What's On This Page?
ToggleYour body is amazingly skilled at maintaining homeostasis and equilibrium of your ‘electric’ minerals. The minerals most important to your muscle and heart function include magnesium and calcium. Today’s focus is on calcium and hypercalcemia.
It’s kind of amazing how your body maintains tight control over calcium levels, especially the amount that is circulating in your blood at any given moment. For example, the thyroid gland will sense high calcium levels in the bloodstream, and in an effort to protect you, it will release a hormone called “calcitonin” which seeks to normalize calcium levels. Calcitonin has many other functions in the body, it’s an important hormone. See this graphic.
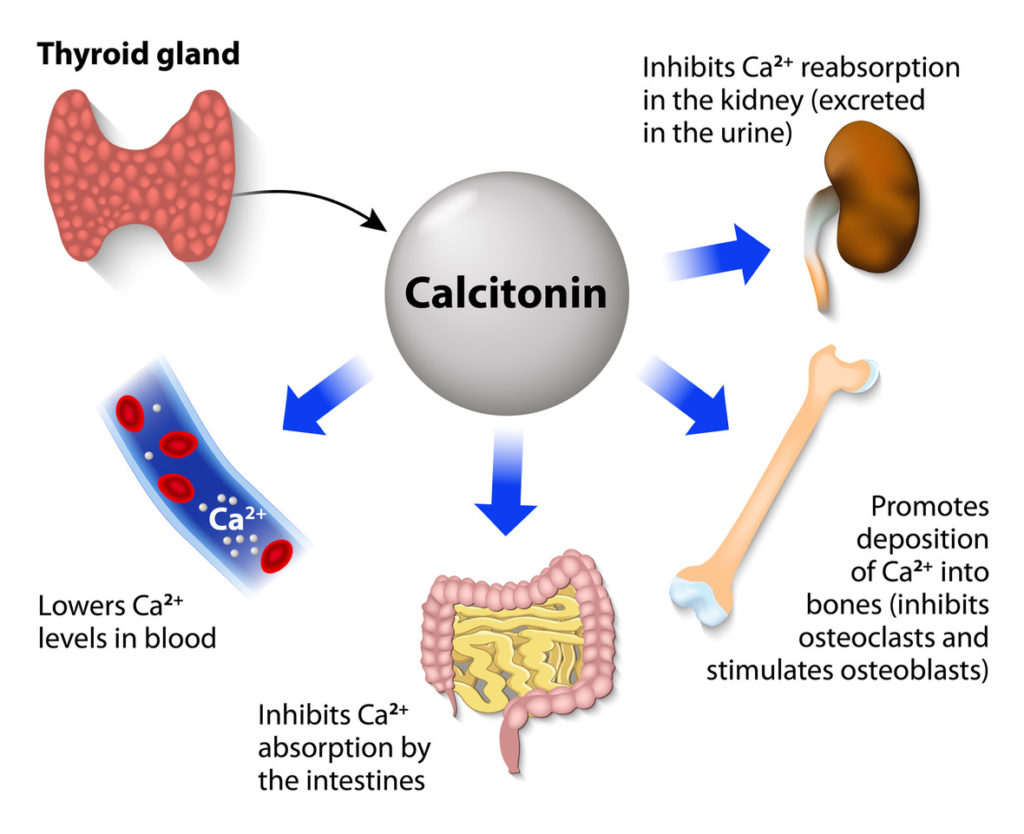
All of these methods are done involuntarily by your body to keep your serum calcium at a normal range, usually somewhere between 9 and 10, but it differs depending on your age.
1. Your intestines absorb calcium from foods that you eat.
2. Your bones give up and take in calcium so there is a dynamic movement of calcium in and out of your skeleton.
3. Your kidneys reclaim calcium or excrete it into your urine.
When the blood levels drop below normal, your 4 tiny parathyroid glands (the size of a grain of rice) immediately rescue levels by secreting parathyroid hormone (PTH) into your blood which tells your bones to release some into the blood, and do it NOW! So people with elevated PTH levels are at higher risk for osteoporosis. You can measure your levels of PTH by the way, it’s a simple blood test. If it’s high, I recommend you read about the subject at parathyroid.com, which compiles all of Dr Norman’s work in one amazing website. I will revisit PTH and parathyroid conditions in a future article, but one thing I want to say now is this.
Physicians will evaluate vitamin D if the PTH is elevated, and if the D is low they will tell you to supplement. This can be very harmful and is the wrong thing to do in most cases because if the PTH is elevated, and your D is low, it’s low because your body’s trying to protect you from more calcium! You may have a parathyroid adenoma (tumor) which is most often benign. So you should not supplement with vitamin D (in an effort to reduce PTH) because doing so will cause you to absorb more calcium from your meals, raising levels to potentially toxic amounts. See #1 above.
Symptoms of Hypercalcemia
Elevated calcium (Hypercalcemia) is bad for your health, it is kind of like getting ‘stoned’ to death. That’s why kidney stones are so common, as well as calcifications in the arteries. You may experience heart palpitations, muscle cramps, benign fasciculations, muscle twitches, easy fractures, bone pain, foot or leg cramps, upset stomach, nausea, and constipation. Kidney stones are another real possibility with Hypercalcemia and/or elevated PTH.
