What's On This Page?
ToggleLet me ask you a question: Are you miserable in your skin, and not sure why?
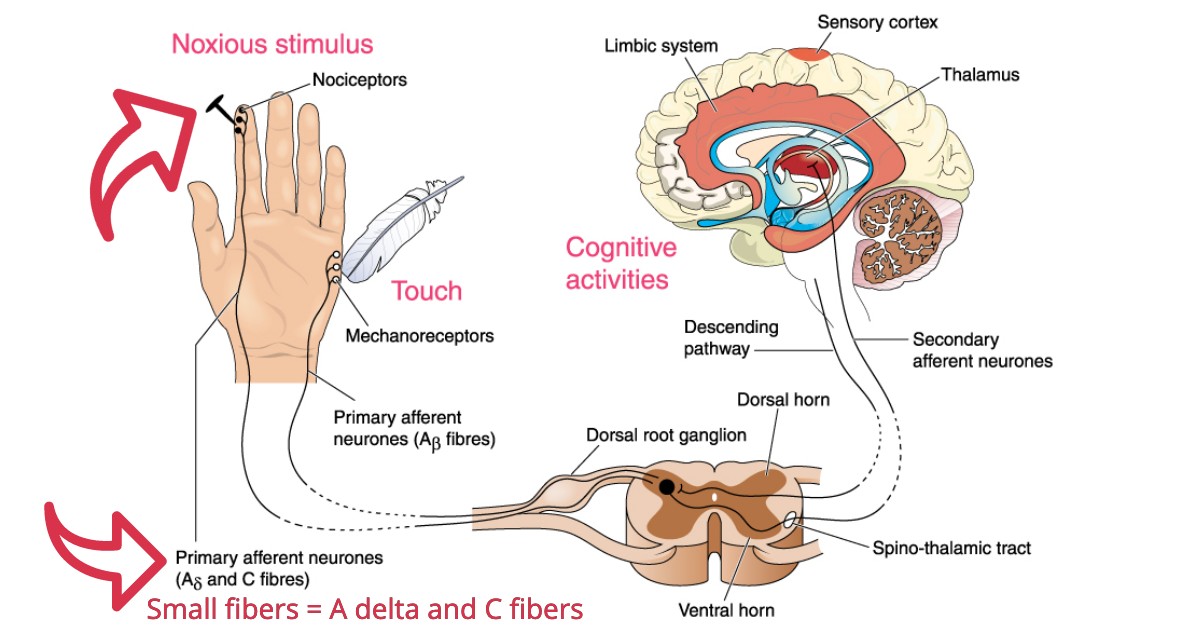
You’re only supposed to hurt if something pokes you or there’s a legitimate reason. But what if your pain-sensing fibers are going off for no reason? What if those nerve endings are just firing signals of pain when nothing happened to you?
That is how neuropathy could be described. It’s the sensation of pain (or prickliness or heat) when there’s no provocation! The medical term for these inexplicable neuropathic ‘weird’ sensations you feel is paresthesias.
There is neuropathy, and then there is small fiber neuropathy! There’s a very distinct difference between the two conditions. Do not dismiss what I’m about to share because you think it’s no different than typical “neuropathy.” In fact, if you think you’re going crazy and that you’re a hypochondriac, STOP.
I am about to prove that your chronic, ever-changing but never-ending symptoms have a real and treatable root cause. No one will think it’s just in your head anymore.
Small fiber neuropathy is a type of peripheral neuropathy that causes various different sensory sensations. There is much less known about small fiber neuropathy compared to typical “peripheral neuropathy” but that’s because doctors aren’t routinely testing for it yet and it has not been widely studied.
I believe it’s far more common than we are aware of, but so far it does not have mainstream attention. About 90% of people who have this condition don’t even know they have it. I will change that today because my articles are printed in newspapers nationwide and posted online all over the world in various language translations. So I know that in time, more medical professionals will be diagnosing their patients with it, plus more research will be conducted which will help us find more treatments.
About Small Fiber Neuropathy (SFN) and Autoimmunity.
You might have small fiber neuropathy (SFN), but if it’s not diagnosed properly, these small fiber problems lead to big problems. Small fiber neuropathy is often an autoimmune-driven disorder. It can be tested by counting the nerve endings from a small piece of skin (under a microscope). The small piece of skin is removed from you via puncture, and it’s called a skin biopsy, or an Epidermal Nerve Fiber Density (ENFD) test.
There is sometimes an autoimmune component to this type of neuropathy. The reason this is even possible is that the small fibers have contact with immune cells and mast cells. An autoimmune attack will cause your body to attack your own small fibers because they’re visible – they project outside the barrier that protects the large fibers.
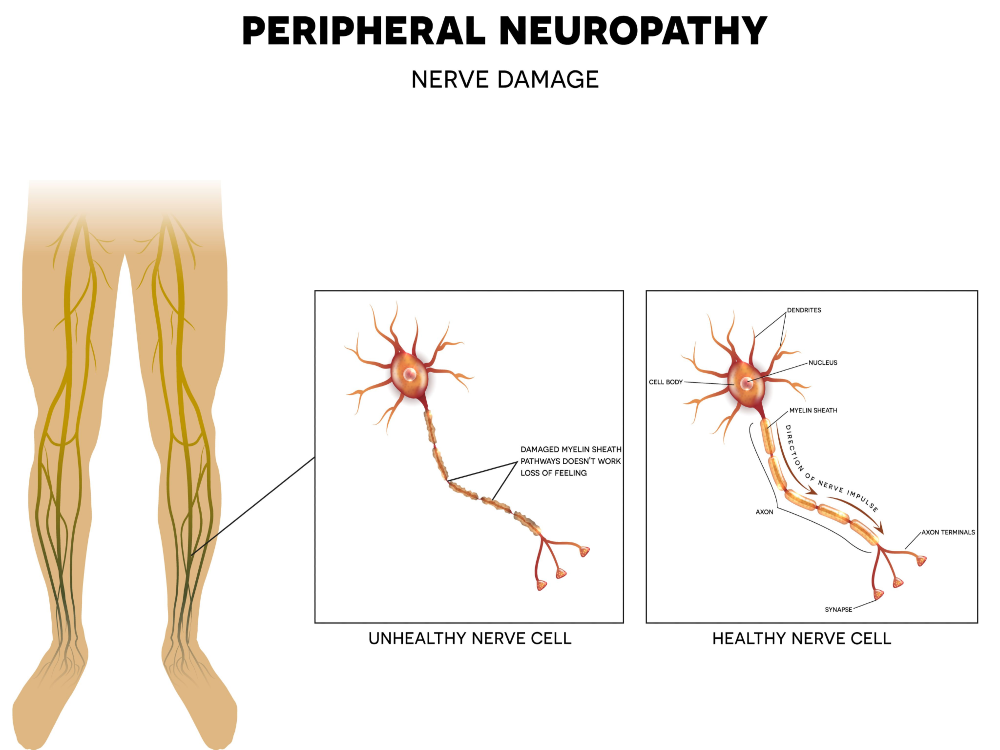
In other words, the larger fibers of the nervous system do not come into contact with the immune cells, they’re barricaded -that’s why you don’t see regular “peripheral neuropathy” driven by autoimmune disorders as its underlying cause. Contrarily, Small fiber neuropathy can be caused by autoimmune disorders. This is important because many people don’t know they even have an autoimmune disorder because it’s so mild, yet they’re already showing signs and symptoms of small fiber neuropathy.
Within a few years, your health may deteriorate to the point of moderate to severe functional disability. It is a treatable condition because these small fibers NEVER stop growing. They grow faster than the large fibers. You just have to find out what is damaging them, and stop it. If it’s autoimmune, and most likely is, then controlling the self-attack will help. Then a full recovery could happen because these small fibers will continue to generate.
I want to give you hope while educating you about the disorder. I’ve spent a long time writing this important article because it will help so many people who are suffering and don’t know what they have!
I surely hope it changes your life for the better. (Please share this article on social media if you like it).
