What's On This Page?
ToggleHormone replacement therapy (HRT) is a powerful tool in managing symptoms associated with hormonal imbalances and age-related declines. It’s not just about alleviating hot flashes or improving mood – it’s about supporting long-term health in areas such as bone density, cardiovascular function, and even cognitive health. But who qualifies for hormone therapy? How do you monitor yourself during treatment, and how do you avoid potential risks, including hormone-driven cancers? What about puberty blockers, they’ve been prescribed to minors in this country fairly indiscriminately and without long-term studies. Let’s dive into all of these crucial topics with a focus on bioidentical hormones and their role in optimizing health and helping you with HRT (hormone replacement therapy).
Who Qualifies for Hormone Therapy?
Hormone therapy is not a one-size-fits-all solution. It’s typically indicated for individuals experiencing symptomatic hormone deficiencies, such as those in menopause, andropause, or with conditions like adrenal insufficiency or hypogonadism. Common symptoms prompting evaluation include:
- HOT FLASHES and night sweats
- Vaginal dryness or discomfort
- Decreased libido
- Fatigue and mood changes
- Poor sleep
- Cognitive changes, such as brain fog
- Bone loss or increased risk of osteoporosis
- People with Seasonal Affective Disorder (READ MY ARTICLE HERE)
For men, low testosterone levels can manifest as fatigue, reduced muscle mass, low libido, and even depression. Hormone therapy can also be considered for those recovering from surgeries, like oophorectomy (removal of ovaries) or prostate procedures, where hormone levels have been affected.
That said, therapy should be personalized. A thorough medical history, lab testing, and symptom evaluation are vital to determine whether you’re a candidate for HRT. If you are not sure if you’re a candidate for HRT, how would you know which testing option to use in order to find out? Let’s talk about that next.
Educate Yourself on Bioidentical and Synthetic Hormones
Knowledge is power. Learn how each option works, their risks, and their benefits so you can make an informed decision. A crucial part of this process involves understanding the best way to assess your hormone levels and metabolism.
Testing Methods: Urine, Blood, and When to Use Each
- Urine Testing (ie The DUTCH Complete Test)
- The DUTCH Complete test is one of the most comprehensive ways to evaluate hormones, providing insights into levels of estrogen, progesterone, testosterone, DHEA, and cortisol, as well as how these hormones are metabolized.
- Best for: Those who are already on hormone therapy (ie topical creams, patches) because it reflects how the body processes and eliminates hormones. Urine testing also excels at assessing hormone metabolites, which reveal potential risks like estrogen dominance or cancer-driving pathways.
- Limitations: It may not accurately reflect hormone levels in people who take oral hormone medications, as oral administration alters how hormones are metabolized and excreted. Additionally, for individuals NOT on therapy, blood testing will be more straightforward to establish your baseline levels.
- Blood Testing (Serum Levels)
- Blood tests measure circulating levels of hormones, such as estradiol, progesterone, testosterone, and cortisol. These tests provide a snapshot of what’s in your bloodstream at the time of the draw.
- Best for: Establishing baseline hormone levels before starting therapy, particularly for individuals not yet on any hormone replacement. It’s also the preferred method for monitoring oral hormone treatments, as oral administration affects metabolism in ways that urine tests may not capture.
- Limitations: Blood tests don’t measure hormone metabolites or provide insights into how your body processes hormones. They also can’t reflect the diurnal (daily) variations in hormones like cortisol as effectively as urine or saliva testing.
- Saliva Testing
- Saliva testing measures free, bioavailable hormone levels and is sometimes used for cortisol evaluation or sex hormone levels.
- Best for: Evaluating bioavailable hormone levels when topical hormone therapy is used, though urine testing often provides more detailed data. Saliva testing may not capture the full picture of metabolism or bound hormone levels.
Synthetic vs. Bioidentical Hormones: Key Considerations
- Bioidentical Hormones:
- These are structurally identical to your body’s hormones, allowing for better receptor compatibility and more natural metabolic pathways. They’re commonly prescribed as creams, gels, patches, or pellets, they offer flexibility in dosing and delivery.