Chronic hypercalcemia can cause calcification of the arteries, plaque, as well as joint spurs. Calcium can be stimulating so you may also have broken sleep or insomnia. If left untreated, or if levels are high enough, it can lead to a heart attack or stroke. Hypercalcemia is a symptom that is important to check and find the root cause of.
So this is very important, taking vitamin D supplements when you have high PTH (and probably high calcium if you were to measure it) will only increase calcium levels. Upon doing an EKG, your cardiologist will now tell you to have cardiac abnormalities and maybe even Left Ventricular Hypertrophy. Now you’re down the rabbit hole!
So if your Vitamin D level is low, measure your PTH. If that is high, it is telling you that your body has innately known to reduce D as a protective measure. It’s been lowered by your own body in order to keep you from going toxic on calcium. Your body is truly amazing!
How is calcium measured?
A person’s calcium can be evaluated in several ways. Usually, a “serum” calcium is measured by a blood test. It’s easy and affordable. This is a general evaluation of how much TOTAL calcium is in your blood that is both bound to a protein and also free.
It’s a combination of the two values. To know the free, unbound calcium levels (which are really more important), you must ask for an “ionized calcium” blood test.
You could do both “serum” and “ionized” at the same time, with one tube of blood. Finally, you can see if you have so much calcium that it’s spilling into your urine in high amounts which are called hypercalciuria.
This test is called a “24-hour urine calcium test” and you just pee in a jug for 24 hours, then return the jug to your lab and they will test the amount of calcium over that 24-hour period. This test is particularly important if you are prone to kidney stones.
What can you take if your calcium is elevated?
I can offer some general ideas that I want you to ask your physician about. I caution you against self-treatment because consistently high calcium levels (Hypercalcemia) are indicative of many other conditions. For example, myeloma and leukaemia are both sometimes tied to hypercalcemia, and so is parathyroid adenoma.
Cancers of the breast, ovaries, and lungs can also cause the body to have calcium leached from the bones and put into the bloodstream, sparking elevated ionized and/or serum calcium. Assuming you are being treated by a qualified, licensed physician for your conditions, here are some ideas to discuss with him/her to help lower calcium:
1. Vitamin K2 – This refers to #2 above where I mentioned how your bones push calcium in and out of their structure. Bones are not “solid” as you might think, they are constantly building, and re-building themselves. Vitamin K2 drives calcium out of the blood and puts it back into the bone. It reduces serum calcium.
2. Bisphosphonates – This also refers to #2 above. The category of bisphosphonate drugs (ie Fosamax) can be used for a short term to remove calcium from the blood and put it back into the bones. It will reduced serum calcium.
3. Reflux drugs – Medications like famotidine (Pepcid) or omeprazole (Prilosec) can quickly reduce the absorption of many minerals and it can be quite potent. Some of these drugs reduce magnesium so profoundly that there’s a black box warning associated with their use! Magnesium is a mineral, it’s a cousin to calcium.
So taking reflux medication can temporarily help by addressing #1 above. It is reducing how much calcium you take in from your meals. Now there is one caveat about this statement, please read down below to #6.
I also want you to ask your doctor before self-treatment because even though these drugs are available over the counter, they’re not right for everyone. They can also crush your gut flora! They can increase the risk for food sensitivities over time as well, so ask a professional.
4. Follow a low-calcium diet – There are many lists on the Internet that show the calcium content of food. To summarize it here for you,
I’d say these foods are the lowest and best ones to consume if you have hypercalcemia: Meat and poultry, shrimp, seafood, green beans, eggs (and egg substitute), oatmeal, squash, nuts, rice, peas, Brussels sprouts, tangerines, kiwi and fruit juice.
5. Switch diuretics – If you are taking a thiazide diuretic like HCTZ (hydrochlorothiazide), this will cause you to retain calcium. By taking a “loop” diuretic such as furosemide, you will spill more calcium, and levels will come down.
This trick is something that addresses #3 above, about your kidneys re-claining calcium or excreting it. There’s a well-known correlation between thiazides and elevated PTH.
In other words, people taking thiazide drugs will often develop primary hyperparathyroidism, perhaps it is underlying but either way, you can review the ARTICLE and learn more.
6. Surgery – Sometimes surgery for a parathyroid adenoma is necessary. I will refer you to Dr. Norman’s website, parathyroid.com. If you have Hypercalcemia, and your PTH is normal (not elevated), you may still have a parathyroid adenoma which can easily be removed with a “mini” surgery.
7. Drink water – This increases your fluid volume, and may help bring down calcium temporarily. It’s a hack, but only useful if you’re dehydrated. Calcium will change day to day, so keep in mind that sometimes, the length of time you’ve suffered with undiagnosed hypercalcemia matters more than the actual number does.
Someone with a level of 10.9 for years might be facing more health challenges than someone who has had 11.2 for 2 weeks. But that said, every person is unique, so that’s just a general rule of thumb.
