesterol, it’s essential to discuss with your healthcare provider possible adjustments or alternative treatments.
The Drug Mugging Effect of Statin Drugs
Statin drugs are commonly prescribed to lower LDL cholesterol, but they can also deplete certain nutrients, particularly CoQ10 and Vitamin D, which are essential for energy production in muscles and the heart. These nutrient depletions may lead to side effects like muscle pain or weakness, affecting overall energy levels, muscle aches and pains, poor memory, depression and a loss in bone mass. While statins can be effective for cholesterol management, they don’t address root causes such as inflammation or lifestyle factors. If you take them, most doctors don’t mind if you add vitamins, omega-3s, and other natural adjunctive supplements. A comprehensive varied approach will work best at least IMHO.
For more on drug mugging and how statins deplete your “fountain of youth”hormone called DHEA, read THIS BLOG.
And also this one if you take medication for heartburn or reflux, Dangerous Drug Mugging Effect by Acid Blockers.
The Thyroid – High Cholesterol Connection!
One of the questions I received last week from a reader belongs to be answered in this blog so I’m going to answer it now. Here’s David’s question: Does Suzy agree that high cholesterol and hypothyroidism often present together? If so, is the link invalidated once the patient takes levothyroxine? I have often heard the former, but not the latter, so I wondered about this.
To answer this let’s first talk about the actual relationship between the thyroid gland and cholesterol. When you have thyroid disease, specifically an underactive thyroid (called hypothyroidism), your body doesn’t make enough thyroid hormones. These hormones help regulate your metabolism, which includes how your body uses and breaks down fats. A lot of people don’t even know if they have a problem with their thyroid gland because doctors just look at your lab test (which doesn’t always correlate with disease progression). Here’s a graphic with the symptoms in case you want to “see if it fits.”
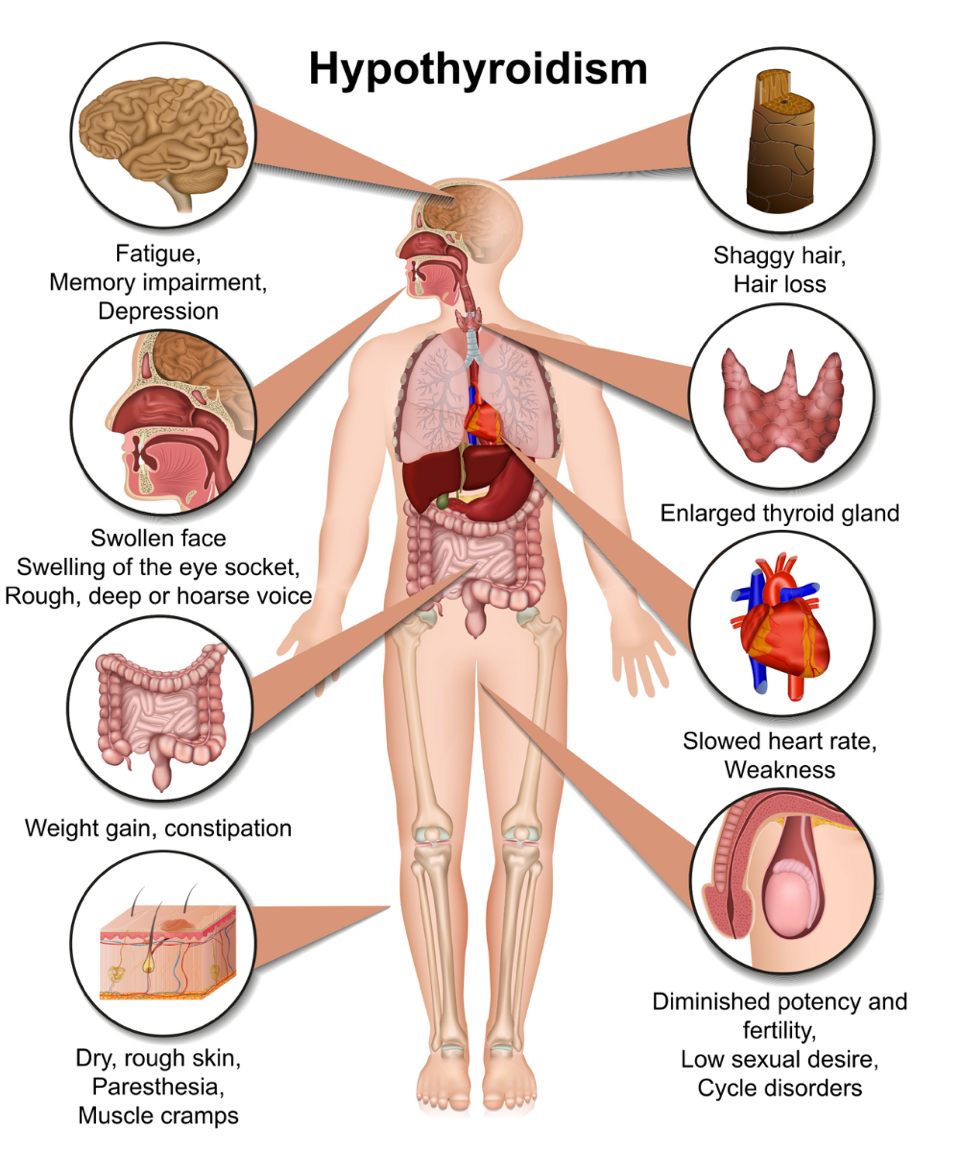
If your thyroid is not working well, your metabolism slows down, making it harder for your body to get rid of “bad” cholesterol (LDL). This can cause your serum lipid levels to rise. So, people with hypothyroidism often have higher cholesterol because their bodies can’t clear it out as effectively! Every have your disposal break in your kitchen sink? It’s annoying and gross, isn’t it? Just like water that can’t flow freely down a clogged drain, your lipid levels rise because they aren’t being cleared out efficiently.
So YES, I do agree that high cholesterol and hypothyroidism often present together. If not at first, then at some point down the road but it’s pretty inevitable. Hypothyroidism can slow down the body’s metabolism, which includes how your cholesterol is processed. When thyroid hormone levels are low, the liver struggles to break down and remove excess cholesterol, often leading to elevated LDL and total cholesterol levels.