Same condition, but it has different names:
SFN = small fiber neuropathy
SFPN = small fiber polyneuropathy neuropathy
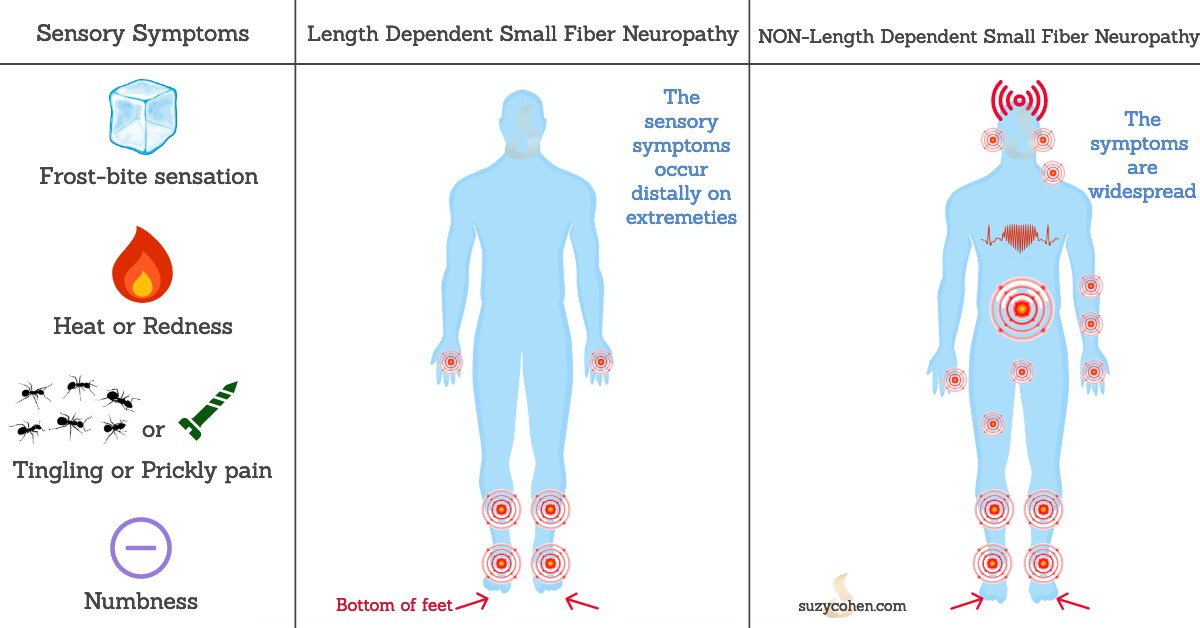
There are TWO types of Small fiber neuropathy – see my graphic below for more info.
1. Length-dependent Small fiber neuropathy
2. Non-Length dependent Small fiber neuropathy
(Please contact me to repost any of my graphics shown or this article: scriptessentials@gmail.com)
Only the small cutaneous (skin) nerves are affected in Small fiber neuropathy.
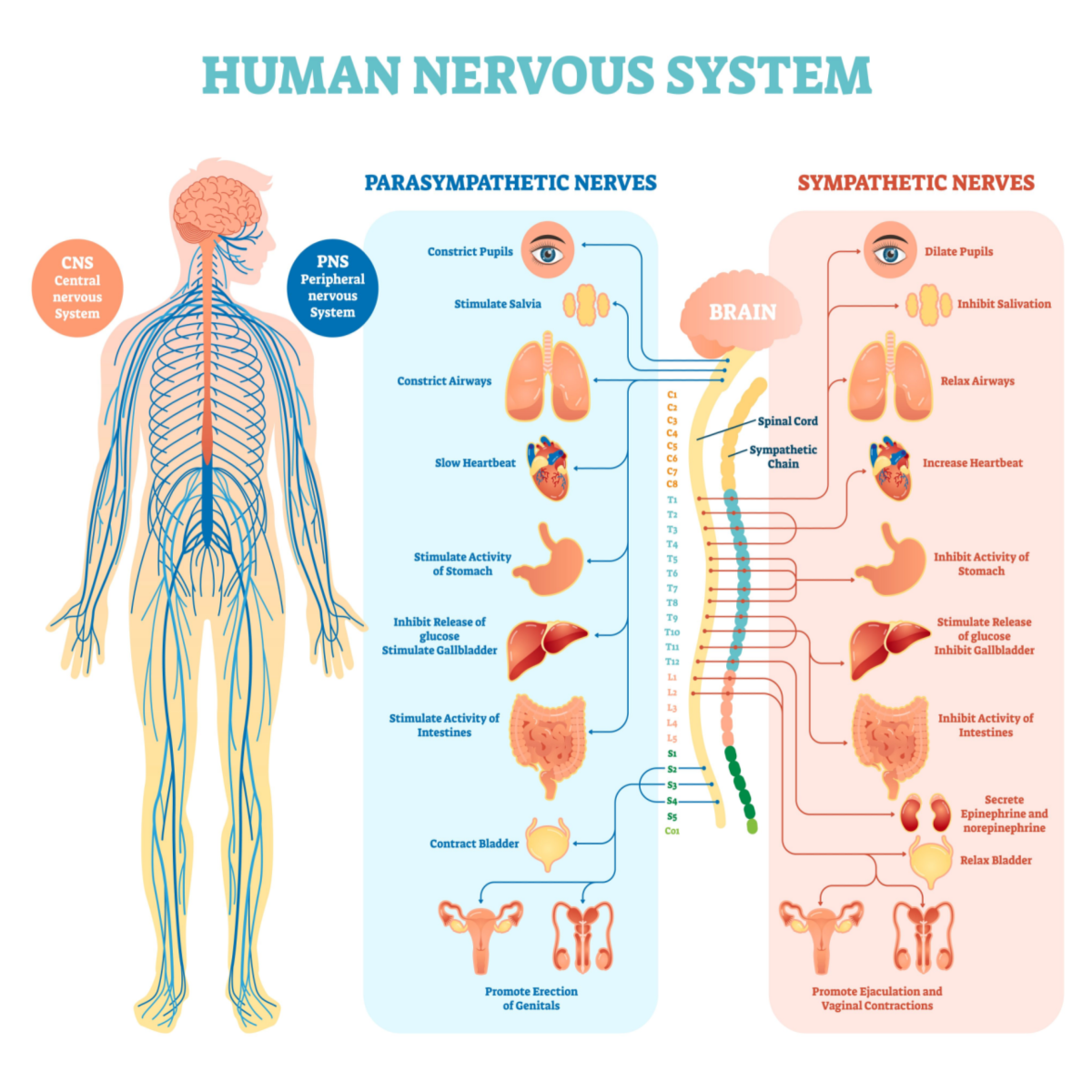
It usually starts in the feet/legs and moves upward to the hands/arms and then eventually all over! The main difference between Small fiber neuropathy and typical peripheral neuropathy (PN) is that SFN most often attacks the “small fibers” hence the name “small fiber neuropathy,” and it begins with odd sensations in the feet. Most other types of neuropathy have some degree of demyelination occurring, but again, the fibers destroyed in Small fiber neuropathy are the SMALL fibers, like the unmyelinated C fibers which handle autonomic input.
On occasion, some individuals with Small fiber neuropathy also experience damage to their myelinated “A delta” nerve fibers. These types of small nerve fibers are responsible for conveying sensations of pain, pressure and temperature to your brain. That’s why damage to these fibers causes such a variety of both sensory and autonomic problems. It also explains why Small fiber neuropathy evades proper diagnosis – it looks like a menagerie of different diseases!
Over time, the neuropathic symptoms are no longer distal (length-dependent), but they begin to progress upwards and throughout the body, first up into the legs… then the fingers and hands, and then you have abdominal symptoms, reflux, esophageal problems (early satiety) and more and more – into the small fibers of the heart causing rhythm disturbances… into the brain, and eyes and it doesn’t ever stop! You may have better days with one symptom, but another flares up.
How is it happening?