- Benefits include reduced risks of side effects like clotting or hormone-driven cancers when compared to synthetic options.
- Synthetic Hormones:
- Synthetic hormones often differ structurally from your body’s natural hormones. Examples include synthetic progestins or conjugated equine estrogens.
- They may produce less favorable metabolites, which can increase risks of side effects, such as cardiovascular events or hormone-driven cancers. There is more to read about this HERE.
Choosing the Right Test for You
- If you are not on therapy, blood testing is often the best starting point to establish baseline hormone levels.
- If you are on topical or transdermal therapy, urine testing (like the DUTCH Complete test) provides critical insights into how well your body absorbs and metabolizes hormones.
- If you take oral hormone therapy, blood tests would likely be more reliable since oral medications can significantly alter urinary hormone metabolites.
List of Synthetic Medications for HRT
Estrogen-Only Medications
- Premarin (Conjugated Estrogens)
- Estratab, Menest (Esterified Estrogens)
- Estrace, Gynodiol (Estradiol)
Combined Estrogen and Progestin Medications
- Prempro, Premphase (Conjugated Estrogens and Medroxyprogesterone Acetate)
- Activella, Combipatch (Estradiol and Norethindrone Acetate)
- Climara Pro (Estradiol and Levonorgestrel)
Progestin-Only Medications
- Provera (Medroxyprogesterone Acetate)
- Aygestin (Norethindrone Acetate)
Selective Estrogen Receptor Modulators (SERMs)
- Duavee (Conjugated Estrogens and Bazedoxifene)
Surprise! Progesterone is NOT the Same as Progestin
Many people who do hormone specialty work do not realize the immense differences between natural progesterone and progestins. This is a critical point I want to make because it can impact your risks for illness and cancer. Progesterone is the natural hormone your body produces, essential for regulating menstrual cycles, supporting pregnancy, and maintaining hormonal balance. You can get this in a bioidentical form easily it’s a pill that usually comes as 100mg. I personally suggest this drug be taken orally at nighttime.
Progestins, on the other hand, are synthetic versions of the hormone designed to mimic progesterone but they have slightly altered structures that can trigger different, sometimes unwanted and uncomfortable effects. Most women do not know this important fact. Many hormone specialists practicing in the field are also unaware of this major distinction and prescribe synthetic progestin drugs (like medroxyprogesterone) rather than natural progesterone. A commercial “natural” progesterone is called Prometrium® which is suspended in peanut oil. I tried this once and almost fainted so I’m not a fan, but many women take it. I prefer the compounded progesterone for natural.
Some women cannot tolerate synthetic progestin drugs like myself, and they have no idea that natural progesterone would probably work better for them. That’s why I wrote this article. While compounded progesterone (especially in its bioidentical form) is gentler and more aligned with your body’s natural processes, progestins are often used in birth control and some hormone therapies like HRT for their potency and extended action. Medroxyprogesterone (Provera®) is the most popular synthetic progestin. Others that are sometimes found at the pharmacy and prescribed include norethindrone or levonorgestrel.
Choosing the natural form for HRT is what I have always recommended, unfortunately most of you reading this today are probably on the synthetic drug form (categorically called a progestin drug). I always advocate for solutions that align closely with your body’s natural rhythms.
What Are the Recognized Harms and Risks of Therapy?
The recognized harms and risks associated with synthetic hormones for HRT vary depending on the type of medicine, the dose and duration of treatment, and other individual factors such as your age, health status, and medical history. Here is a summary of potential risks and harms associated with different types of HRT:
General Risks of HRT:
- Cardiovascular Risks:
- Increased risk of blood clots (deep vein thrombosis, pulmonary embolism), particularly with oral estrogen formulations.
- Potential increased risk of stroke and heart disease, especially in older women or those starting HRT long after menopause.
- Cancer Risks:
- Breast Cancer: Combined estrogen-progestin therapy is associated with a slightly increased risk of breast cancer, especially with long-term use.
