What's On This Page?
ToggleWhen your mouth hurts, it’s so uncomfortable, it’s hard to enjoy a meal, and sometimes even sleep. Not only that, oral lesions can produce a lot of mental chatter… is it simple like a canker sore? Could it be an infection? Is it contagious? Get on “Dr. Google” lol, and in about 5 minutes you’ll be convinced you have oral cancer!!! What are the symptoms of that? Today, I’ll clarify all of this and more as we delve deeper into an immune-system disorder that sometimes affects the mouth and causes scary-looking sores that linger for weeks, if not months!
 It’s called “Oral Lichen Planus” (pronounced “Like-en PLAY-nus”) and it’s a chronic inflammatory condition affecting the mucous membranes in the mouth. This condition remains a challenge for many people because it doesn’t respond easily to things like mouthwashes or oral gels that numb the area.
It’s called “Oral Lichen Planus” (pronounced “Like-en PLAY-nus”) and it’s a chronic inflammatory condition affecting the mucous membranes in the mouth. This condition remains a challenge for many people because it doesn’t respond easily to things like mouthwashes or oral gels that numb the area.
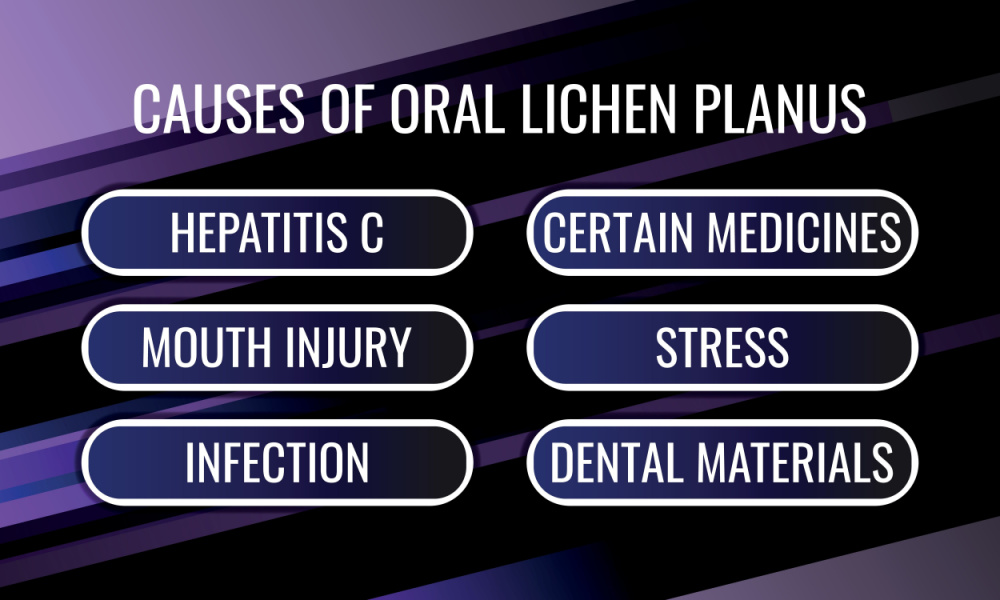
With approximately 1-2% of the global population experiencing this condition, its impact is pretty significant. The problem is characterized by painful lesions and discomfort, and risk factors include genetic predisposition and immune system dysfunction (usually it goes hand-in-hand with another autoimmune condition).
If you’re interested in another blog I wrote about immunity, you can CLICK HERE to read: How to Make Your Immune System Fight for You.
It’s also true that eating acidic foods can make it harder to heal. Doctors treat it with conventional things, let’s talk about those now.
Conventional Medical Treatments
The following medications are often used by people who have mouth sores. Those can include lichen planus, but also oral Candidiasis, angular cheilitis, oral leukoplakia, and oral hairy leukoplakia. Your physician will know which one of these is right for you.