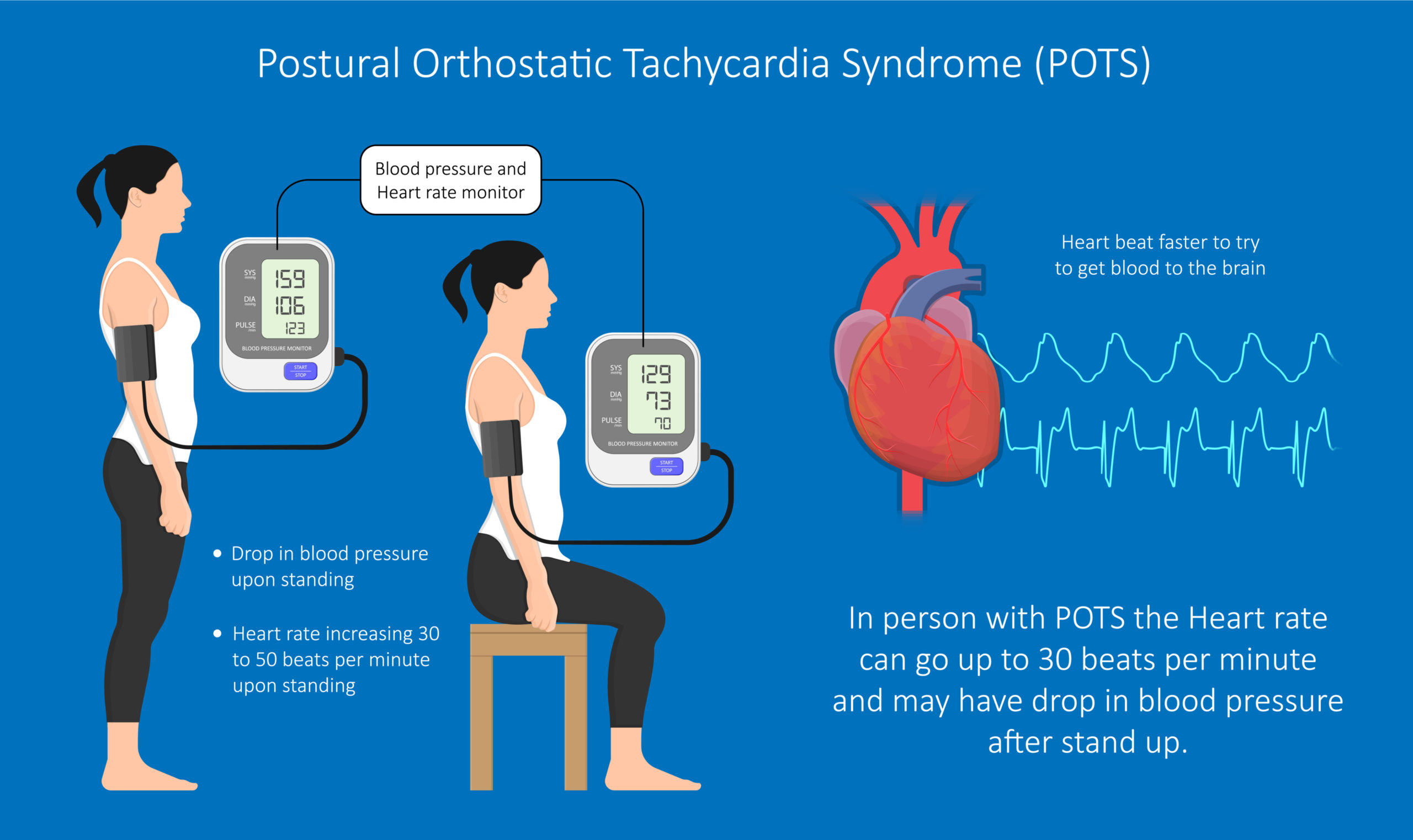
You may wonder how small fibers on the skin can create widespread havoc all over the body, but these small fibers innervate all of your internal organs, including the heart, lungs, gastrointestinal tract, brain, bladder, pancreas, and everywhere! When small fibers are destroyed throughout the body, you will be running around to doctor after doctor trying to figure out why your whole body is annoying you. So SFN isn’t just a skin sensory condition, it’s a full-blown systemic disease. And it can make you dizzy too! As in POTS (Postural Orthostatic Tachycardia Syndrome). I wrote an article about the use of choline in POTS which you can read HERE.
I believe that many people with many painful and disabling conditions remain misdiagnosed for years because SFN is not thought of, and never tested for. For example, I am sure there’s a good percentage of people who have POTS but may also have long-standing Small fiber neuropathy that went undetected and untreated.
POTS May Be Associated with Small fiber neuropathy in Some People
If there’s one thing that bothers me, it is misdiagnosis. I hate those because I’ve witnessed my sweet husband Sam get repeatedly misdiagnosed! Over the years, each incorrect diagnosis he was pinned with become agonizing for the whole family and lead to the use of expensive and harsh treatments which made things worse. So proper diagnosis of any illness is critical.
Let me ask you again: Are you miserable in your skin, and not sure why?
Symptoms of Small Fiber Neuropathy
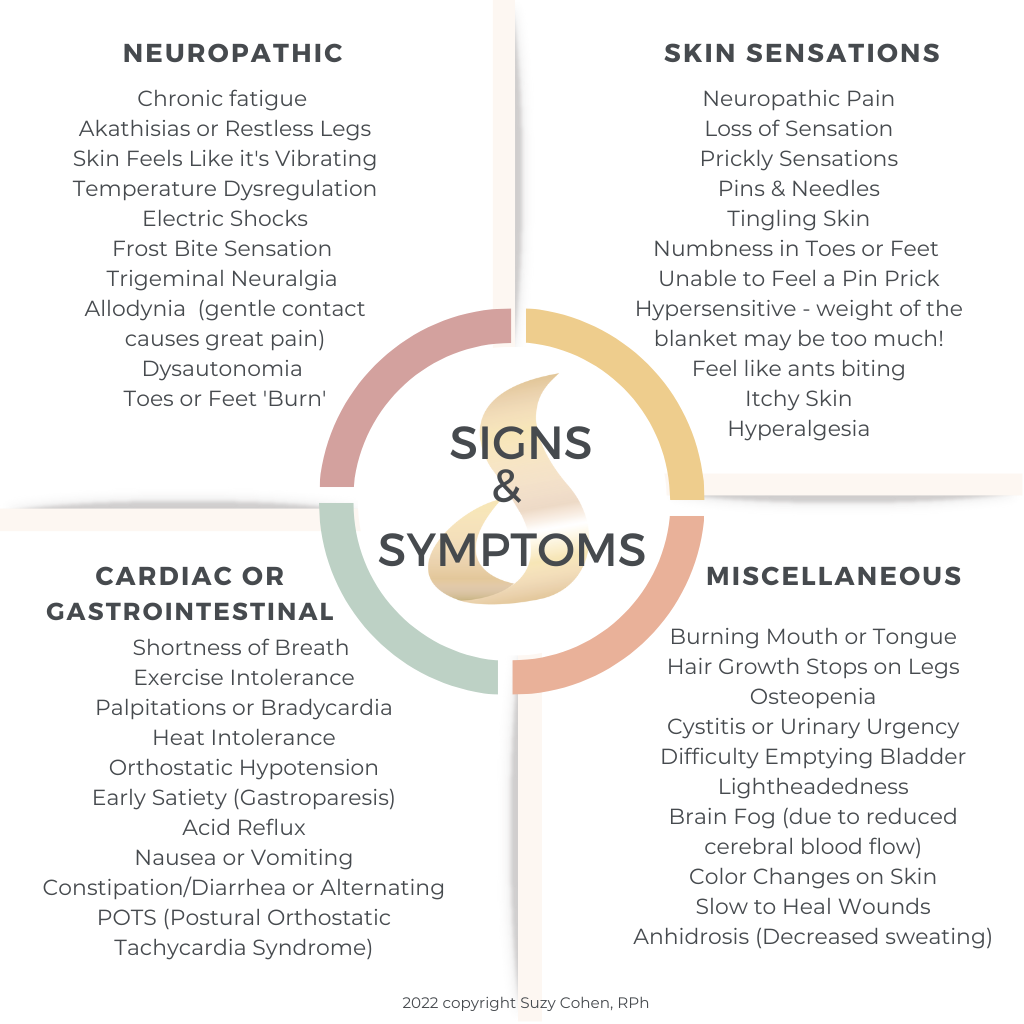
In the early stages, the signs and symptoms are sensory in nature and there is no organ involvement. It’s mainly sensations on the skin in the beginning.
One major hallmark symptom of Small fiber neuropathy is chronic fatigue. Another is pain. It can be widespread (possibly moving around your body) but the pain often begins in distal areas. There is usually no easily discernible etiology.
The “fatigue” occurs because the nerves that go to the blood vessels which then nourish the muscles have been damaged. If there’s neuropathy, the blood vessels don’t get the right signals and the heart muscle doesn’t work properly, so you feel easily fatigued, winded, short of breath, and have exercise intolerance.
If you were to do an ultrasound or other work-up on your heart, the organ itself would be fine, the muscles too. Tests would not reveal an organic cause for your heart condition per se, it’s more related to the fact that your heart muscle isn’t getting proper nourishment, causing poor blood flow, shortness of breath, and the need to lay around in bed and rest. This type of chronic fatigue is common with Small fiber neuropathy, yet rarely picked up.
Signs and Symptoms
The signs and symptoms listed below are the most common ones. There are others. I’ve listed the symptoms for BOTH the length-dependent and the non-length-dependent Small Fiber Neuropathy conditions.
You don’t have to have all of the symptoms, most people do not.
This condition begins in the feet with unusual skin sensations and progresses upward in the body if left untreated. Later, the hands and fingers become affected, and finally, symptoms may start afflicting your whole body, kind of like a spinning dial! This gets better one day, but that begins, and on and on...
The symptoms are difficult to describe accurately for each of you reading, and that’s because when your nerves are affected the sensations vary minute to minute. Also, descriptions of these sensations vary from person to person. One person may say “it feels like I’m walking on a bed of nails” and another may describe it as “I feel like a hundred ants are biting me.
Primary Signs and Symptoms of Small Fiber Neuropathy
By the way, you don’t have to ALL these symptoms, of course, you won’t! But if you have some of them, you need to get tested (see below).
Over time, the odd symptoms of Small fiber neuropathy become more generalized and widespread in the body creating a myriad of maddening symptoms that makes you feel like a hypochondriac. But you’re not. One doctor for this, another for that, in a never-ending cycle of physicians, blood tests, imaging scans, and dangerous, addictive drugs!