- Endometrial Cancer: Estrogen-only therapy can increase the risk of endometrial (uterine) cancer in women with an intact uterus unless combined with a natural progesterone.
- Ovarian Cancer: Some studies suggest a small increased risk of ovarian cancer with prolonged HRT use.
- Gallbladder Disease:
- Estrogen therapy, particularly oral forms, can increase the risk of gallstones and gallbladder disease.
- Cognitive Decline:
- This is often news to people but starting HRT late in life (like after 65 years of age) can potentially increase your risk of dementia or cognitive decline.
Specific Risks by Hormone Type
Estrogen-Only Therapy:
- Risks:
- Increased risk of stroke and blood clots.
- Endometrial hyperplasia and cancer (if no progesterone is added in women with a uterus).
Combined Estrogen-Progestin Therapy:
- Risks:
- Greater risk of breast cancer compared to estrogen-only therapy.
- Potential increase in cardiovascular risks.
Progestin-Only Therapy (the risk noted below does not apply to progesterone which is natural)
- Risks:
- May cause mood changes, bloating, or breast tenderness.
- Long-term use is linked to a slight increase in breast cancer risk.
Selective Estrogen Receptor Modulators (SERMs):
- Risks:
- Risk of blood clots and stroke.
- May cause hot flashes and leg cramps.
Other Considerations:
- Side Effects:
- Common side effects include nausea, bloating, headache, mood swings, and breast tenderness.
- Timing of Therapy:
- Risks may differ depending on when HRT is started. For example, starting HRT closer to menopause onset may carry fewer risks compared to starting it later.
- Individual Variations:
- The risks vary widely based on individual factors like smoking, obesity, and family history of cardiovascular disease or cancer.
Important Notes:
- The Women’s Health Initiative (WHI) study in 2002 raised awareness of these risks, leading to more cautious prescribing of HRT.
- Transdermal or vaginal forms of HRT may carry fewer risks (e.g., lower clotting risk) compared to oral forms.
- The decision to use HRT should involve a thorough evaluation of benefits and risks, individualized for each woman.
If you are considering or currently using HRT, it’s essential to discuss these risks with your healthcare provider to ensure it aligns with your health needs and goals.
Monitoring and Testing During Hormone Therapy
Monitoring hormone therapy is as critical as starting it. Hormones are powerful substances, and their levels must be maintained within an optimal range. Over-treatment or under-treatment can lead to adverse effects.
The DUTCH Complete test (Dried Urine Test for Comprehensive Hormones) is one of the most comprehensive ways to monitor hormone levels at home, offering insights into cortisol, cortisone, DHEA, progesterone, testosterone, estrone, estradiol, and estriol. This test also analyzes urine metabolites, helping you understand how your body processes and eliminates hormones. For example, imbalances in estrogen metabolism pathways could increase the risk of hormone-sensitive cancers, like breast or prostate cancer. Some of you may be interested in my other article, What You Should Test for in Prostate Cancer.
When monitoring HRT, the following parameters are essential:
- Baseline Testing: Establish your hormone levels before initiating therapy.
- Follow-Up Testing: Monitor levels every 3–6 months initially, then annually, to ensure proper dosing.
- Symptom Tracking: Keep a journal of your symptoms—this subjective data often complements lab results.
- Metabolite Analysis: Urinary metabolites reveal whether your body is metabolizing hormones safely or producing potentially harmful byproducts.
Symptoms of Over- and Under-Treatment
Hormone therapy, when poorly managed, can lead to a range of symptoms. Being vigilant about these is key to avoiding complications.
Over-Treatment
Symptoms of excessive hormone levels include:
- Estrogen: Breast tenderness, bloating, headaches, and increased risk of estrogen-sensitive cancers.
- Testosterone: Aggression, acne, hair loss, or increased red blood cell count.
- Progesterone: Sedation, dizziness, or fatigue. Here is a good article by the Cleveland Clinic about PROGESTERONE.
Under-Treatment
If hormone levels remain suboptimal, symptoms like fatigue, mood swings, hot flashes, or low libido may persist.