Dexamethasone Elixir (0.5mg/5cc): This is a topical corticosteroid that helps with pain and inflammation. A potent corticosteroid, this prescription elixir reduces inflammation and provides symptomatic relief by putting the steroid right into the mouth. It’s used as a swish and spit treatment, without swallowing. This can be ordered by your doctor and picked up at pretty much any local pharmacy in your area. If you need some specific dose that isn’t available commercially at a local pharmacy, the compounding pharmacy can of course make it.
It is considered one of the most potent topical corticosteroids available. It is classified as a super-high-potency corticosteroid (Class I) and is typically used for severe dermatological conditions that are unresponsive to less potent steroids.
Clobetasol Propionate 0.05% oral rinse is something your physician can have compounded for you at a Compounding Pharmacy. It’s not found at the local pharmacy as a commercially prepared solution. This medication is similar to dexamethasone, but it is more potent and would be used if the dexamethasone doesn’t work well enough.
Clobetasol is also a corticosteroid medication just like dexamethasone. Yet another choice in this category of topical corticosteroids is fluocinonide, which has to be compounded as an oral solution (because it’s only commercially available as an ointment/cream). Again, these corticosteroid drugs help with pain and inflammation. Similarly to dexamethasone, these are for swish and spit, without swallowing.
Calcineurin Inhibitors: Tacrolimus and pimecrolimus, applied topically to the lesions, may help modulate the immune response in a local manner. These are a bit controversial, and definitely not first line agents. You might see these prescribed to a person who is unresponsive to the topical corticosteroids listed above (ie dexamethasone, clobetasol or fluocinonide, etc).
Systemic Treatments: In severe cases, systemic corticosteroids or immunosuppressants may be recommended. Things such as a steroid dose pack like Medrol or Prednisone pack include pills that you take by mouth, starting with a high dose, and then tapering it each day. These work well, however some people experience insomnia, psychiatric side effects and nausea so tolerability is something to consider.
Laser Therapy: Low-level laser therapy (LLLT) can help in reducing symptoms and promoting healing. This is usually something your dentist does for you. A PAPER is here for you to read. Essentially, LLLT is the use of red light on your gums or tongue, which helps to minimize pain, swelling and redness which of course allows the mouth sores to heal faster.
Miscellaneous Treatments: Other things that I won’t elaborate on here, include cyclosproine or retinoids. These would be administered in a topically applied gel form to the lesions. Also, there are treatments such as oral photochemotherapy and extracorporeal photochemotherapy that can be done. I am not a dentist so I don’t know much about those treatments so I’ll have to leave it there for you to research on your own and talk to your dentist or oral surgeon.
You may be interested in my other article: Your Tongue Tells a Story.
Natural Remedies for Oral Lichen Planus
 Aloe Vera Gel: Aloe vera is renowned for its healing and anti-inflammatory properties. For oral lichen planus, using pure aloe vera gel directly on the affected areas can provide relief. It’s recommended to apply the gel two to three times daily. Ensure the gel is as pure as possible, with minimal additives. After applying, avoid eating or drinking for at least 30 minutes to allow the gel to work effectively. You can cut into a piece of fresh aloe, or you can buy commercially prepared aloe vera gel.
Aloe Vera Gel: Aloe vera is renowned for its healing and anti-inflammatory properties. For oral lichen planus, using pure aloe vera gel directly on the affected areas can provide relief. It’s recommended to apply the gel two to three times daily. Ensure the gel is as pure as possible, with minimal additives. After applying, avoid eating or drinking for at least 30 minutes to allow the gel to work effectively. You can cut into a piece of fresh aloe, or you can buy commercially prepared aloe vera gel.
Turmeric: The curcumin in turmeric has strong anti-inflammatory and antioxidant properties. To use turmeric for oral lichen planus, create a paste by mixing turmeric powder with a little water. It’s literally that easy! Apply this paste to the lesions in the mouth once or twice daily. Alternatively, turmeric supplements can be taken orally for a more systemic approach to inflammation and immune dysfunction.
Vitamin A: Essential for maintaining healthy mucous membranes, Vitamin A can be beneficial in the healing process. Supplements can be taken, but it’s also beneficial to include Vitamin A-rich foods in the diet, such as carrots, sweet potatoes, and leafy greens.