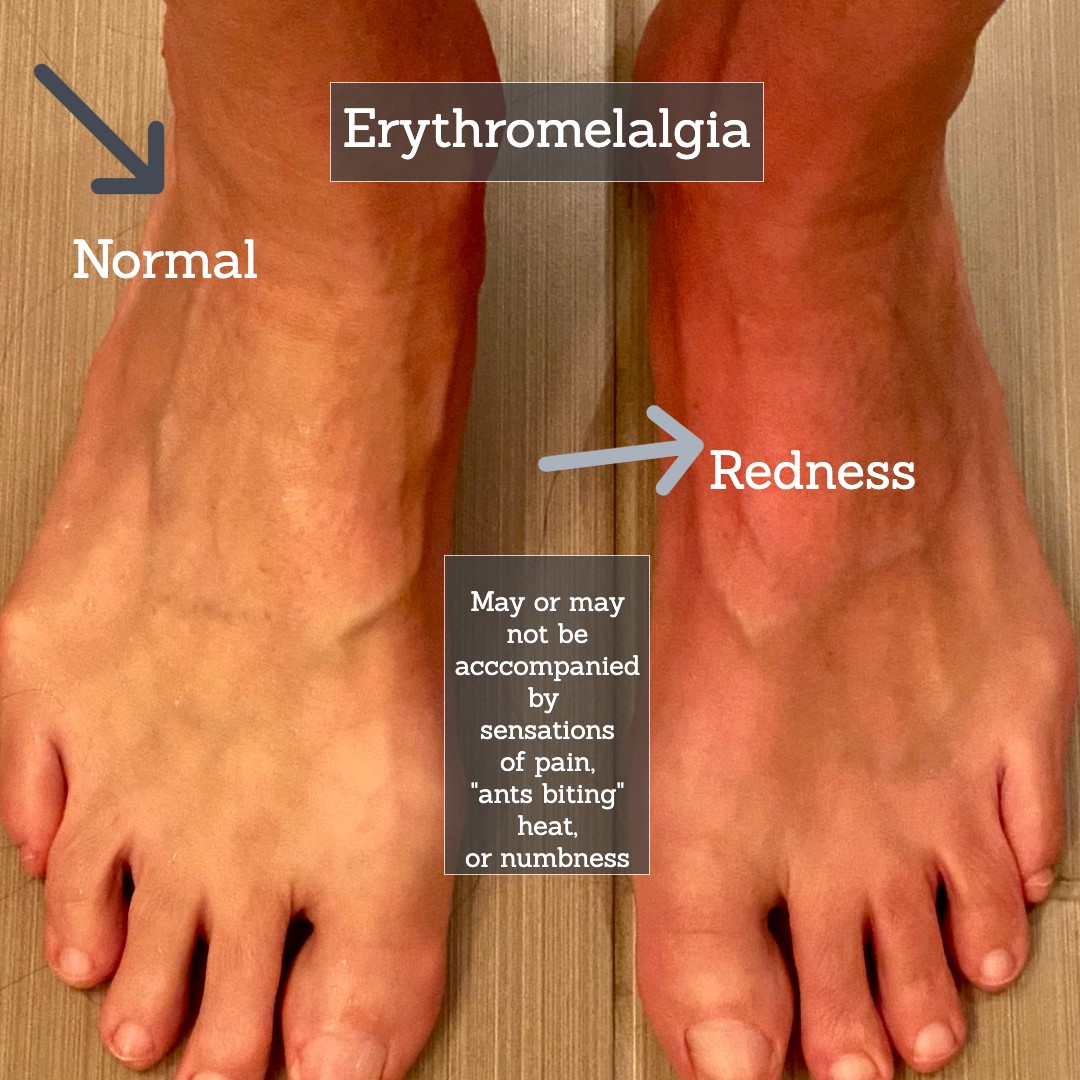
* Erythromelalgia is characterized by episodes of redness, heat, pain, or mild swelling in the feet usually. It’s usually triggered by raising your body temperature. When you get out of the shower, hot tub, or steam room you may discover one or both of your feet has turned red. The temporary problem goes away after a few minutes. About 50% of people with SFN have this.
Small fiber neuropathy disorder is not discussed much (I hope to change that today) because most people especially those with diabetes are diagnosed with “peripheral neuropathy.” That’s the end of it. SFN is never even checked for!
Today’s focus is to educate you about Small fiber neuropathy so you can recognize it yourself, and push harder for tests and treatment. It’s so frequently missed that you could have this condition for 20 years and see 100 different specialists and still never once hear about it!

may be Small Fiber Neuropathy
Burning Feet Syndrome
There’s such a lack of awareness about this condition that millions of people have the diagnosis of “Burning Feet” syndrome a.k.a. Grierson-Gopalan Syndrome.
So you go to the doctor and tell them your feet feel like they’re on fire sometimes, and you leave with the diagnosis of “Burning Feet” syndrome, which is of little help since your “diagnosis” conveys nothing more than the description of how you feel! It’s such an outdated understanding of the situation.
So I think everyone with Burning Feet syndrome should be tested for Small fiber neuropathy, and I suspect many of you are going to show positive biopsies for Small fiber neuropathy. If that happens, then you could actually seek useful treatment and that would be incredible.
Burning Mouth Syndrome or “Burning Tongue” is such a painful, upsetting condition that sometimes drives people to suicide! It was demonstrated back in 2005 that this painful sensory condition may be related (in some cases) to Small fiber neuropathy of the trigeminal nerve. You can read more about that HERE and HERE.
Diagnosis and Detection of Small Fiber Neuropathy
Diagnosing Small fiber neuropathy is not that difficult if you know exactly what to look for. Unlike similar neuropathic conditions, muscle strength remains normal and so do your reflexes. Even nerve biopsies will be normal. MRIs will be normal.
Because of this, it can be confusing. The EMG will be normal too! So if your doctor conducts a regular EMG (electromyography) study on you, and it’s normal, then your physician may stop there. Do not let him/her stop there.
In other words, you might get dismissed if your EMG study is normal even though you have SFN. But again, the damage done by Small Fiber Neuropathy will not be revealed in an EMG study. So please do not ever depend on an EMG study to confirm Small fiber neuropathy. That’s not how you test for small fiber neuropathy.
Scroll down below for testing labs. The condition must be ruled in or ruled out properly and tested objectively by doing an epidermal (skin) biopsy. Nerve conduction studies will usually be normal with Small fiber neuropathy. I made a graphic to try to summarize this for you.
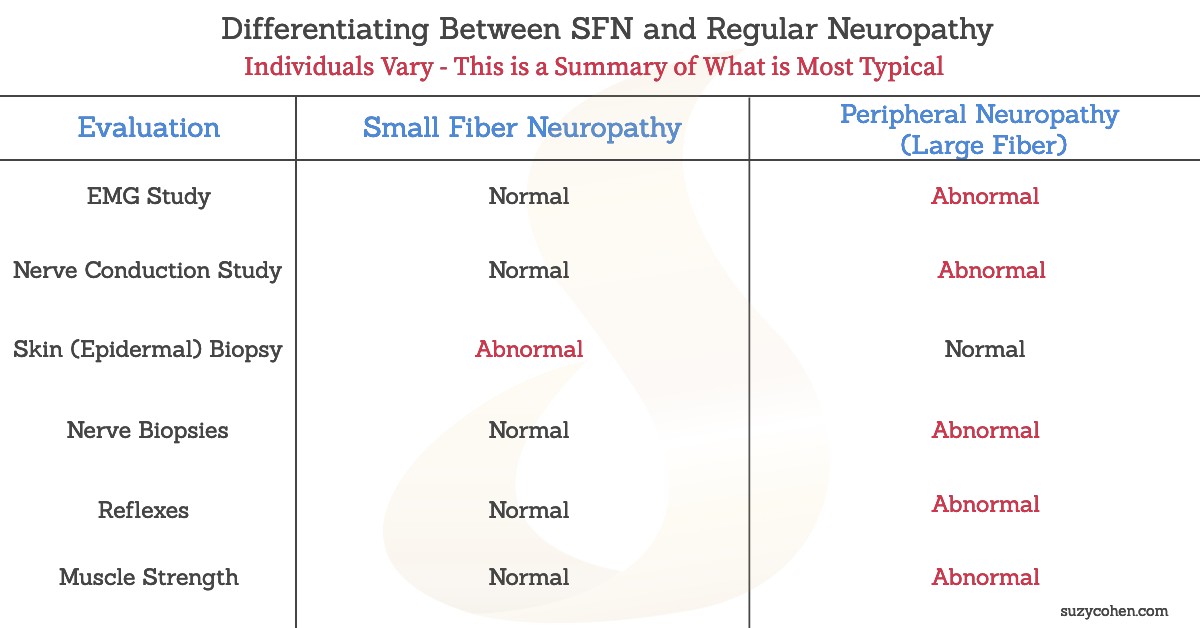
What about balance and strength?
People with regular peripheral neuropathy (PN), sometimes have issues with balance and coordination, as well as muscle weakness. With SFN, you will not see these problems because they’re only associated with LARGE nerve fibers, not the small C or A delta fibers.
Detection of Small fiber neuropathy is confirmed by doing a skin (epidermal) biopsy on several areas of your extremities (ankle, thigh, arm, etc). To test properly, two or three different areas on the extremities should be biopsied at the same time, for one test kit. See below about Therapath and Corinthian.