The Cancer Connection: Estrogen and Risks
One of the most significant concerns with hormone therapy is the potential link to cancer. Estrogen dominance—whether due to endogenous factors or poorly managed HRT—can increase the risk of breast, ovarian, and uterine cancers. Here’s why monitoring is essential:
- Estrogen Metabolites: Some estrogen metabolites, particularly 16-alpha-hydroxyestrone, are associated with proliferative (tumor-promoting) effects. The DUTCH Complete test measures these metabolites, allowing for targeted interventions to shift metabolism toward safer pathways.
- Progesterone Balance: Progesterone opposes estrogen’s proliferative effects. Bioidentical progesterone, unlike synthetic progestins, supports this balance without introducing additional risks.
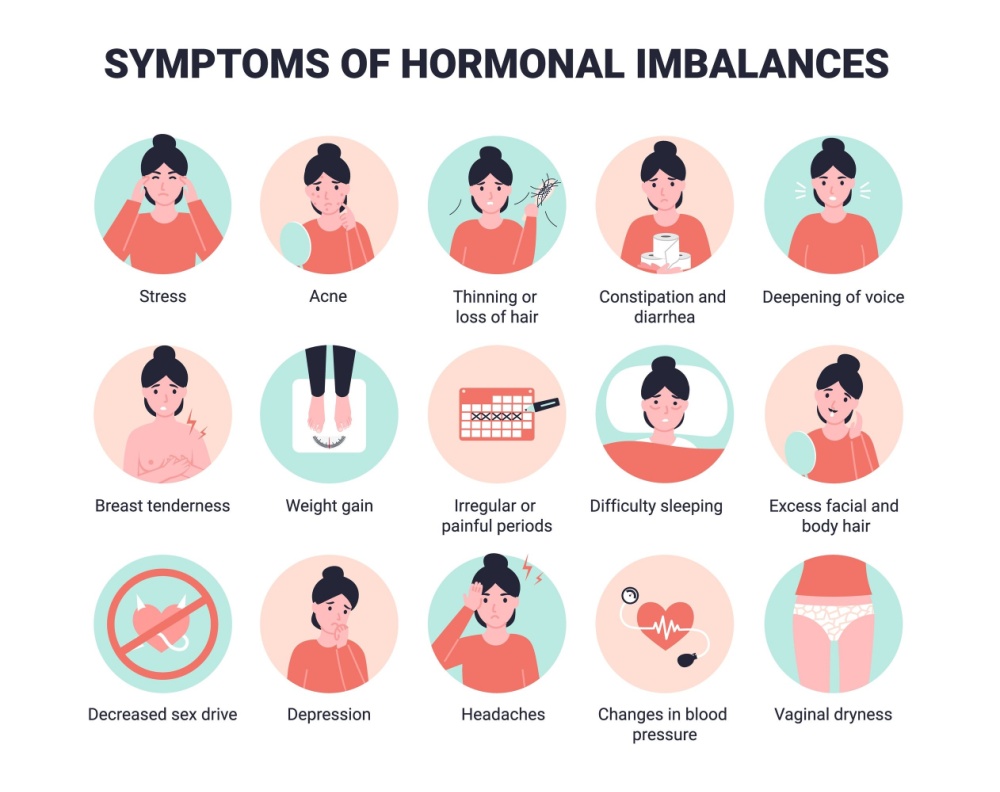
For men, the interplay between testosterone and estrogen is crucial in prostate health. Excess conversion of testosterone to estradiol (via aromatase enzyme) can exacerbate prostate issues, making monitoring testosterone-to-estrogen ratios essential. Below is a graphic I downloaded to illustrate the symptoms of hormonal imbalances specific to women’s health. One thing is that this graphic fails to list fibroids, but this is a sign of hormonal imbalance and you can read more in my article, 8 Natural Strategies for Uterine Fibroids.
