What's On This Page?
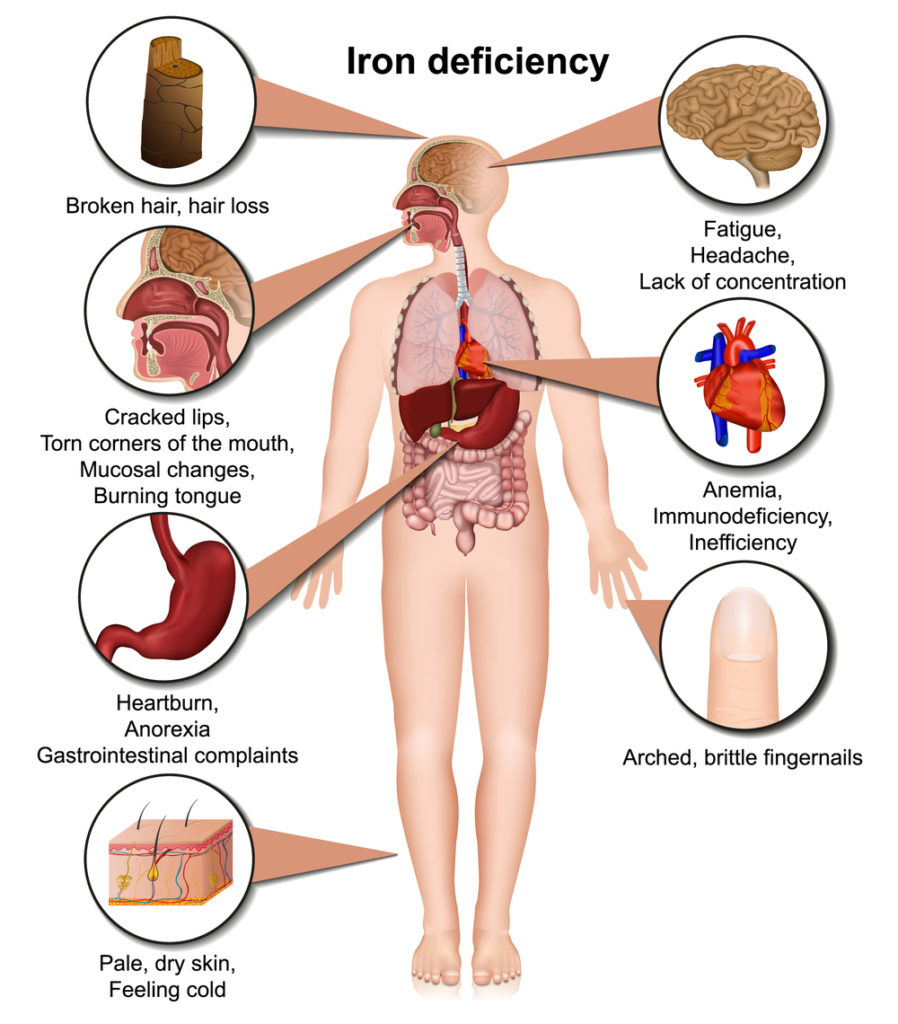
ToggleThe symptoms of low iron (aka iron deficiency) mimic those of hypothyroidism, and low iron levels go hand in hand with low thyroid levels. It usually occurs due to reduced gastric acid production as we age, which then reduces iron absorption.
The iron deficiency results in sluggish conversion of T4 to T3. Since iron deficiency goes hand in hand with hypothyroidism, I will be switching back and forth between the two conditions periodically.
