What's On This Page?
ToggleThis article is going to tell you more about how to help irritated and itchy eyes. It will also help determine if blepharitis is what you’re dealing with, or if’s ocular rosacea… if it’s something else. Let’s find out what’s behind your irritated eyes. Let me ask you a question:
If your eyes feel dry, gritty, itchy, or irritated, but every exam keeps coming back “normal,” have you ever been told to look at your eyelids instead of your eyes?
Most people haven’t. I didn’t fully appreciate this either until I started researching the topic and seeing how often blepharitis flies under the radar.
Blepharitis is one of those conditions that doesn’t announce itself loudly. It more like whispers. And if you don’t know what to listen for, you’ll keep treating the wrong thing and you know how much I hate a misdiagnosis. Those happen ALL the time to people!
What blepharitis really is (in plain English)
Blepharitis simply means inflammation of the eyelids, especially along the lash line. That’s it. Not an infection. Not contagious. Not dangerous. But definitely annoying and uncomfortable.
In many people, it’s tied to oil glands along the eyelids that aren’t working well. These meibomian glands are supposed to release a micro amount of oil that slows your tear evaporation. When the oil gets thick, stagnant, or inflamed, your tear film becomes unstable. The eye surface dries out, even if your eyes water constantly. It’s ironic, isn’t it?
That’s one of the biggest clues.
Watery eyes can still be dry eyes.
Read my related article for more help: 5 Awesome Solutions for Dry Eyes and Blurry Vision
Blepharitis Symptoms: How It’s Described
Most people don’t walk around saying or even thinking, “I think I have blepharitis.”
They say things like this:
- “My eyes feel gritty, like there’s sand in them.”
- “My vision gets blurry late in the day, then clears when I blink.”
- “My eyes itch, but allergy drops don’t really fix it.”
- “Sometimes I get a stye or these weird bumps on my eyelid.”
- “By afternoon, my eyes just feel so tired … and burny.”
If that sounds familiar, you’re not alone. Blepharitis symptoms often fluctuate, which makes people doubt themselves. One day your eye feels okay. The next day doesn’t. It comes off like you have an allergy. Maybe you try changing laundry detergents and bed sheets, or you try to use your device less (to reduce eye fatigue), or you try allergy eye drops, or whatever… it’s that variability that is a hallmark feature of blepharitis.
Here’s Why Blepharitis is Easy to Miss
Here’s the problem at the doctor’s office. Many eye exams focus on the inside of your eye, the important things like the retina, optic nerve, and basic structures. The exam focuses a lot on figuring out what your eye pressure is to see if you have glaucoma. All important. But blepharitis lives on the edges and it’s not always obvious.
If no one looks closely at the lash line or oil glands, it could be missed entirely. And because it’s so common, and severity varies, it’s sometimes dismissed and you’re diagnosed with “dry eye.” You’ll be told to get some wetting “tear” eye drops at the local pharmacy, and sadly, those don’t do a good job at relieving blepharitis.
I wrote this related blog that may interest you, 7 Key Strategies to Combat Blurry Vision: A Comprehensive Guide.
3 Main Reasons Blepharitis is Missed!
-
Symptoms overlap with “dry eye.” Grittiness, burning, and irritation are often labeled as dry eye without closely examining the eyelid margins where the problem usually resides.
-
The lids aren’t examined carefully. A quick eye exam may miss subtle signs like lash debris, mild redness at the lid margin, or early gland blockage unless the lids are specifically inspected.
-
It waxes and wanes. Blepharitis flares and calms down, so patients may look relatively normal on the day of the visit, leading to under-recognition or dismissal of symptoms.

Are There Risk Factors? Yes, and Medications Matter
Blepharitis isn’t random. Certain things make it more likely in a person, and this is where my pharmacist brain kicks in.
If you spend a lot of time on phones/devices, kindles, laptops, TV screens, or other screens your risk goes up. If you blink less than you should, your risk goes up. Also, this one’s underrated, but if live in a dry climate (think Utah, New Mexico, Wyoming, Colorado, or Arizona), wear contacts, or have fragile/sensitive skin, your risk goes up.
Another risk factor includes having dandruff, dry/flaky skin or dermatitis. And finally, if you have rosacea, or hormonal changes, you’re at a higher risk too. Take a look at this blog I wrote for a discussion on dry eyes, vitamins/herbs and how what you eat impacts your eyesight: Eye Drops and 8 Natural Treatments for Blurry Vision.
And yes, medications can absolutely make it worse.
I don’t say this to scare you, but to empower you. Many common drugs dry out the tear film or alter oil production. The most likely offenders are anticholinergics. I’ll make list of the biggest offending medications so you can check your drug list and see if you take one of these:
- Antihistamines – Here’s a blog listing: The 5 Best Natural Antihistamines
- Decongestants
- Antidepressants – Read: Why Some Antidepressants Work and Some Don’t
- Blood pressure medications – if you take these you MUST READ THIS to know what nutrients to restore (to reduce side effects)
- Isotretinoin (Accutane)
- Any anticholinergic medicine not listed here (search at drugmuggers.com) – Also, read this important article about stomach problems and gastroparesis (when you feel full quickly): Top 5 Medications Linked to Gastroparesis and How to Spot the Symptoms
Taking these medications may be necessary, so don’t suddenly stop (especially antidepressants because those get tapered not suddenly discontinued). And by the way, taking any of this doesn’t mean you caused the problem. It means your eyes are paying the price for medication side effects, and it can be easily mitigated. You can read more about blepharitis at the American Academy of Ophthmalogy’s WEBSITE.