Vitamin D: Since immune dysfunction is a key part of the etiology of oral lichen planus, it’s pretty safe to say that having adequate amounts of vitamin D in your body matter! But don’t take my word for it, look at this STUDY (a randomized controlled clinical trial) which proves that there is an association between low serum vitamin D and oral lichen planus. Low D impacts the progression and prognosis of oral lichen planus.
Catalase and Glutathione: There’s a STUDY that suggests low levels of both of those antioxidants are associated with oral lichen planus. Scientists concluded, “that the salivary levels of Glutathione reductase and Catalase were lower in OLP patients than in the healthy group, which means these antioxidants were affected by OLP and also associated with the type of it. So salivary Glutathione reductase and Catalase levels may be used as biomarkers for OLP monitoring and treatment.”
If you are looking for the very best supplement of CATALASE, use my brand because it is encapsulated in acid-resistant capsules so it is guaranteed to be absorbed, and work!
Tea Tree Oil: Known for its antiseptic and anti-inflammatory properties, tea tree oil can be used as a natural mouthwash. However, it should be diluted before use, as it’s quite potent. Mix a few drops of tea tree oil in a cup of warm water. Use this as a mouth rinse, swishing around the mouth for a minute before spitting it out. This can be done once or twice daily. Be sure not to swallow the rinse, as tea tree oil should not be ingested.
Chamomile Tea: Chamomile has soothing and anti-inflammatory properties, making it an excellent natural remedy for oral lichen planus. To use chamomile tea as a mouth rinse, steep a chamomile tea bag in hot water for a few minutes, then allow it to cool down to a comfortable temperature.
Use the tea to gently rinse the mouth for a minute or so, then spit it out. This can be done two to three times daily. While chamomile tea is generally safe to swallow, the focus here is on swishing it around the mouth for its topical benefits.
My “Immune Script” which supports immune health and cytokines and while this is not a direct treatment for any disease (including lichen planus), it supports a healthy immune system and provides the right nutrients and prebiotics for cytokine balance.* Another consideration in terms of immune support is Vitamin D.
Mouthwashes for Oral Lichen Planus
When dealing with oral lichen planus, choosing the right mouthwash, toothpaste, and topical treatments is crucial, as certain ingredients can irritate the sensitive mucosa affected by this condition. Here are some guidelines:
Alcohol-Free Mouthwashes: Alcohol can be irritating to the lesions caused by Lichen Planus. Look for mouthwashes that are alcohol-free and formulated for sensitive mouths. Products containing aloe vera or chamomile can be soothing.
Saline Rinses: A simple saline solution (salt water) can be effective and gentle. Mix a teaspoon of salt in a cup of warm water and use it as a mouth rinse. This can help in maintaining oral hygiene without irritation. As for the salt you use, that’s up to you.
There are pros and cons to all salts. For example, plain iodized salt (NaCl) is cheap and readily available but it’s stripped of the other healing minerals that natural sea salt has. For that reason, I suggest you use something like Real® salt, Himalayan sea salt or Celtic salt if you happen to have something like that.
Chlorhexidine Mouthwashes: These are often recommended for their antimicrobial properties. However, they should be used cautiously and for short durations, as they can cause staining of the teeth and alter taste sensation.
Homemade Mouth Rinse Recipe
A homemade mouth rinse is something you can do at home. It can be made very easily by combining chamomile tea with a few drops of essential oil of tea tree. Swish in the mouth for a minute and spit out. This rinse can help in reducing discomfort and promoting oral health. It is a swish and spit, without swallowing.
Toothpastes
SLS-Free Toothpastes: Sodium Lauryl Sulfate (SLS), a common ingredient in toothpastes, can irritate oral lichen planus. Opt for SLS-free toothpastes, which are gentler on the mouth.
Toothpastes for Sensitive Teeth: These types of toothpastes are often formulated to be less irritating and may be a good choice for those with oral lichen planus.
Natural or Herbal Toothpastes: Toothpastes containing natural anti-inflammatory ingredients like aloe vera or tea tree oil might be beneficial.