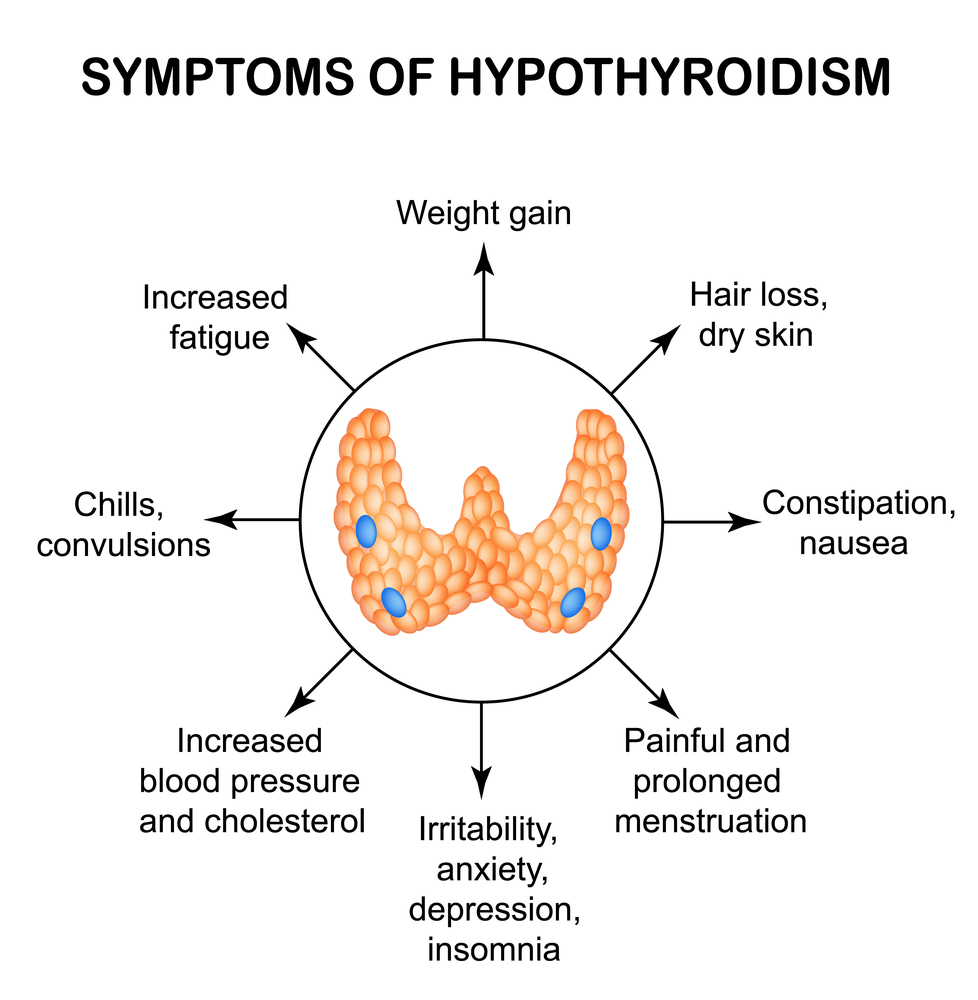
Iron Deficiency Looks Similar to Hypothyroidism – in terms of its presentation!
Symptoms for both of these conditions are similar. One common symptom of both low iron and hypothyroidism is exhaustion! You’ll feel fatigued which lasts all day, even if you slept well the prior night. Scroll down to the picture below to see some symptoms of iron deficiency.
People with low iron and low thyroid hormone often have reduced immunity (higher risk of cough/cold), slow wound healing, pale lips and skin, dizziness, weakness, hair loss, and mild depression.

The reason for the paleness (a hallmark symptom) is that your red blood cells store iron, and without enough iron, you have smaller, sicker, and fewer red blood cells (RBC). You’ll appear pale, so will your conjunctiva. Go ahead and pull down your lower eyelid and check to see if you have this.
Not everyone with iron deficiency anemia looks pale because you have to be very deficient in iron before you present with that specific symptom. Lips will match the color of your skin instead of being pink.
Furthermore, since your RBCs tote oxygen to your body’s organs and cells, you won’t have enough oxygen so you’ll feel weaker, short of breath, and easily tired. Speaking of shortness of breath, you may be interested in tips to remedy this frustrating condition. Read my other article, Revealing 15 Hidden Causes Of Shortness Of Breath And How To Overcome Them.
Iron and Pregnancy
Iron is important during pregnancy, and many women go into their pregnancy with years of low iron. In doing so, this raises the risk of problems (and death) for both mother and child. It’s hard to believe but worldwide, maternal and neonatal deaths account for about 2.5 to 3.4 million each year! For this reason, if you’re exhausted but want to get pregnant, it’s best to go ahead and test your iron (and thyroid) levels first.
You can easily correct both iron and thyroid deficiencies prior to conception and this will be an excellent safety precaution for both mother and child. Miscarriage risk is dramatically higher from deficiencies of either thyroid or iron. Again, thyroid hormone requires iron so when you’re low in one, you’re often (not always) low in both!
One more interesting tidbit…oral contraceptives appear to increase iron and copper levels so if you’re coming off those pills, you may not need to address anything. It’s a question for your OB/GYN or a simple blood test to be 100% sure.