What You Can Do now (Before Your Appointment)
When the eyes are uncomfortable and in this type of trouble, you need doctor’s appointment to see what’s going on. Try to resist self-diagnosis with your eyes. So make your appointment, and I’ll assume you did that. Now let’s talk about what you can before you go in to see doc.
If your goal is calm, stable eyes, that’s good. Not perfection, not even a cure yet. Just get those upset eyes to feel more calm and cooler.
You don’t need to wait passively (and be terribly uncomfortable) for your doctor’s appointment. Gentle, consistent care can make a real difference. Here’s the short list I give people while they’re waiting:
-
- Daily warm compresses (moist heat, 10 minutes). This helps melt thickened oils so they can flow again. You can buy a warm eye compress for this very purpose on Amazon, look for “MediViz Warm Compress Eye Mask.”
- Gentle lid hygiene once a day. Not scrubbing. Not baby shampoo. Just calm, consistent cleaning of the lash line. Hypochlorous acid (HOCl) lid sprays or wipes (non-stinging, anti-inflammatory). Try “OcuSOFT Lid Scrub Original” – these wipes are convenient and it sells for less than $20 on Amazon. Alternatively, try Avenova Eyelid and eyelash Cleanser Spray” also sold on Amazon. You can use a Q-tip to apply that one, or spray it on a cotton pad or whatever you think is right for you. You don’t spray it into the eye.
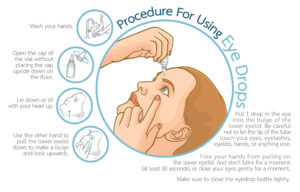
- Preservative-free artificial tears, used strategically – not every 20 minutes, but before irritation spirals. You’re looking for lipid-containing, preservative-free drops and these aren’t for when your eyes are screaming at you, it’s more like using them before irritation sets in.
- Blink retraining (shockingly effective): This sounds silly until it works. Most people don’t blink fully, especially while reading on a phone or screen. Try closing your eyes gently for 5 seconds every 10 – 20 minutes. Then squeeze softly for 2-3 seconds. Repeat 3 times. This alone can reduce end-of-day blur and light sensitivity. Do it right now.
- Black currant seed oil (a smart option for eyelid health).
Black currant oil supplies GLA (gamma-linolenic acid), a fatty acid that helps calm inflammatory signaling and support healthier oil flow from the meibomian glands over time. It’s not a quick fix, but used consistently, it can gently support tear stability, especially for people with dry, irritated, or allergy-prone eyes. Think of it as supportive, not curative.
And if light sensitivity or visual strain is part of your picture, VISION SCRIPT can be a thoughtful add-on. It’s designed to support retinal health and visual comfort rather than eyelid oil glands, so it doesn’t treat blepharitis directly—but for some people, supporting the visual system helps the eyes feel less reactive overall. It’s there if you want it, not something you have to do. Read this article on BLACK CURRANTS and VISION to see exactly why this might be better than fish oils for those of you with poor night vision.
- Gentle lid massage (simple, not aggressive).
After a warm compress, use clean fingers to gently massage the eyelids to help express the softened oils. With eyes closed, lightly sweep downward on the upper lids and upward on the lower lids, moving toward the lash line. This should feel calming, not painful. You’re encouraging flow, not squeezing toothpaste out of a tube.
What I usually recommend avoiding during this phase: Redness-relief drops, harsh cleansers, scented products near the eyes, and aggressive rubbing. If something stings “just a little,” that’s your cue to stop.
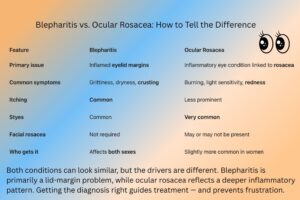
A Word About Ocular Rosacea
This eye condition comes up far too infrequently, so let’s take a brief detour.
Blepharitis and ocular rosacea can overlap, and they’re often confused. You can even have ocular rosacea without having rosacea on your skin, which surprises everyone. Here’s a simple way to think about it – look at the graphic I made.
Blepharitis tends to feel gritty and itchy. Ocular rosacea tends to feel more burning and light-sensitive. Both can exist together, which is why diagnosis isn’t very tidy.
Today’s focus is blepharitis – but if someone has intense burning, flushing, or heat triggers, that’s when ocular rosacea deserves consideration. The treatments are a little different.
If your symptoms aren’t improving after consistent home care, or if vision changes persist, light sensitivity worsens, or styes keep returning, that’s your signal to involve an eye doctor. Prescription treatments can help, but you’ll be surprised how much relief you can get from getting the basics right first. Scroll above to read what to do for quick relief.
My parting thought
Blepharitis is common. It’s manageable. And it’s often overlooked.
If your eyes feel dry but water or tear up…
If drops help for about 2 minutes, and then the discomfort comes back…
If things worsen as every day goes on…
…it may not be “just dry eyes.” It may be your eyelids asking for attention because it’s blepharitis. Getting the diagnosis accurate means you get proper treatment, and feel better soon. That’s my hope for you. If this helped you, or you have another idea to share that worked for you, write me at scriptessentials@gmail.com and I’ll add your comments below.

Suzy Cohen, has been a licensed pharmacist for over 30 years and believes the best approach to chronic illness is a combination of natural medicine and conventional. She founded her own dietary supplement company specializing in custom-formulas, some of which have patents. With a special focus on functional medicine, thyroid health and drug nutrient depletion, Suzy is the author of several related books including Thyroid Healthy, Drug Muggers, Diabetes Without Drugs, and a nationally syndicated column.