What's On This Page?
ToggleDo you live on antacids?! Let me tell you about my son Michael, who prides himself on his iron stomach. He likes to sample spicy food and will eat anything from Thai curries to Indian vindaloos, without so much as a hiccup.
One day, he went to a local Mexican restaurant in Orlando (The Ocoee Taco Company) and saw the challenge to beat the record set there, by eating more than 26 street tacos! If I had been there I would have staged a taco intervention!

With a grin and a shrug, he and his friend Garrett accepted the challenge. The waiter brought their tacos out! Michael ended up eating 20 tacos and Garrett 23!
The guys left the restaurant with as much composure as they could muster (being that the rumble in their tummies could rival a volcano), and drove to the nearest pharmacy to buy every antacid on the shelf! I suspect the fiery revenge of 20 tacos complete with salsa, took revenge on my son’s once-iron stomach!
On the upside, a photo of the two young men is posted on the restaurant wall as a testament to their efforts because they rank second and third place now, lol!
Now, the point of this story is that acid reflux is a pretty common ailment, one that is caused by various factors, including taco-eating challenges! Regardless of the “why,” if this problem becomes more than an occasional nuisance, you have to examine your diet, and probably cut out most of the foods you’re eating.
In the United States alone, approximately 20% of the population suffers from gastroesophageal reflux disease (GERD), a chronic form of acid reflux. This staggering statistic highlights the importance of understanding the various antacid options available in the market. Whether it’s traditional over-the-counter solutions or natural alternatives, each comes with its own set of benefits and precautions which I will discuss now.
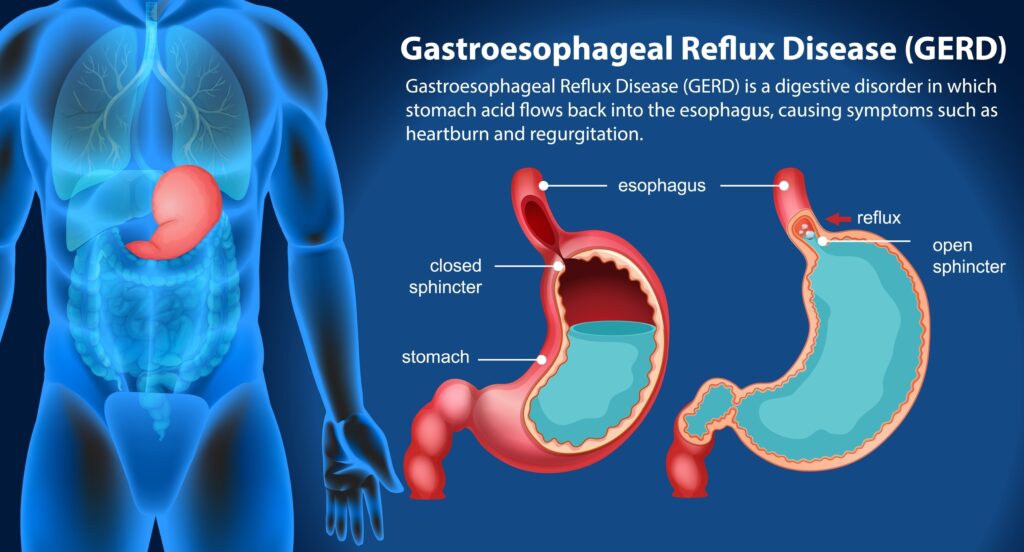
A Synopsis of GERD
Do you get GERD? This is essentially chronic acid reflux (or backflow) of stomach acid up into your esophagus. Do you know the symptoms of this condition? Because a lot of people have symptoms so mild they don’t even realize they have GERD for years.
- Heartburn: A burning sensation in the chest, often occurring after eating, which might worsen at night or when lying down.
- Regurgitation: A sour or bitter-tasting acid backing up into the throat or mouth.
- Dysphagia: Difficulty swallowing, feeling like food is stuck in the throat or esophagus.
- Chest Pain: Discomfort or pain in the chest area, which can sometimes be mistaken for heart pain.
- Hoarseness or Sore Throat: Irritation in the throat, often noticeable in the mornings.
- Chronic Cough: A persistent cough, which is often worse at night or when lying down.
- Laryngitis: Inflammation of the voice box (larynx) characterized by hoarseness or voice changes.
- Asthma Symptoms or Worsening Asthma: For some people, GERD can exacerbate asthma symptoms.
- Dental Erosion: Acid reflux can wear away the enamel on the teeth.