Folate vs. Folic Acid
Before I leave the topic of pregnancy, the World Health Organization (WHO) recommends iron and folic acid supplements for the purpose of reducing anemia in women of reproductive age. Folic acid is a synthetic compound that does not in my estimate support a healthy pregnancy. In fact, its use is totally questionable because it will occupy the receptors where natural folate should go – competitively blocking entry of the real deal!
I think the WHO should revise its statement to say “folate” not “folic acid.” Perhaps one day they will realize the error because today, both folate and folic acid are widely available. As a woman seeking pregnancy, you should know that folate is the one that reduces birth defects.
Read more about the differences between folic acid and folate by CLICKING HERE to read my article, Nutrients You Need Before Pregnancy.
How is Iron Packed and Unpacked
Most iron (about 3.5 grams) is in the hemoglobin portion of your blood which is a protein that transports oxygen. Some of it is stored as “ferritin” too. Evaluating ferritin levels is the most affordable, and easy way to quickly assess iron levels, but it is not the most complete method. See below for more on ferritin.
Additionally, some of your iron is stored in the form of “hemosiderin” which is a breakdown by-product of ferritin. The organs that hold various forms of iron include your liver, spleen, bone marrow, and muscle tissue. This explains why anemic patients are told to eat organ meats such as liver…. because it is rich in iron. It also explains why people with anemia (diagnosed or not) are weak and tired… because their muscle cells don’t contain enough iron.
Iron Utilization
Iron is a crucial mineral for the human body, serving as a key component of hemoglobin, the protein in red blood cells that carries oxygen from the lungs to the rest of the body. This ‘heavy’ mineral, while essential, is regulated meticulously within the body to prevent both deficiency and excess. The transportation of iron throughout the body is managed by a protein known as transferrin, which binds iron ions in the bloodstream and delivers them to various tissues where they are needed.
The human body has mechanisms in place to both absorb and excrete iron, ensuring that its levels remain balanced. Iron is absorbed primarily in the duodenum and upper jejunum of the small intestine, with the rate of absorption being influenced by the body’s current iron stores and its demand for new red blood cells.
On the flip side, the body also excretes iron, albeit in much smaller quantities, through urine, feces, sweat, and cells shed from the skin and the inner lining of the gastrointestinal (GI) tract. For women, menstrual periods represent another significant avenue for iron loss, with heavy periods leading to greater iron depletion.
Let’s Talk About Hepcidin
Overseeing the delicate balance of iron distribution, absorption is a hormone called hepcidin. Produced by the liver, hepcidin plays a critical role in iron homeostasis by inhibiting the absorption of iron from the intestine and the release of iron from macrophages, cells that store and recycle iron from old red blood cells. By doing so, hepcidin prevents the potential toxicity of iron overload, ensuring that your iron levels stay in the normal/healthy range.
Interestingly, genetic factors can influence the regulation of iron in the body. Some of you carry a genetic single nucleotide polymorphism (what is called a SNP and pronounced “snip”) that affects the production or activity of hepcidin. The problem is that a deficiency in hepcidin due to such genetic variations can lead to a condition known as hemochromatosis, where the body absorbs too much iron from the diet.
The excess iron is then deposited in various organs, including the liver, heart, and pancreas, potentially causing damage and leading to serious health problems such as liver disease, heart problems, and diabetes.
The balance of iron within the body is a complex interplay of absorption, utilization, and excretion, tightly regulated by the protein transferrin and the peptide hormone hepcidin.
There are two forms of DIETARY iron:
1. Heme
2. Nonheme
As the name implies, heme iron comes from hemoglobin and it is found in animal-based foods such as liver, organ meat, poultry, red meat, fish, and some seafood. As for nonheme iron, you’ll find that in seafood as well as some plant-based foods like beans, legumes, and nuts. You are an animal, not a plant and therefore respond quicker to iron consumed from another animal (heme) sources.
Ferritin Testing: It can Help You Determine if You Have Low Iron
Today, you can self-order ferritin tests by going to my favorite “Any Lab Test Now” which are available in some cities around the country, or Labcorp or Quest locations, as well as many hospital labs. You just make an appointment or walk in and order tests nowadays, no physician is required (but I obviously do recommend they remain involved in your care and supervise you). Self-treatment for iron deficiency isn’t as easy as it sounds, lots of other hormones and minerals are involved.