Medications that Cause Small Fiber Neuropathy
The condition of SFN has not been widely studied so not all of the causes are known right now. There are MANY causes for SFN, too many for me to list here. If you can find out the cause of it, you can at least work towards curing it, versus managing symptoms. It’s always better to cure than to medicate symptoms away. For example, you can ask your physician to switch you to a therapeutic equivalent drug that is safer if you are currently taking neurotoxic drugs like a STATIN, colchicine, nitrofurantoin for bladder infections, quinolone antibiotics (which should NEVER be used in people with diabetes).
Another example is if you’re unknowingly mega-dosing yourself on vitamin B6 (like royal jelly supplements rich in pyridoxine), you could stop that. You can control your blood sugar levels and heavy metal exposure. Certain things are within your control. You can control your cholesterol with diet and exercise if taking a statin is causing neuropathies. Here’s a STUDY showing that statins may be associated with non-length-dependent SFN confirmed by punch biopsy.
Alcoholism will cause nerve damage, as in SFN. With alcoholism, you might think it has to do with low B1, but no, the SFN is due to another mechanism. Hepatitis C infection and smoking are other causes for SFN.
What about chemo?
If you are currently undergoing treatment for cancer, you may want to ask your oncologist to use a different chemotherapy, one that does not affect the small fibers, or ask for a pre-treatment to protect you if you’re using some of the “taxane” drugs known to cause length-dependent SFN.
For those that have an unknown cause, you will be given the diagnosis of “Idiopathic Small Fiber Neuropathy” which is nonsense, it’s just saying “I don’t know” what’s causing this. You must keep searching or find another doctor who will search with you until you get an underlying cause. It makes sense right, you have to know what exactly to treat. I suspect you’ll find an autoimmune component.
Small Fiber Neuropathy could easily be termed “Autoimmune Neuropathy” just in case you research on your own.
Other causes of SFN are as follows:
Small Fiber Neuropathy: Causes
1. Endocrine or Blood Sugar Abnormalities.
We do know that peripheral neuropathy (and SFN) may be related to diabetes, pre-diabetes or other conditions that impair blood glucose metabolism. This is a very common cause for millions of people with neuropathic pain. Cancer and chemotherapy is another common cause for neuropathy.
2. Chronic Infections such as Lyme.
HIV is known to cause small fiber neuropathy. Another accepted cause for SFN is a post-Lyme disease, caused by a tick bite. This is a very dangerous situation because Lyme may go undetected and undiagnosed for years all the while causing symptoms of SFN. Undiagnosed Lyme is actually one possible cause of a child’s severe neuropathy.
Lyme is frequently caused by an unknown tick bite because a person does not feel the bite. What happens is, that ticks often come off the pet dog or pet cat, biting a person and you do not feel a thing because the tick numbs the skin before puncturing it, and dumping their infectious bacteria into the body.
Furthermore, the hallmark bullseye rash only occurs in 50% of people who are bitten. So the difficulty is that a person may have Lyme disease, and not know it, but the ensuing small fiber nerve damage causes painful sensations and SFN symptoms without an obvious cause.

only appears 50% of the time
When I hear a person has idiopathic neuropathy or idiopathic SFN, I begin to wonder if they have been properly tested for Lyme disease yet. The best way to test for tick-borne diseases is to do the complete panel plus co-infections. The best test is offered by Igenex Laboratories. FYI, some of their comprehensive panels run about $1,000 – 2,500.00. I’d say they’re worth it though. Other tests produce false negatives. Insurance may cover it.
If this specific connection is important to you, please refer to this STUDY published in PLoS ONE, that details the association between Lyme disease and SFN. In the study, 10 patients (5 men, 5 women) were evaluated and all were positive for Lyme infection. We don’t know if they had Bartonella or Babesia though.
After IVIg therapy, ALL of the patients (not some, ALL!) reported symptomatic improvement, and their skin biopsies were remeasured and they were significantly better. Dr. Katz concludes, “Patients who develop neuropathy after contracting Lyme disease or receiving the LYMErix vaccine, improve clinically and increase their ENFD after IVIg therapy.”
[ENFD = Epidermal Nerve Fiber Density]
Skin biopsies confirmed abnormal epidermal nerve fiber density (ENFD), and at least one skin biopsy was abnormal in ALL 10 participants. The researchers concluded that SFN may be responsible for certain sensory symptoms in patients who have had Lyme disease. Additionally, they concluded, “dysautonomia related to SFN and abnormal CBFv also seem to be linked to PTLDS.” What they’re saying is that if you have odd sensory and cognitive symptoms related to your sympathetic or parasympathetic nervous system, it could be tied to Lyme and might be related to decreased blood flow to your brain.
It confirms that Small fiber neuropathy can affect the brain, something that is important but not well known. Most physicians still think that neuropathies are limited to skin sensations. Another ground-breaking 2009 STUDY led by Amiram Katz, MD, a world-renowned neurologist from Connecticut (USA) who specializes in Small Fiber Neuropathy and Lyme disease was conducted. His research study is of tremendous importance to Lyme disease patients because that infection unfortunately turns into an autoimmune disease, and this is not widely known in the community.
According to Dr. Katz, “Small fiber neuropathy can be easily diagnosed by counting nerve fibers in a skin biopsy and many times represents the outcome of a multisystemic autoimmune process.”
He and Dr. JM Berkley enrolled their patients, and administered IVIg to these patients with Lyme disease. The participants all had small fiber neuropathy complaints of varying degrees. The biopsies were taken from their ankles, then they were treated with IVIg for 6 to 12 months. All patients had antibodies to B. burgdorferi, the main infecting organism of Lyme.
3. Shingles.
Another infection that we are re-thinking is post-herpetic neuralgia, as in shingles. There is now data from a 2018 ARTICLE to suggest that persistent neuropathic pain from post shingles is caused by SFN. This is huge because the clinical basis for your pain or itch must be detected in order to treat you properly. Many people deal with shingles-related pain/itch and no one ever checks them for SFN!!! This is one condition where SFN is probably driving the pain. So I hope this information helps you. Remember, the small fibers will keep growing, and if infection is the cause here, then immune-regulating efforts will improve the situation.
4. Autoimmune Disorders.
Having an autoimmune disease will raise one’s risk for SFN. In fact, many times SFN goes hand in hand with autoimmune diseases. Sjogren’s disease is one very common cause for SFN, and has hallmark features of dry eyes and dry mouth. Sarcoidosis is associated with SFN. Celiac is also another possible cause for SNF. Rheumatoid arthritis is rarely reported in association with SFN, compared to Sjogren’s, however it is still possible.
Autoimmune disorders of any sort may go hand-in-hand with small fiber neuropathy. It’s seen with Guillain-Barré as well as chronic inflammatory demyelinating polyneuropathy (CIDP). One of my close friends can’t ever go to yoga with me because she has Ehlers Danlos Syndrome and says she’s apt to hurt herself. If you have that condition, you should know that Small fiber neuropathy is a common feature of it. Here’s the STUDY.
Complex Regional Pain Syndrome (CRPS) may also be a condition that goes on way too long, and it may be due to small fiber neuropathy damage. There may be an autoimmune component too.
5. Fibromyalgia.
The condition called “fibromyalgia” does not have one definitive cause, we just know that patients with this pain syndrome accompanied by all kinds of sensory and neurological complications which vary from day to day. I wonder how many fibromyalgia patients actually have SFN based upon infection!
According to this STUDY symptoms of SFN showed up in about 40% of fibromyalgia patients. Not all patients with fibro have symptoms of SFN but a substantial portion of fibromyalgia patients have SFN. If I were a fibromyalgia patient that had these sensory changes, I would absolutely do the biopsy test for SFN. I would search for a root cause. I wouldn’t be happy with a descriptive name for my condition, I would want to at least test for SFN to see if that was the root cause. I’d also test for Lyme. Remember, small fiber neuropathy is definitely treatable, but the prognosis is better if you know what the underlying cause is.
Here’s another STUDY regarding fibromyalgia patients whose eyes were evaluated.
6. SSRI Use or Withdrawal.
Interesting and hard to explain, but people who are taking, or even weaning off SSRI antidepressants (in withdrawal) report areas of skin numbness, or altered sensations on their back, chest or abdomen. Sometimes the whole body is affected. I’m going to hypothesize that benzodiazepine withdrawal can trigger feelings of SFN as well. In time, my studies will back me.
7. Sodium Channel Mutations.
It’s not common in the US, however, in Europe, mutations in the sodium channels contribute to the neurodegeneration of small fibers. Some changes in the sodium channel also lead to seizure disorders. The sodium channel gene SNPs may occur in SCN9A or SCN10A (and others).
8. Hypothyroidism.
Many people with low thyroid experience sensory changes in the skin and temperature regulation difficulties (usually feeling cold). Other symptoms could be attributed to SFN, so thyroid problems including Hashimoto’s thyroiditis may be another cause for SFN.
I will cover this more extensively in a future article because if you have subclinical hypothyroidism, you can still have nerve problems. That’s very important. You can read this one STUDY and another STUDY.