What About Puberty Blockers
I’ve been asked about this over the years and while it doesn’t have much to do with hormones or HRT, the topic still fits. To be clear, bioidentical hormones are not typically used in conjunction with puberty blockers like leuprolide acetate (Lupron) or histrelin acetate (Supprelin LA). However, they may be used for other gender dysphoria issues, or to balance hormones later. By the way Lupron is usually used for endometriosis, prostate cancer or uterine fibroids.
Puberty blockers like those listed above or others are given to children as young as 12 pose significant and dangerous risks with potentially irreversible consequences. They cause hormonal imbalances because they do not coincide with natural X and Y chromosomes. The drugs employed interfere with critical developmental processes, including bone density formation, sexual maturation, and brain development, potentially leading to lifelong physical and emotional harm.
They can cause permanent infertility, impair cognitive and emotional growth, and exacerbate mental health issues like anxiety or depression. They can impact one’s ability to achieve orgasm in many cases although this is not usually talked about openly, and it is contingent on the hormones given and the age of the child. Socially, these drugs isolate children by preventing them from developing alongside their peers.
Far from a “pause button,” these blockers often lock children into a pathway of lifelong medical intervention and prescriptions, increasing the likelihood of persisting gender dysphoria rather than allowing natural resolution. The long-term effects remain unknown, with potential risks for hormone-driven cancers, not to mention the ethical concerns of subjecting young, vulnerable children to such drastic interventions. The changes are profound. These drugs are not a benign solution in my humble opinion, they are a dangerous gamble with a young child (or teenager’s) future.
As you may already know, opinions on puberty blockers are deeply divided—some criticize opposition as “intolerant,” while others liken their use to severe ethical violations, with stronger language often reserved for surgical interventions. The world’s approach, meanwhile, is like a spice rack, with each country adding its own flavor:
Cautious Europe: Countries like Sweden, Finland, and the UK are tapping the brakes on routine use, favoring research trials or prioritizing psychological support first. They’re waiting for more solid evidence before moving ahead at top speed with prescribing.
Patchwork USA: In the U.S., it’s a mixed bag. Some states (22 states as of today Jan 14, 2025) have banned puberty blockers for minors, while others still allow access, creating a patchwork of policies.
Still on the Menu: Canada, Australia, the Netherlands, Spain, and New Zealand haven’t slammed the door on puberty blockers, but they’re taking a more cautious approach, focusing on informed consent and psychological evaluations.
Ongoing Review: Globally, there’s a collective “let’s pause and rethink” vibe as countries seek more clarity on the long-term effects and outcomes.
It’s a complex issue, balancing compassion, science, and safety, but thoughtful deliberation signals progress toward informed care and parental consent.
READ THIS: Bioidentical vs. Synthetic Hormones – The Main Difference
Bioidentical hormones are chemically identical to those your body naturally produces. This likeness allows them to fit perfectly into your body’s hormone receptors, minimizing side effects and maximizing effectiveness. Synthetic hormones, on the other hand, often differ structurally and may carry higher risks, particularly concerning clotting, cardiovascular events, and hormone-driven cancers.
For example, prescription estradiol patches contain estradiol but may also include chemical additives. Estradiol creams, often compounded by specialized pharmacies, provide flexibility in dosing and often lack these additives. While both forms deliver estradiol, creams may offer more customization, especially when tailored to individual needs. Natural progesterone is safer than synthetic because it’s bioidentical, not a mimic that barely forces its way into your cell by hacking your receptors.
Urine Metabolites: The Value of DUTCH Testing
Why is metabolite analysis so important? Because it provides a detailed map of how your body processes hormones. Estrogen, for instance, can follow three primary metabolic pathways: 2-hydroxyestrone (protective), 4-hydroxyestrone (potentially harmful), and 16-alpha-hydroxyestrone (tumor-promoting).
The DUTCH Complete test highlights these pathways, allowing you to:
- Identify risks of estrogen dominance or poor metabolism.
- Take actionable steps, such as incorporating dietary changes (e.g., increasing cruciferous vegetables) or supplements (ie DIM or calcium D-glucarate) to promote safer estrogen metabolism.