Topical Treatments Like Orajel
Orajel: Products like Orajel, which contain benzocaine, are designed to numb the area and can provide temporary relief from the pain of oral lesions. However, they should be used sparingly and only when necessary, as overuse can lead to further irritation or allergic reactions in some individuals.
General Recommendations
- Avoid Irritants: It’s important to avoid products containing harsh chemicals, strong flavors, or alcohol, as these can exacerbate symptoms.
- Patch Testing: Before committing to a new product, consider doing a patch test to ensure it doesn’t irritate your mouth.
Remember, while these products can help manage symptoms, they are not cures for lichen planus. Ongoing management and regular consultations with healthcare professionals are essential for effective treatment and symptom relief.
Foods to Avoid During a Flare-Up of Oral Lichen Planus
When experiencing a flare-up of oral lichen planus, certain foods can exacerbate symptoms. It’s generally recommended to avoid:
- Acidic Foods: Citrus fruits, tomatoes, and foods high in vinegar can irritate sensitive oral tissues.
- Spicy Foods: Hot spices can cause discomfort and irritation.
- Hard or Crunchy Foods: These can cause mechanical irritation or injury to the lesions.
- Alcoholic Beverages: Alcohol can be drying and irritating to oral lesions.
- Very Hot Foods and Beverages: Extreme temperatures can cause discomfort. Opt for bland, soft foods that are less likely to irritate the mouth. Keeping a food diary can also help identify specific triggers.
Visual Differences Between Oral Lichen Planus and Oral Cancer
 Oral lichen planus and oral cancer can look different.
Oral lichen planus and oral cancer can look different.
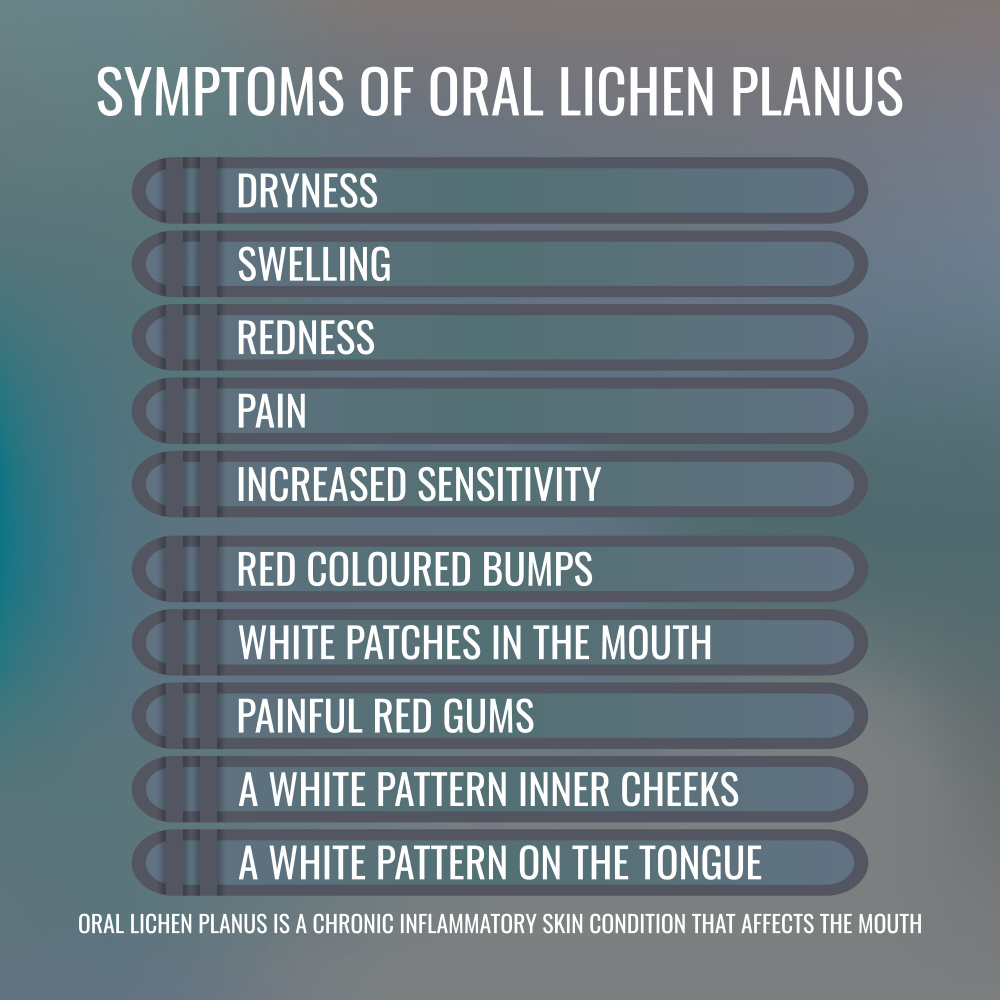
Oral Lichen Planus: Typically presents as white, lacy patterns (Wickham’s striae) on the mucous membranes. The lesions may have a slightly raised, red border but are usually not ulcerated unless they are erosive. The borders are often well-defined.