You can also use my search box, I have written extensively on hypothyrodism and Hashimoto’s and other thyroid-related symptoms.
9. Vaccination or Long Covid.
You might be interested in this ARTICLE published in May 2022 in the journal, Neurology. It’s about long-covid and small fiber neuropathy. There’s a relatively new peer-reviewed PAPER published in June 2022 regarding a case and you can read about that if you’re interested.
Small Fiber Neuropathy: The Treatment
Treatment for Small fiber neuropathy varies and is based upon the underlying cause. The length of treatment will likely be life-long. There are ways to manage SFN, and stop some of the sensations, and many people do feel a significant recovery if they can find out what is damaging their small fibers. Remember, they grow back! So as disabled as you may feel right now, it is possible to reverse the damage and get better.
This is a great time to enlighten you to the work of Dr. Anne Louise Oaklander who made an enlightening VIDEO about SFN. Dr Oaklander calls it “Small Fibers, Big Pain” and one of the most interesting statements she makes is, “Small fiber neuropathy can actually affect the brain.” She is an amazing world-renowned expert in this field and if you think you have Small fiber neuropathy, take a look at her WEBSITE for more information.
Most people don’t think of neuropathy as a brain problem, but it definitely can be!
1. IVIg Intravenous Immunoglobulins.
There is EVIDENCE to show that IVIg (also written as IVIg) is very useful for small fiber neuropathy. After 3 months of IVIg (using a dose of 2grams/kg every 4 weeks that was titrated), 74% of patients reported improvement. There was a 15% remission rate too! Pain levels decreased and most of the adverse events were expected and mild.
That is good news! Having IVIg as a treatment is important if you have a serious case, however getting IVIg covered by insurance is a challenge because it’s very $$$$$$, and clinics that administer it are not available in all parts of the country. Still, it is my #1 suggestion for people with SFN because it is known to help especially if the Small fiber neuropathy stems from immune system-related conditions or infections. Autoimmune disorders that cause SFN will usually respond to IVIg.
Although IVIg is a blood product (which raises many questions because it’s made from healthy blood donors -thousands of donors per batch- I think it’s a good starting point. There is available some SCIG (subcutaneous IG) which is basically pooled human antibodies but it’s given SQ. Whether you get it IV through an infusion, or subcutaneous is up to your treating doctor, and what your insurance will allow. IVIg is currently the gold standard despite the fact that it is a blood product and can even cause blood clots. Incidentally, IVIg is being used in the treatment of COVID-19.
IVIg is FDA approved for various conditions such as immune-mediated peripheral nerve disorders, Guillain-Barre syndrome, chronic inflammatory demyelinating polyneuropathy (CIDP), and multifocal motor neuropathy. These conditions cause dysautonomia, which affect small fibers. If you’re interested in a learning more about SFN and dysautonomia, I can point you to a good video by Dr. Amanda Peltier. Here’s the LINK.
IVIg isn’t approved for SFN specifically, but it is the treatment of choice for individuals with this SFN. There are many potential, risky side effects for people receiving infusions of IVIg, however the most common ones include headache, flu-like symptoms, GI distress, nausea and/or fatigue. Staying well hydrated prior to your infusion will help reduce these. Taking a baby aspirin or an antihistamine could also be useful on the day of the infusion.
There was a STUDY that enrolled 55 patients with biopsy-confirmed SFN. The treatment duration of IVIg lasted several years in some cases, and improvements were seen. Most of the patients in this study had autoimmune conditions, or biomarkers that were suggestive of past autoimmunity. The doctors concluded that there was “real-world, proof-of-concept evidence suggesting that IVIg is safe and effective” for the right candidate, especially those with an autoimmune component. The study is entitled, IVIg for Apparently Autoimmune Small-fiber Polyneuropathy: First Analysis of Efficacy and Safety.
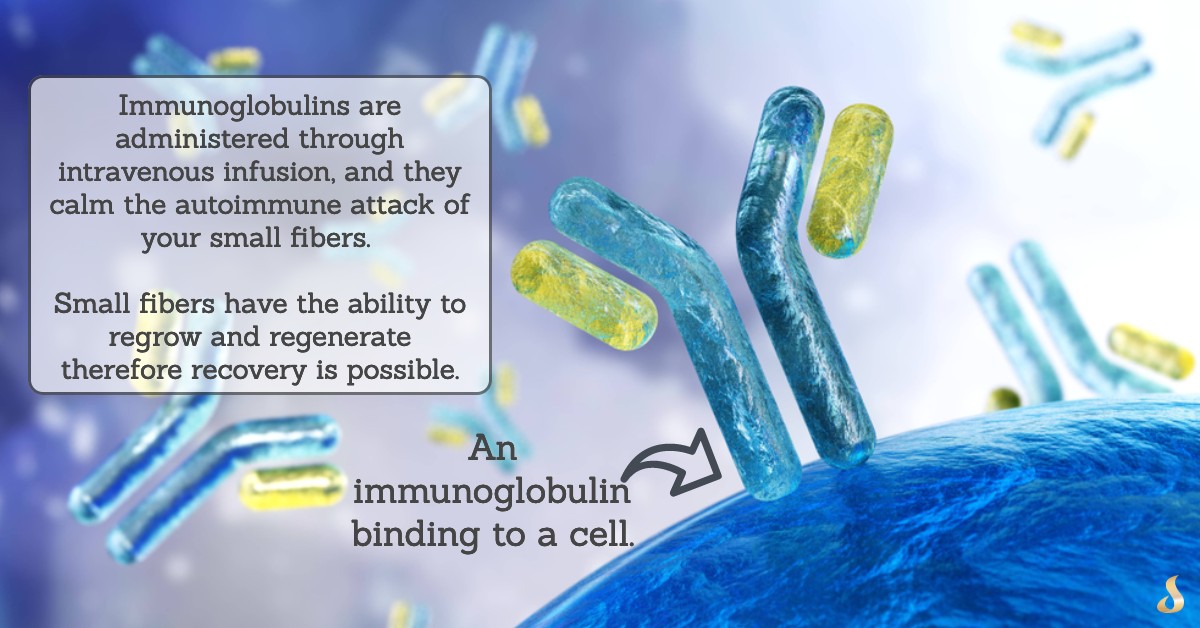
Insurance companies don’t like to reimburse for IVIg treatment because it is rather expensive (I believe 300 – 500 thousand dollars annually), so you can imagine how many appeals you’ll have to have with your insurance company in order to garner reimbursement. Doctors who work in this field already understand this and will go to bat for you. They often have a designated person that works closely with insurance companies and they know how to get a patient qualified. Of course, you MUST have one of qualifying conditions to receive coverage for it, but I’m saying it might take a few phone calls and labs!
2. ARA 290 a.k.a. Cibinetide
This is a small peptide that is available online at Peptide Sciences, however they only sell it for research use, as it is not intended for human or vet use. So if you buy it, you must click on a box, to “agree” to their terms (to use it only for research). It requires bacteriostatic water to reconstitute it prior to injection because it comes as a powder.
According to the research done on this compound, I think it could be extremely useful, and in a short amount of time. The common dose is given SubQ (subcutaneously) as 4 mg every day for 28 days. It’s a 28-day course. It has been studied in humans of course, for many years, and it has powerful benefits to regrowing the small fibers, but again, the FDA has come down on injectable peptides lately, hence all the restrictions. In studies, even in those on humans (which are available on PubMed), this remarkable peptide has been extraordinarily helpful and free of any dangerous side effects as far as I can tell with the 4mg daily dose.
There is a PAPER published on this website for Araim Pharmaceuticals that explains more about the human study using this novel peptide that they named cibinetide (because it’s a drug in their eyes, but it also goes by ARA 290. In an interesting VIDEO, Dr. Daniel Culver explains the benefits of ARA 290 for people with sarcoidosis who commonly also have small fiber neuropathy. I really enjoyed his talk, and suggest you watch it if you have small fiber neuropathy because he talks about other treatments too.
Here’s a STUDY that looked at the cornea which correlates with small fiber status in the body and ARA 290: Cibinetide Improves Corneal Nerve Fiber Abundance in Patients With Sarcoidosis-Associated Small Nerve Fiber Loss and Neuropathy Pain.
3. Blood Sugar Management.
If your SFN is related to your diabetes, then controlling blood sugar and weight will be helpful. Improving insulin sensitivity will help too. Exercising to your abilities will also be helpful. If your blood sugar and insulin levels are normal, and you do not have any endocrine dysfunction, then there’s nothing you need to do here. CLICK HERE if you are interested in learning more about my own formulation called GlucoScript.
4. The Medications.
The actual paresthesias and symptoms of SFN can sometimes be treated with gabapentin (Neurontin®), or with pregabalin (Lyrica®). These may cause drowsiness and weight gain, as well as potentially irreversible tinnitus. They are both anti-seizure prescription medications known to help with SFN and other neuropathies.
The use of certain antidepressants may be of value if their side effects are tolerable. Cymbalta is one prescription option, but it may not be well tolerated. This is because Cymbalta (and similar medications in this category) cause hypertension by raising levels of norepinephrine. This may feel fine to some patients, whereas others find that intolerable and uncomfortable. So some of you can try this if your doctor approves, however it may not be right for you.