If you’re interested in more information, consider taking a couple of minutes to skim through this article, The DUTCH Complete Test – #1 Guide to Hormone Testing.
Hormones Beyond Estrogen: The Role of Cortisol, DHEA, and Progesterone
Your adrenal hormones—cortisol and DHEA—are key players in overall hormonal health. Chronic stress can disrupt this balance, leading to symptoms like fatigue, poor sleep, and weight gain. Monitoring cortisol (active) and cortisone (inactive) can help identify adrenal dysfunction, whether it’s high cortisol from stress or low cortisol linked to burnout.
Progesterone, often called the “calming hormone,” is another critical piece of the puzzle. It not only balances estrogen but also supports sleep, mood, and bone health.
Prostate and Breast Health: Hormone Therapy’s Role
Hormones play a dual role in prostate and breast health—they can be protective or harmful, depending on how they are balanced and metabolized.
- Prostate Health: Testosterone therapy, when appropriately managed, can improve symptoms of low libido and fatigue in men. However, excess testosterone can convert to estradiol, potentially contributing to prostate enlargement or even cancer in predisposed individuals.
- Breast Health: For women, maintaining a healthy balance of estrogen and progesterone is essential to prevent estrogen dominance and its associated risks. The DUTCH test’s metabolite analysis provides invaluable insights here because it shows the 4-OH to 16-OH and other metabolites.
3-Step Action Plan
Here’s a 3-step action plan tailored for both men and women to help you determine whether synthetic or bioidentical hormones are the better option for your needs. Before choosing between synthetic and bioidentical hormones, it’s essential to understand your current hormonal status and health goals. Here’s how:
- Identify Symptoms: Track your symptoms over time. Common signs of hormone imbalances include fatigue, weight changes, hot flashes, low libido, poor sleep, mood swings, or brain fog. Read: 8 Ways to Save Your Brain and Calm Down.
- Get Tested: Use a reliable testing method to determine your hormone levels. See the beginning of this article to determine what kind of testing you need in order to evaluate key hormones like estrogen, progesterone, testosterone, DHEA, and cortisol, and/or their metabolites. For men, it’s especially important to assess testosterone and estradiol balance.
- Clarify Goals: Are you seeking relief from menopause or andropause symptoms, or are you aiming to support long-term health, such as bone density or cardiovascular function? Your goals and your doctor will guide your choice because some doctors will tell you not to worry, and just take what the drug makers sell as opposed to going to a compounding pharmacy. This may be due to them not fully knowing how to prescribe bioidenticals.
Conclusion: Why Choose Bioidenticals?
I am always in favor of bio-identical hormones so long as they are used in proper doses and you don’t have any adverse side effects (which occur at improper doses). Bioidenticals offer a safer and more tailored approach to HRT, emphasizing balance and individualized care. If you’re doctor doesn’t know about those, switch to a hormone specialist that works with patients all day long.
If you’re considering hormone therapy, the DUTCH Complete test is on sale at MY OTHER WEBSITE since I am a Provider and can sell it online directly to you. It’s an at-home test – no doctor’s visit required – that provides comprehensive insights into your hormonal health. Plus, you’ll receive a free eBook to help you interpret your results and take control of your health journey. Once you have your test results you can visit a hormone specialist who can help you feel better quickly because they can see what’s going on and prescribe the correct hormones for you. This will breathe life into you, and turn back the clock. Skin improves, hair growth and energy… and much more.
Empower yourself with the knowledge and tools to make informed decisions about hormone therapy. Hormones may be small molecules, but their impact on your health is profound. With the right approach, you can harness their power for vibrant, lasting health, protect your heart and reduce your risk for cancer.

Suzy Cohen, has been a licensed pharmacist for over 30 years and believes the best approach to chronic illness is a combination of natural medicine and conventional. She founded her own dietary supplement company specializing in custom-formulas, some of which have patents. With a special focus on functional medicine, thyroid health and drug nutrient depletion, Suzy is the author of several related books including Thyroid Healthy, Drug Muggers, Diabetes Without Drugs, and a nationally syndicated column.