Oral Cancer: Lesions may appear as a persistent ulcer or a red and white patch that doesn’t heal. They may have irregular, ill-defined borders and might bleed easily. The color can vary from red, white, or a combination. Oral cancer lesions are often harder and can be felt as a lump or thickening in the mouth.
It’s crucial to consult a healthcare practitioner (or even two!) for a proper diagnosis, as visual inspection alone is not reliable for distinguishing between these conditions. You may need a biopsy to know for sure what’s going on. Regular dental check-ups and screenings are essential, especially for those with chronic conditions like lichen planus, which can have a higher risk of developing into more serious conditions like oral cancer.
When to Follow Up
It’s important to regularly monitor the condition of oral lesions and see your dentist and/or oral surgeon if you notice any of this:
- Increase in Size or Number: Any noticeable growth in the size or an increase in the number of lesions.
- Change in Color: If lesions become markedly red, white, or develop a distinct color change.
- Bleeding or Ulceration: If the lesions begin to bleed easily or develop into ulcers.
- Pain or Discomfort: An increase in pain or discomfort, particularly if it’s not relieved by usual treatments.
- Difficulty Eating or Swallowing: If the condition starts affecting your ability to eat or swallow.
These changes might not indicate something as serious as oral cancer, but they warrant medical attention to rule out complications or the need for treatment adjustment.
Conclusion
Oral Lichen Planus is a chronic inflammatory condition that affects the mucous membranes of the mouth, causing discomfort and impacting quality of life. During flare-ups, it’s advisable to avoid acidic, spicy, hard, or crunchy foods, as well as alcoholic beverages to reduce irritation.
In terms of treatment, alcohol-free mouthwashes, saline rinses, and SLS-free toothpastes are recommended. Natural remedies such as aloe vera gel, turmeric paste, Vitamin A supplements, diluted tea tree oil mouth rinses, and chamomile tea can provide relief. However, it’s important to consult healthcare professionals before starting any new treatment.
Regular monitoring of oral lesions is crucial. Follow up with a healthcare professional if there is an increase in size or number of lesions, changes in color, bleeding, increased pain, or difficulty eating or swallowing. These symptoms could indicate the need for a revised treatment plan or the presence of more serious conditions.
Visually, oral lichen planus typically presents as white, lacy patterns with well-defined borders, while oral cancer lesions might appear as persistent ulcers or patches with irregular borders and varied colors. I wouldn’t say they’re nothing to worry about because they are, you want to improve immunity and take care of yourself, but relax into the knowing that this condition is not cancer of the mouth! Regular check-ups are essential for proper diagnosis and management and again, you want to take care of it so it does not progress to anything more serious.

Suzy Cohen, has been a licensed pharmacist for over 30 years and believes the best approach to chronic illness is a combination of natural medicine and conventional. She founded her own dietary supplement company specializing in custom-formulas, some of which have patents. With a special focus on functional medicine, thyroid health and drug nutrient depletion, Suzy is the author of several related books including Thyroid Healthy, Drug Muggers, Diabetes Without Drugs, and a nationally syndicated column.