8. Vitex Agnes (Chasteberry) Extract – There is limited data to suggest this herb may be helpful in reducing calcium (serum), and supporting healthy parathyroid hormone (PTH) levels. Women who are pregnant should not take this. Because Chasteberry has a widespread effect on prolactin and other hormones, ask your practitioner if it’s right for you.
What to avoid with hypercalcemia?
* Avoid leafy greens like kale, spinach, chard, and also okra for a while. This is because they are tremendous sources of calcium and can trigger Hypercalcemia, and they are far richer in calcium than milk and ice cream! It shocks me that mustard greens are not that high in calcium compared to other greens.

* Avoid milk, cheese, and yogurt. These dairy items are rich sources of calcium. In fact, some people don’t realize this but evaporated milk and soy milk are particularly high in calcium. Surprisingly, sour cream and a small shmear of cream cheese on your bagel aren’t that bad in terms of their calcium content!
* Avoid supplements that raise calcium levels. You’d be surprised at how many herbs are rich in calcium and you may be taking them for one thing, but then they are simultaneously raising calcium because they are nutrient-dense. For example, oat straw herb is very rich in calcium.
* Avoid Vitamin D if you’re hypercalcemia because it causes you to absorb (and retain) more calcium.
* Discontinue calcium supplements – If this applies, and you are shown to be hypercalcemia, you should discontinue your supplements. You may not know this, however, both TUMS® and Rolaids® contain a great deal of calcium that can trigger Hypercalcemia.
These medications are used to treat reflux and acid indigestion but if you’re taking them frequently, you could be adding calcium to your body. Under normal conditions that’s alright, but if you have Hypercalcemia, this will be additive to the calcium your bloodstream is already holding.
* Reduce or discontinue estrogen supplements – Many post-menopausal women take estrogen-containing supplements (or creams) and this increases calcium absorption, leading to Hypercalcemia.
But like they say, too much of a good thing… As you know, estrogen is good to protect your bones of course, but again, your physician may want you to discontinue the hormones because they can increase PTH and they can lead to Hypercalcemia indirectly by increasing endogenous vitamin D production.
It’s a catch-22 and I realize that as I type this so I want you to ask your doctor. The catch-22 is that even though these herbs help prevent bone loss, they are also rich sources of calcium: Oat straw, calendula, alfalfa, hops, wild yam, sage, ginseng, and licorice.
* Avoid drugs or supplements that inhibit your kidney’s ability to excrete calcium or reduce blood flow – While there is conflicting evidence, vitamin A and retinoid drugs (ie Isotretinoin) may have some effect on bone remineralization. You may be wondering which drugs do this, so I”ll list them here for you:
-
Thiazide Diuretics (e.g., hydrochlorothiazide, chlorthalidone)
- These drugs increase calcium reabsorption in the kidneys, leading to higher calcium levels in the blood and reduced excretion.
-
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) (e.g., ibuprofen, naproxen)
- NSAIDs can reduce blood flow to the kidneys by inhibiting prostaglandins, which are important for maintaining adequate kidney blood flow.
-
ACE Inhibitors (e.g., lisinopril, enalapril)
- These drugs can reduce kidney blood flow, especially in people with kidney disease or dehydration.
-
Angiotensin II Receptor Blockers (ARBs) (e.g., losartan, valsartan)
- Like ACE inhibitors, ARBs can decrease blood flow to the kidneys and potentially reduce kidney function in vulnerable individuals.
-
Lithium carbonate (prescription) and Lithium orotate (over-the-counter)
- Lithium can impair the kidneys’ ability to excrete calcium and may cause long-term damage to kidney function.
Honorable mention: Prescribed vitamin A too. Just consider this and speak to your pharmacist about a medication you are taking to see if it hinders calcium excretion or not. Very high doses (not the type of dose in supplements) of Vitamin A may also be a problem and raise serum calcium.
* Avoid Horsetail herb (Equisetum arvense) – This is a common herbal remedy for vein health and hemorrhoids, and it is rich in calcium.
* Avoid Quercetin – It may raise serum levels of calcium and vitamin D. This is good for bone mineralization of course, however, it’s bad if you have pre-existing hypercalcemia.
* This is not an “avoid” supplement or drug for Hypercalcemia, but Lithium can lead to elevated levels of calcium. This is why patients who take lithium (either supplement of “lithium orotate” or prescribed lithium) require constant testing and medical supervision.
Do not suddenly stop your medication, just be aware that if your calcium is slightly elevated, it may be from your lithium. Talk to your doctor about this.
If you have any comments or hacks you’d like to share, you can always email me at scriptessentials@gmail.com.

Suzy Cohen, has been a licensed pharmacist for over 30 years and believes the best approach to chronic illness is a combination of natural medicine and conventional. She founded her own dietary supplement company specializing in custom-formulas, some of which have patents. With a special focus on functional medicine, thyroid health and drug nutrient depletion, Suzy is the author of several related books including Thyroid Healthy, Drug Muggers, Diabetes Without Drugs, and a nationally syndicated column.