- Nausea: Some people with GERD experience nausea, though this is less common.
- Bloating, Belching, or a Feeling of Fullness in the Stomach: These symptoms can occur, often as a result of the stomach’s reaction to prolonged acid exposure.
I found this interesting too. A STUDY published in the Journal of Clinical Medicine suggests that people with celiac disease tend to experience more GERD than others, although they are unclear about why that would be.
If you live on antacids, you should be aware that some of them can interfere with the absorption of vitamins and minerals. They are very potent drug muggers of nutrients (all of them) because they alter the pH of your stomach, thus interfering with the absorption of everything, including nutrients extracted from food.
Also, chronic use of antacids can lead to gastroparesis which is delayed emptying of stomach contents. Finally, a lot of antacids and acid blockers (which are really the same thing) are able to produce a change in your system and cause gluten or dairy sensitivities.
Maybe you don’t have heartburn, or need antacids, but you have a condition called diverticulitis? Your 7 Step Guide: Herbal Remedies And Dietary Tweaks For Diverticulitis Relief.
Traditional Antacids
TUMS® (Calcium carbonate):
Benefits: TUMS, primarily composed of calcium carbonate, provides quick relief by neutralizing stomach acid.
Ideal For: People experiencing occasional, mild heartburn. If you know you’re going to get into some Thai green curry that is spicy, or some salsa, you can pop one of these in advance (about 15 minutes before you eat).
Caution: Not recommended for those with kidney problems due to its calcium content.
Zantac®:
Recalled as ranitidine, currently contains f”amotidine.”
See below for information on Pepcid (famotidine).
Pepcid AC (Famotidine):
Benefits: Unlike TUMS, Pepcid AC reduces the stomach’s acid production. It’s longer-lasting and more suitable for frequent heartburn.
Ideal For: Individuals with persistent acid reflux symptoms.
Caution: Those with kidney problems should consult a doctor before use.
Mylanta®:
Benefits: Combines antacids like aluminum hydroxide and magnesium hydroxide and something for gas (simethicone) to provide quick relief and create a protective barrier in the stomach. Just a quick note to tell you that Gaviscon® is another option but instead of having simethicone in it, it has alginic acid (aka “alginate”) which is there to help stop the backflow of acid into your esophagus (aka “food pipe”).
Ideal For: Quick relief from heartburn and gas. You could take a swig of this 15 minutes before eating two dozen buffalo wings or a bowl of Madras curry!
Caution: May interact with other medications due to its magnesium and aluminum content.
Pepcid® Complete:
Benefits: Pepcid Complete combines the acid-reducing effects of Famotidine (found in Pepcid AC) with antacids calcium carbonate and magnesium hydroxide. This dual-action formula offers both quick relief from heartburn and long-lasting prevention of acid production.
Ideal For: Individuals seeking immediate relief from heartburn, as well as lasting protection against recurring symptoms.
Caution: While beneficial for occasional heartburn, it’s not intended for long-term treatment of GERD without a doctor’s guidance. Excessive use can lead to side effects such as constipation or diarrhea due to its mineral content.
Nexium® (Esomeprazole):
Benefits: A proton pump inhibitor drug (PPI) that significantly reduces stomach acid production. PPIs are strong drugs and suppress acid for 24/7. They are most often used for people with GERD, or Zollinger-Ellison syndrome, a condition that requires more than a quick fix like TUMS®.
Ideal For: Patients with GERD or those needing long-term treatment for Zollinger-Ellison syndrome.
Caution: Long-term use can lead to magnesium deficiency and increased risk of bone fractures.

Prilosec® (Omeprazole):
Benefits: Prilosec is another brand of PPI that reduces stomach acid production. It is often used for treating GERD, stomach ulcers, and other acid-related conditions.
Ideal For: Patients who require a more powerful and long-term solution for acid reflux, especially those with chronic symptoms.
Caution: Long-term use has been associated with risks such as vitamin B12 deficiency, bone fractures, and kidney disease. It’s important to use it as prescribed and under medical supervision.
Protonix® (Pantoprazole):
Benefits: Another PPI, pantoprazole effectively decreases the amount of acid produced in the stomach. It’s particularly effective for erosive esophagitis and other severe forms of acid reflux disease.
Ideal For: Individuals with severe acid reflux symptoms or those diagnosed with esophageal damage due to acid reflux. Also commonly used for people with Zollinger-Ellison syndrome.