Using the clogged drain analogy, levothyroxine works by potentially fixing one underlying problem: It helps “unclog” the drain by restoring proper thyroid function, which can improve the body’s ability to naturally regulate and clear out cholesterol more effectively. (Statins would slow down the water flow which contributes to the overflow using the same analogy).
However, even when a person starts taking levothyroxine (Synthroid®) to correct the hypothyroidism, the link is not always entirely “invalidated.” While levothyroxine can help restore normal thyroid hormone levels and potentially lower cholesterol, it doesn’t always lead to full resolution of the cholesterol issue because other factors come into play such as diet, lifestyle, genetics and innate production of cholesterol, not to mention how you clear/break down the smaller particles. I found an article on John Hopkins entitled, What to Do When High Cholesterol Runs in Your Family, in case that interests you.
In some people, cholesterol levels may improve significantly with proper thyroid hormone replacement, while others may continue to have high cholesterol for various reasons. Again, such as concurrent lifestyle factors, everything I mentioned a minute ago and also how well your body is responding to the medication. Herbal supplements can enhance drug effects. Read my other blog, 5 Surprising Ways Fig Fruit Extract Helps Glycemic Control and Cholesterol.
Therefore, it’s crucial to continue monitoring lipid levels even after starting levothyroxine may be necessary to fully address lipid imbalances. Working with an intelligent physician who understands all of this is the best way to manage both thyroid and cholesterol issues together.
Closing Thoughts
Lowering LDLs and triglycerides is crucial for cardiovascular health, but it’s important to approach this goal holistically. Dietary modifications, regular exercise, stress management, and nutrient balance are all powerful tools to improve lipid levels naturally. Remember, medication is only part of the solution—lifestyle is powerful medicine too. Correcting thyroid imbalances helps some people because hypothyroidism goes hand in hand with hypercholesterolemia.
Before making any changes to your diet, lifestyle, or medication regimen, please consult with your healthcare provider.

Suzy Cohen, has been a licensed pharmacist for over 30 years and believes the best approach to chronic illness is a combination of natural medicine and conventional. She founded her own dietary supplement company specializing in custom-formulas, some of which have patents. With a special focus on functional medicine, thyroid health and drug nutrient depletion, Suzy is the author of several related books including Thyroid Healthy, Drug Muggers, Diabetes Without Drugs, and a nationally syndicated column.