Any medical doctor will order (or draw) this lab if you ask. It’s not one of those specialty tests. Hemoglobin and hematocrit tests are two other popular tests that help screen a person especially when these are drawn in tandem with ferritin and TIBC. In fact, I recommend you get a “Complete Iron Profile” rather than this test and that one and then another. It’s one needle stick and it looks at all the different iron biomarkers.
I’ve measured my ferritin over the years so I know a lot about this one. Low ferritin doesn’t necessarily qualify for “Iron Deficiency Anemia” as the actual condition. It is only suggestive of anemia if it’s between 11 and 30 mcg/L. But if your ferritin is less than 10 mcg/L then you are really anemic. Mine was super low (it was 8) for a while when I was in my early 40’s and I ended up finding out that it was tied to hypothyroidism which I didn’t know I had! I was very tired, dizzy, and pale and it came on pretty suddenly.
 After fixing this condition myself and raising my ferritin to healthy levels, I wrote a book on it called, Thyroid Healthy: Lose Weight Look Beautiful and Live the Life You Imagine. In this book, I cover both medical and nutrient/diet recommendations. It also has a chapter about Graves’ disease and Hashimoto’s. You can read reviews on Amazon HERE.
After fixing this condition myself and raising my ferritin to healthy levels, I wrote a book on it called, Thyroid Healthy: Lose Weight Look Beautiful and Live the Life You Imagine. In this book, I cover both medical and nutrient/diet recommendations. It also has a chapter about Graves’ disease and Hashimoto’s. You can read reviews on Amazon HERE.
The confusing part is that serum ferritin can be influenced by many factors and may go up and down depending on different factors:
1. Inflammation from autoimmune disorders or pathogens
2. Infectious diseases – some of them elevate ferritin, while others reduce it
3. Pregnancy – demand for iron goes up due to the developing baby
4. Orange juice that you drink right before your ferritin blood test
5. Medications that deplete iron from your body, what I call “drug muggers” of iron
Almost all infecting organisms that I know of the can and do use iron. They need it either for their biological processes or their transport, so iron depletion can often occur with pathogens. I’d term it this way: Pathogens are drug muggers of iron! The only exception that comes to mind off the top of my head is Borrelia burgdorferi -the official Lyme bug- which is a drug mugger of manganese, not iron.
That one found a hack! That is treated with doxycycline usually, so as long as I’m thinking about it, I’ll tell you that you should not combine iron with doxycycline, tetracycline or minocycline. If you take iron with those antibiotics, you will reduce the effect of the antibiotic so separate administration. Take the iron 2 hours before the antibiotic, or 4 hours afterward to avoid the possibility of low iron.
Finding Low Iron
The symptoms of iron deficiency mimic other conditions, so it can be very complex for a practitioner to recognize what’s going on. Iron is required by almost all organisms because it serves as an essential cofactor in their ‘spreadability.’ It’s not to be feared, but rather respected. Here’s why… iron can be very toxic in high concentrations because it turns into a cellular weapon (ie free “oxidative” radical). This harms the cell.
So just like everything else in the body, homeostasis or balance is critical to good health. So if iron is being depleted from your body due to an organism, do you treat and kill the organism, or do you keep replenishing the iron, or do you do both… and in what order? These are all good questions, and you along with your supervising physician will know what is right for you.
Some pathogens use iron and over the years, they massively deplete your iron stores! One example of this is Babesia (a co-infection of Lyme disease that one gets from an infected tick). You may not know you have Babesia if you’re asymptomatic, however, your blood cells will still be invaded by the parasite, and they will be destroyed.
That means a man or woman who has idiopathic iron deficiency (meaning there’s no discernible root cause) could have Babesia which is causing hemolytic anemia. Igenex can test for this pathogen. If the topic of Lyme interests you, read my other article related to this, If You Think Lyme is Bad, Meet Babesia.
These are the main ‘drug muggers’ of Iron
1. Aspirin.
Used for arthritis, fever, cardiovascular disease, and platelet inhibition
2. Acid suppressing drugs (a.k.a. Acid Blockers).
Used mainly for reflux, peptic/duodenal ulcer, GERD, chronic heartburn, Zollinger-Ellison syndrome, or Barrett’s esophagus. That last condition “Barrett’s esophagus” is linked to chronic heartburn, and can turn into cancer of the esophagus. There are several categories within the category of acid blockers. I’ll break the acid blockers into the 2 main categories of H2 antagonists and PPIs.