Medications like Tylenol with Codeine #2 or #3 could be helpful if used for a short period of time, but they are not that useful long-term. Opiates do not repair the damage of the small fibers and do not help as much as steroids.
Corticosteroids (dexamethasone, prednisone, hydrocortisone) are steroids, and these are another category of potentially effective prescription medications that help patients with small fiber neuropathy (especially if is autoimmune-driven).
Steroids slow down the attack on your self. These types of medication need to be taken in the morning because they can interfere with sleep.
These have psychiatric side effects like agitation, rage, psychosis, and other bizarre brain-related side effects which may limit their use.
Further limiting their use is the immunosuppression that occurs and during a pandemic, it may not be ideal to begin therapy right about now. That said, DO NOT STOP them if you’ve been on them because doing so could be harmful.
5. Light Therapy.
I am uncertain about this therapeutic option for Small Fiber Neuropathy, however, it could be useful for regular PN. I’ve read about the benefits from light therapy, and have seen people claiming that light therapy, specifically near-infrared lights were helpful at relieving some of their pain. I’m listing it here in case you want to follow up with a light-therapy professional or research it on your own.
6. Physical Activity.
I’m listing this as a possibility for those of you in the early, mild stages of Small fiber neuropathy. But for those of you who are suffering greatly, you already know that practically any form of exercise or physical strain may exacerbate your symptoms. Even easy housekeeping chores could set a person back if they have severe Small fiber neuropathy!
The benefits of physical activity are that it improves blood circulation and increases the flow of oxygen to nerves and to the brain, so it is important, but again, do not push yourself if being sedentary is most comfortable for you.
Small Fiber Neuropathy: Testing
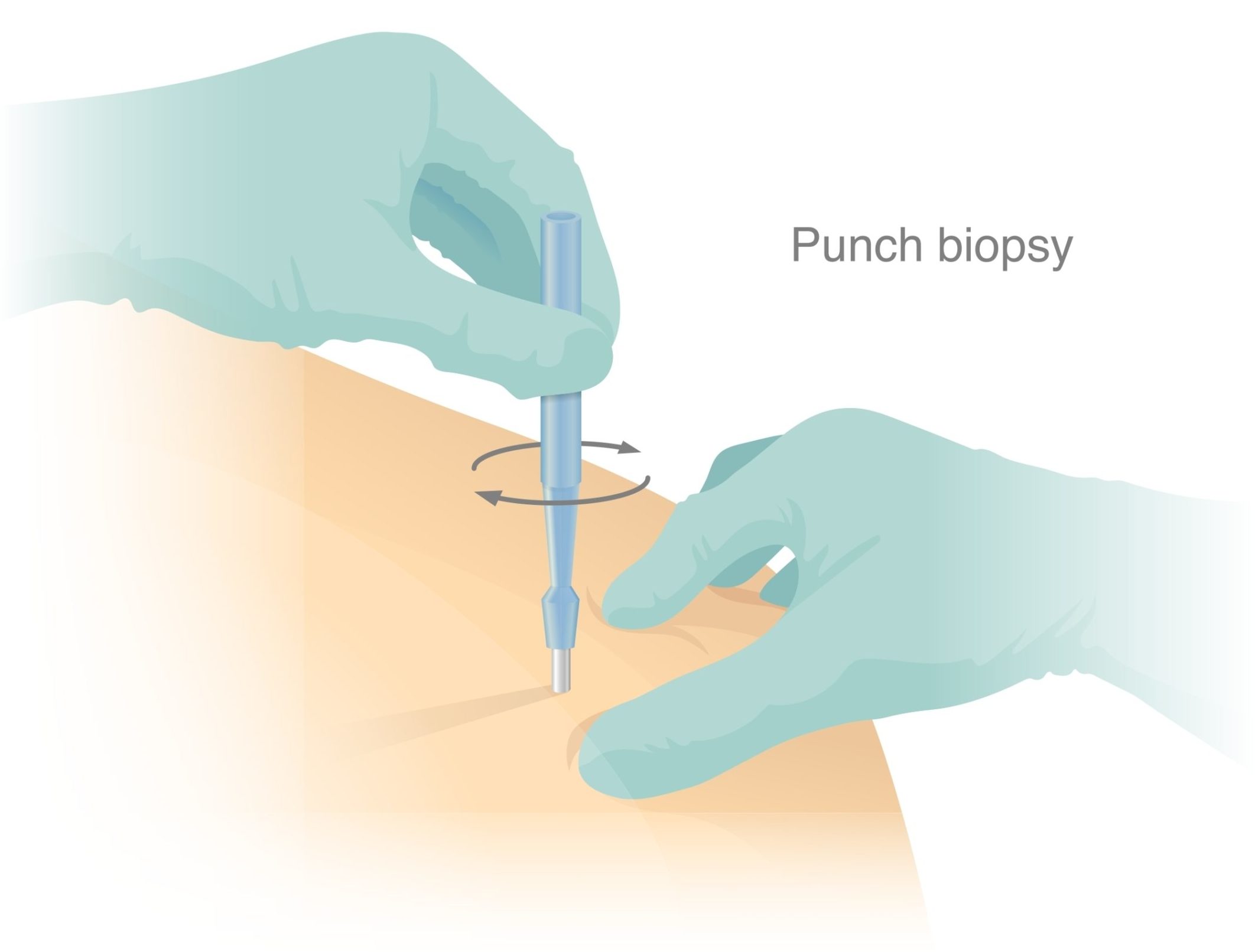
The good news is that Small Fiber Neuropathy is relatively easy to test for. It does not require invasive scopes, anesthesia, a trip to the hospital, or any kind of expensive imaging! It requires 2 or 3 small skin punctures (biopsies), and it takes just a few minutes for someone to perform the test on you. Then you just have to wait patiently for your results, which could take a few more weeks.
The objective evidence of a biopsy test for Small fiber neuropathy really takes the guesswork out of diagnosing a patient with odd symptoms. An accurate diagnosis of the underlying cause of plaguing problems is key to you ultimately getting well.
I am not a Provider for Therapath or Corinthian (see below), so you must go through a Medical Doctor to get these, preferably your neurologist who understands Small fiber neuropathy or a neurologist specializing in neuromuscular disorders. (The labs will allow PAs and Nurse Practitioners to order from them as well).
Once ordered, the test kit is mailed to your practitioner, but you will also need a qualified practitioner who is capable of doing the skin biopsy for you. They will numb your skin first with lidocaine, then take a 3mm circle (puncture) of skin off you, then cover it with a bandage. Sometimes 1 stitch is needed, sometimes not, it depends on what they want to do. There’s a video link below that you can watch in the Therapath section.
Getting this test done PROPERLY sounds pretty easy, but it’s really not depending on where you live and how knowledgeable your doctor is because the test is dependent on them taking the 3mm skin fibers off the right location on your body. If the biopsy isn’t taken from the correct part of your leg (or arm), it may not be accurate.
If it’s taken too early in the course of the disease, it may show up as “normal” even though you have many symptoms. You might have to do the test again the following year as your symptoms progress. Testing your progress is important, but I would only suggest you do the test once per year.
Be patient, and persistent about finding a competent team of practitioners to help you complete the test properly.
Patients CANNOT order the following tests, only these practitioners:
1. Medical doctors (Internists, Neurologists, Dermatologists)
2. Nurse Practitioners
3. Physician’s Assistants
Ultimately, you are seeking a neurologist that understands exactly what Small Fiber Neuropathy is.
This is what you need to get well and get tested properly. Here are the tests:
1. Therapath Small Fiber Neuropathy Testing
This lab is a leader, they are excellent if you would like to test for Small fiber neuropathy. They have a convenient test kit, and they’ve been around for years. Therapath provides these skin biopsy tests, also referred to as Epidermal Nerve Fiber Density (ENFD) tests. Whatever you want to name it, it is a test for Small fiber neuropathy. Therapath also has a test kit for sweat gland nerve fiber testing, which is useful for cystic fibrosis. Results by Therapath are processed quickly, in about one to two weeks.
The Therapath test kit comes with lidocaine, and everything you need. It’s mailed to your doctor. Two or three specimens (each 3mm) will be taken from various sites on your body. The physician will put the specimens into the kit which comes with a pre-paid label to send back. Be sure that the frozen ice pack goes inside the kit as instructed.
Here’s a VIDEO made by Therapath that you can watch. This shows you the exact procedure and how the skin puncture is done. Warning – they are extracting a piece of skin in this.