Caution: Similar to other PPIs, long-term use can lead to potential side effects like magnesium deficiency and an increased risk of infections like C. difficile. Regular monitoring by a healthcare provider is recommended.
Zegerid OTC (Omeprazole with Sodium Bicarbonate):
Benefits: Zegerid OTC combines omeprazole, a PPI, with sodium bicarbonate, an antacid. This combination not only reduces acid production but also neutralizes stomach acid quickly.
Ideal For: Those seeking both immediate and sustained relief from heartburn and acid reflux symptoms.
Caution: The sodium bicarbonate in Zegerid OTC can cause increased sodium levels, making it less suitable for individuals on a low-sodium diet or with certain cardiovascular conditions. As with other PPIs, long-term use should be medically supervised.
Natural Alternatives
1. Mastic Gum:
Benefits: Known for its anti-inflammatory and antibacterial properties, it can help soothe the stomach lining and reduce symptoms.
Ideal For: Those preferring natural treatments and suffering from mild symptoms.
Caution: Should be avoided by individuals with tree sap allergies.
2. Zinc Carnosine:
Benefits: A compound known to support the gut lining and promote healthy digestive function.
Ideal For: People looking for long-term gut health improvement.
Caution: Can interact with certain antibiotics and diuretics.
3. Marshmallow Root:
Benefits: Contains mucilage, which forms a protective layer in the
Ideal For: Individuals seeking gentle, herbal relief for occasional heartburn.
Caution: Not recommended for people with diabetes or those taking diuretic medications, as it may affect blood sugar levels and water balance.

4. Aloe Vera:
Benefits: Aloe Vera is known for its soothing and anti-inflammatory properties. When taken in juice form, it can help calm the stomach lining and reduce irritation caused by acid reflux.
Ideal For: Individuals looking for a gentle, natural remedy to ease gastrointestinal discomfort.
Caution: It’s important to use aloe vera juice that’s specifically prepared for internal use. Aloe Vera latex, found in some whole-leaf extracts, can be a potent laxative and should be avoided.
5. Apple Cider Vinegar:
Benefits: Although it might seem counterintuitive to treat acid reflux with an acid, Apple Cider Vinegar is believed by some to balance stomach acidity and aid in digestion.
Ideal For: Those who prefer a natural, holistic approach and may have mild symptoms.
Caution: Apple Cider Vinegar is highly acidic and should always be diluted before consumption. It’s not recommended for people with stomach ulcers or esophagitis, as it can exacerbate these conditions.
Summary
The first thing I want to close with is to try to avoid the trigger foods. Anything spicy will hurt you obviously. But other things like lemon and citrus could too. Mustard sometimes causes heartburn or reflux. Overeating does, but most people don’t even know that so control portions.
Something else I’ve noticed for me is that I can’t eat anything big before doing aerobics or yoga or it tends to want to come back up, lol! Maybe that’s just because I’m squeezing my innards so much doing various poses or dance moves. So I just eat after my exercise routine, that solves it.
Next up is to choose the correct acid reducer for you. I’m a natural-minded pharmacist so I always recommend starting with holistic options and dietary changes.I like the zinc carnosine and mastic gum and aloe vera gel supplements (which are drinkable).
I know that navigating the array of antacids available can be overwhelming, I ‘ve seen those pharmacy aisles! I used to walk customers like you down the aisles and talk about all this in order to help people choose the best option.
It’s hard, especially when considering both traditional and natural options and there are just so many. Understanding each option’s mechanism of action, benefits, and potential drawbacks is crucial for making an informed choice that’s why I wrote this blog.
Whether you opt for the quick relief offered by TUMs and Mylanta, the longer-term solutions like Pepcid AC and Nexium, or natural remedies such as mastic gum, zinc carnosine, or marshmallow root, it’s important to align your choice with your specific health needs and conditions.
Remember, while over-the-counter and natural remedies can provide relief, they are not substitutes for medical advice. For persistent or severe symptoms, consulting a gastroenterologist in your area to check for major issues, and rule things out. I do not recommend self-treatment for a long-term problem such as this. The guidelines I’ve provided are really for minor concerns, or those caused by eating 20-something tacos!

Suzy Cohen, has been a licensed pharmacist for over 30 years and believes the best approach to chronic illness is a combination of natural medicine and conventional. She founded her own dietary supplement company specializing in custom-formulas, some of which have patents. With a special focus on functional medicine, thyroid health and drug nutrient depletion, Suzy is the author of several related books including Thyroid Healthy, Drug Muggers, Diabetes Without Drugs, and a nationally syndicated column.