*** H2 antagonists.
 Pepcid, Zantac, and Tagamet are examples of “H2 antagonist” acid blockers.
Pepcid, Zantac, and Tagamet are examples of “H2 antagonist” acid blockers.
These are a sub-type of acid-blocking drugs. These drugs latch hold of H2 receptors in your stomach cells and reduce the production and secretion of stomach acid, reducing your ability to extract iron from your meals. As a result, over time low iron levels may occur, but it’s not a guarantee of course! By the way, other nutrients that these drugs steal include calcium, folate, vitamin B12, vitamin D, probiotics, and possibly others.
*** Proton-Pump Inhibitors or PPIs.
These are another sub-type of acid blockers and they are strong drug muggers of iron. You may recognize them by their brand names like Nexium, Prevacid, Prilosec, and others. These drugs block the acid transporter “proton” pump permanently… like, they grab hold and DO NOT LET GO of the receptor site! Picture a pit bull hanging onto a T-bone! So with the PPIs, the acid suppression is strong and long-lasting. That’s why you only take them once a day. So the iron deficiency that may result is more pronounced than with H2 antagonists or antacids. Let’s talk about those next.
3. Antacids.
Antacids raise pH in the stomach by directly neutralizing acid. When you suppress acid like this, you can no longer extract iron from the foods you eat… or any mineral really! The effect isn’t strong so if you eat a bowl of hot salsa and then get heartburn, an antacid is all you need to do the trick. You don’t need a PPI for a one-time indulgence. The risk of iron deficiency with these is also slim to none unless you take them every day.
4. Indomethacin, Naproxen and Ibuprofen a.k.a. NSAIDS.
The category of NSAIDs (non-steroidal anti-inflammatory drugs) can deplete iron levels. If you take these medications once in a while, it’s no problem. If you’re supported on them daily, then you may want to check your iron status. It’s because the NSAIDs irritate the GI tract and cause GI loss. In the elderly, this effect is quite pronounced and dangerous.
Iron supplements can also cause GI irritation so it’s a catch-22. If you’re taking an NSAID daily, and have symptoms of iron deficiency (or hypothyroidism) then do an iron profile annually. Iron supplementation is rarely needed for PRN use of NSAIDs. I think you know this but just in case… PRN is pharmacist jargon for “as needed.” So again, PRN’s use of the NSAIDs will not necessitate the need for iron supplements.
5. Calcium supplements.
Often taken by women for osteoporosis, calcium supplements may alter your levels of iron if you take a high dose. Calcium decreases the amount of iron (specifically heme iron) absorbed from your meal. It raises pH and therefore suppresses acid. Some people take calcium in the form of Rolaids too. If you have ever had parathyroid surgery, you may need to take more calcium. I share my journey about this condition, and having hyperparathyroidism in this BLOG in case you’d like to learn more.  6. Coffee
6. Coffee
7. Tannins in Herbal Teas
Studies have shown that coffee is a drug mugger of iron. But what about something as simple as peppermint tea? The answer is yes, but the depletion is not strong, so therefore it’s not something you need to really supplement with iron for.
Here are some herbs that you might be taking which are mild drug muggers of iron. Consuming these may cause low iron. I just want you to be aware… again, enjoying these does not mean you have to take iron supplements!
- Hibiscus
- Ginger
- Chamomile
- Cinnamon
- Clove
- Nettles
- Peppermint
- Raspberry
8. Babesia – See above, discussed earlier in this article.
About Thyroid and low Iron
The relationship between levothyroxine (a popular T4 thyroid drug) and iron is a little complex. There is evidence that shows thyroid hormones increase iron absorption and iron incorporation into erythrocytes (thus raising ferritin levels). These studies show increased TSH and lower serum T3 and T4 levels in iron-deficient subjects, meaning they’re more hypothyroid.
But there is also good evidence showing that iron deficiency might negatively affect thyroid metabolism by reducing oxygen transport and T3 binding and TPO activity. Let your physician test you for a few things to see if this fits you.
If you take thyroid medication and you still have persistent hypothyroidism, it may be due to the fact that you have an iron deficiency. A small study determined that years ago, and it explains why no matter how much thyroid hormone you take, you still feel terrible. This situation occurs in 30 to 50% of people with persistent hypothyroid symptoms (even while on Levo or other drugs). Such was the case for me I had both (low thyroid hormone and low iron).