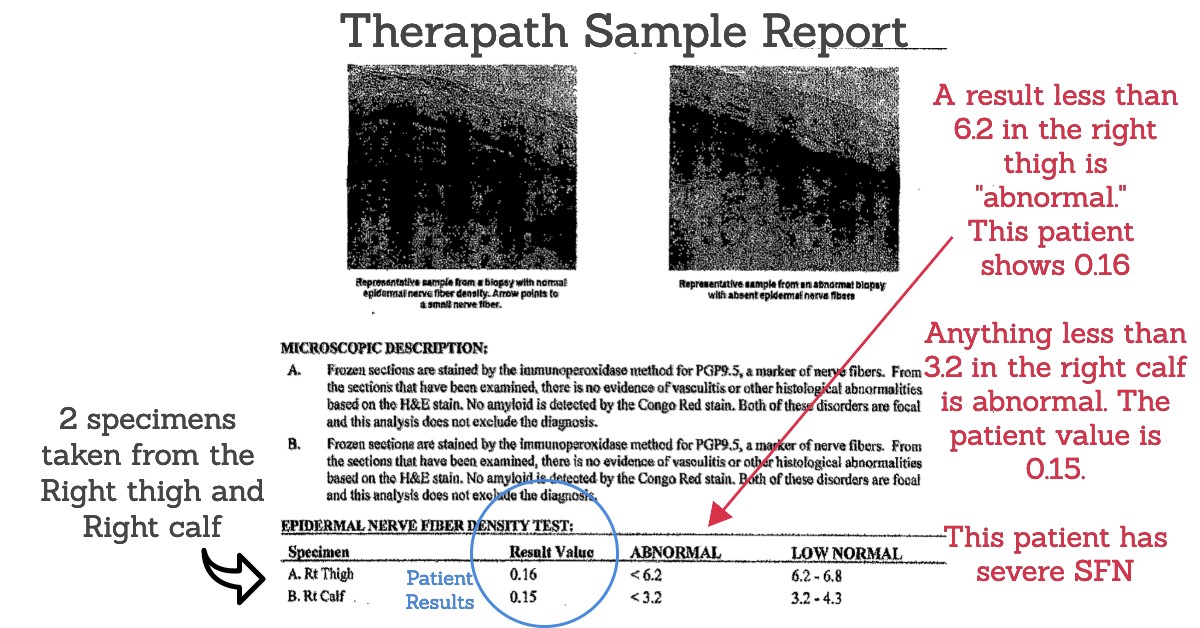
Here’s a graphic I made for you using a patient’s data from the Therapath Small Fiber test. As you can see from the test result, two specimens were obtained and tested (right thigh and right calf biopsy). This patient has skin biopsy-confirmed Small fiber neuropathy that is severe and long-standing since the results are virtually zero.
Therapath Labs
Address 545 West 45th Street, New York, New York 10036
Phone 800.681.4338
Fax 917.441.1116
Email clientservices@therapath.com
2. Corinthian Reference Labs
Corinthian is another commercial diagnostic laboratory specializing in neurological disease detection, and they specialize exclusively in testing skin biopsies, and also sending a kit to your physician. I like this lab too, but I don’t have a graphic of a sample test to show you like the one above. Their site has a lot of information including this great ARTICLE written by two physicians: David S. Saperstein, MD, and Todd D. Levine, MD.
Ordering kits from them is easy, and convenient.
Corinthian Labs – Phone: 855-CRL-LABS (855-275-5227).
3. Dr. Oaklander’s Site.
It’s possible that you can have a test done at Massachusetts General Hospital, or to have Dr. Oaklander, a leader in the field give you a second opinion regarding a test you’ve already done. Here’s the LINK to learn more about these other options.
4. Corneal Microscopy Imaging of Sub-basal Layer.
This eye test isn’t available for consumers, it’s a research test right now, but it has a lot of merits and I like that it’s not invasive. No punctures needed! I suspect it will become an option for testing in years to come. Ophthalmologists always look into the eye using their special keratometer and other ‘microscope’ tools, and they can actually see the nerve fibers in there (without having to take a chunk of skin out you)! So this eye test might is a great way to check for small fiber neuropathy. Here’s a LINK to learn more.
Other Tests that Physicians Can Order to Uncover Small Fiber Neuropathy.
In addition to the specialty labs above that test for Small Fiber Neuropathy, there are tests here that I want to mention that could be important to your building the case to appeal to your insurance.
At the end of the day, if you want IVIg, the best treatment in my humble opinion, then you will need to have some more lab tests in your back pocket to build the picture of inflammation and/or autoimmunity. More specifically, if you have an autoimmune disease such as “autoimmune encephalopathy” for example, your odds go up for qualifying for the IVIg.
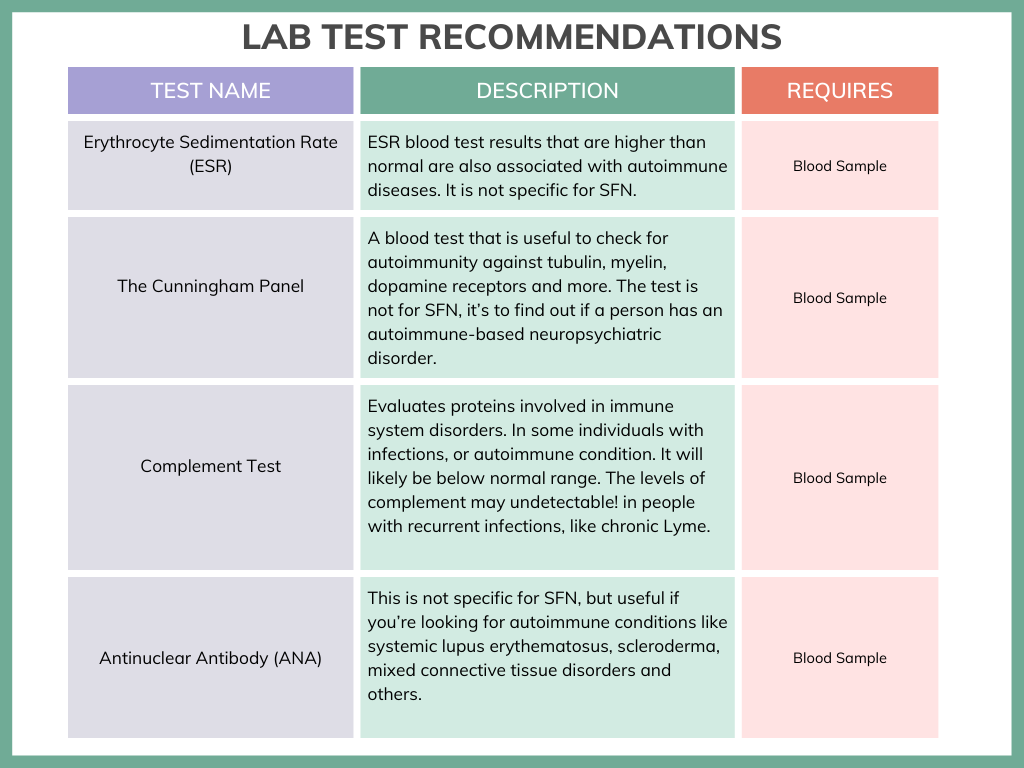
Follow the link to know more about The Cunningham Panel.
There are many other miscellaneous tests a physician can order. For example, today we can test for antibodies to the adrenergic and muscarinic receptors, ion channels, NMDA receptors, or ganglionic acetylcholine receptors. There may be antibodies against the N-type or P/Q type calcium channels (look up Lambert Eaton), and more. It is beyond the scope of this article.
Some of these blood tests I’ve mentioned just now can be evaluated using the Mayo Clinic or Cyrex Labs (Cyrex Array 12 Pathogen-Associated Immune Reactivity Screen). If you have an autoimmune condition, along with symptoms of small fiber neuropathy, there’s a good chance you’ll get your insurance company to cover the IVIg. There’s more about this HERE in an article entitled, How We Treat Autoimmune Small Fiber Polyneuropathy with Immunoglobulin Therapy.
In closing, many of you who suffer from mysterious symptoms may find help today, and hope.
Having an actual name for what you have gives you peace of mind. I’m assuming that many of you with these mystifying symptoms have been misdiagnosed repeatedly. Perhaps your diagnosis has kept changing, but your symptoms remained the same. Small fiber neuropathy is NOT just a skin sensory problem with plaguing neuropathy-like paresthesias. If left untreated the small fibers of your organs become affected, making it a progressive condition.
The good news is that it is treatable because those small fibers regenerate. So finding out if you have it is the key to getting proper treatment. I’ve worked very hard on this article and sincerely hope it has helped enlighten you. If you have any comments you’d like to share with me, or any tips for dealing with Small fiber neuropathy, or with insurance companies, please feel free to email me at scriptessentials@gmail.com
Related articles you may be interested in:
Strange Causes for Seizure Disorders
7 Common but Strange Reasons for Insomnia
Snatiation and 7 Facts about Sneezing

Suzy Cohen, has been a licensed pharmacist for over 30 years and believes the best approach to chronic illness is a combination of natural medicine and conventional. She founded her own dietary supplement company specializing in custom-formulas, some of which have patents. With a special focus on functional medicine, thyroid health and drug nutrient depletion, Suzy is the author of several related books including Thyroid Healthy, Drug Muggers, Diabetes Without Drugs, and a nationally syndicated column.