The way I got better was by taking care of both deficiencies and it took me two years to do it! There are lots of studies online to peruse if this interests you. By the way, you cannot supplement with iron at the same time as Synthroid (Levothyroxine). Ferrous sulfate reduces thyroxine (T4) absorption if taken together.
How to Raise Iron Levels
As you have seen, iron is depleted by many medications, some herbs, and even coffee! But this doesn’t mean you have to supplement. I believe in looking at ferritin and iron levels, not just randomly supplementing. And that may sound weird to you because if you have all the symptoms of iron deficiency, you might be tempted to supplement. The danger in that is that symptoms of hypothyroidism look exactly the same as iron deficiency anemia.
Taking care of the latter (ie addressing the root cause of hypothyroidism) would shift your iron, and that’s better than supplementing with iron for years! Taking too much iron will increase free radical species like ROS and cause undue oxidative stress and side effects. It’s not a pill you want to pop just because your ferritin is low.
How to Raise Low Iron
1. Supplements.
The obvious way is through dietary supplements sold over-the-counter at any pharmacy. It’s not my first choice and I don’t recommend this for low iron unless you stop after a couple of months. You can’t stay on those supplements forever. They are also very harsh on the stomach and cause gas, nausea, and stomach pain, so take them with food to try to minimize this.
2. Intramuscular injections of Dextran.
A physician has to administer this and it’s used as a last resort due to the side effects. While rare, they can be frightening. Some patients have experienced fainting or a light-headed feeling, flushing and tingling in the body, blue lips, pink urine, shallow or slowed breathing (or serious respiratory distress), or seizures.

3. Iron-rich Foods
Beef, chicken, ham, giblets, or organ meat (ie liver) are rich sources of heme iron. Egg yolks are another rich source of iron. So are sardines, clams, mussels, and oysters. Some animal protein contains nonheme iron because they’re eating the plants. Some vegan foods provide nonheme iron such as lentils, spinach, beans, cashews, and fortified cereal. Our bodies are somewhat less efficient at absorbing nonheme iron from plants.
4. Orange juice or vitamin C.
This raises low iron by enhancing your absorption of plant-based iron during a meal. It doesn’t make iron though.
5. Acid in the form of Betaine Hydrochloride Supplements.
Betaine HCL will raise iron indirectly because it helps you extract more iron from your food. But if you don’t need acid, or can’t tolerate it, it will give you bad heartburn! So please be careful with these supplements and follow directions for them very carefully or you could wind up with chest pain and heartburn and serious discomfort! Less is more with these supplements.
But I want you to know that these can be incredible in terms of naturally raising low iron levels because they help you absorb the mineral better than if you have hypochlorhydria. I wrote a fascinating article entitled, Strangely, Acid May Ease the Burn. If you take betaine, you do not need and should not use iron supplements.
It’s fairly easy to detect low iron and correct deficiencies. The use of supplements of iron is something you can do for a short period of time, however, there are better ways to obtain raise low iron. For example, minimizing the foods, coffee, and medications that mug it, while simultaneously raising levels through diet. Heme iron (as opposed to nonheme iron foods) is the fastest
The hallmark symptoms of low iron include weakness, fatigue, shortness of breath, and paleness. Some people have “spoon” nails. You may also have dizziness, anxiety, cold hands and feet, and occasional abnormal heart rhythm changes. It often goes hand in hand with low thyroid hormone which has the same exact symptoms!
If you have low iron (or the symptoms I’ve described) you should ask yourself if this is driven by hypothyroidism or an infection like Babesia. Is it possibly related to a medication you take each day? Is it perhaps related to something entirely different than what I’ve covered today in my article?
Spend some time testing and thinking it through, don’t just buy an iron pill because that doesn’t solve the root cause.
Today you can test your own ferritin and share the results with your doctor in order to determine what is best for you. Seek your practitioner’s guidance for all medical conditions since I am just providing information about low iron, not medical advice.

Suzy Cohen, has been a licensed pharmacist for over 30 years and believes the best approach to chronic illness is a combination of natural medicine and conventional. She founded her own dietary supplement company specializing in custom-formulas, some of which have patents. With a special focus on functional medicine, thyroid health and drug nutrient depletion, Suzy is the author of several related books including Thyroid Healthy, Drug Muggers, Diabetes Without Drugs, and a nationally syndicated column.