What's On This Page?
ToggleIn the realm of endocrine disorders, a thyroid nodule or multiple nodules present a significant diagnostic challenge for healthcare professionals. Recent research spearheaded by the University of Colorado School of Medicine has illuminated a promising path forward! Let’s talk about that now. Part of the beauty of this study is that fewer needles will be needed!
Imagine you have a small lump or bump in your neck, and you’re not sure if it’s something harmless or something serious like cancer. This is similar to finding a thyroid nodule, which is just a fancy term for a lump in the thyroid gland located in your neck.

Is it a Goiter or a Nodule?
A goiter may present as a diffuse enlargement, characterized by a smooth and uniform increase in size across the thyroid gland. Alternatively, it can manifest as a nodular goiter, which is characterized by the presence of one or more nodules within the gland itself. These thyroid nodules vary in composition; they can be entirely solid, completely filled with fluid, or have a mixed consistency, containing both solid and fluid components. The occurrence of thyroid nodules is relatively common in clinical practice.
Evaluating the Thyroid Nodule?
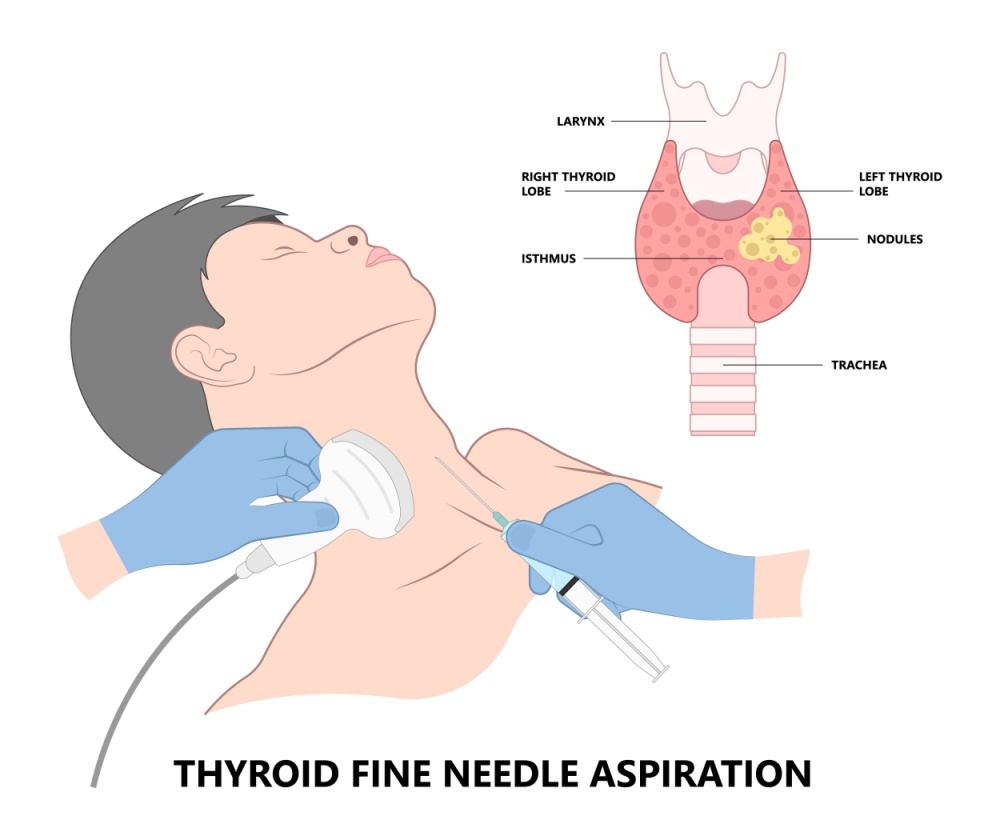
Now, doctors want to figure out if this lump is something to worry about (cancerous) or not (benign). Doctors will take your medical history, look at your THYROID LAB RESULTS, and almost always do a simple non-invasive ultrasound. If they still can’t figure out what this nodule is, the next step is a biopsy. This biopsy method is called a fine-needle aspiration (FNA) biopsy. Perhaps you’ve had an FNA already, or you’ve scheduled one for your follow-up.
It’s the standard of practice to do a biopsy, and they must use a needle. The exact way to do a nodule biopsy is by inserting a thin needle into your neck to take a tiny sample of tissue from the lump in there.
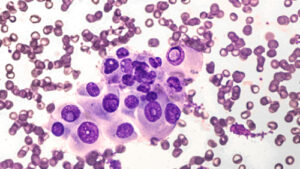
That way they can look at these cells more closely with a microscope to determine if they’re malignant or benign.
It may not stop with a biopsy. Sometimes, the physicians even have to do surgery just to make sure of what they’re looking at. But here’s the catch: these procedures can be stressful, costly, and sometimes, they turn out to be unnecessary because the lump was harmless all along!
So, what if we could avoid all this trouble for a lot of people? That’s where the researchers at the University of Colorado come in. They did a little study!
Study Overview
The 2023 STUDY, funded by the National Institutes of Health, aims to leverage your genetic data to develop what’s called a Polygenic Risk Score (abbreviated as PRS). This approach will enhance the precision of thyroid cancer diagnoses, reducing the reliance on all these needles! It will also help differentiate thyroid cancer from benign nodules (ie adenomatoid nodules the medical term for hyperplasia).
So using a fine-needle aspiration (FNA) biopsy (and surgeries) may become a thing of the past – or at least may be minimized and that would be incredible!
Thyroid Nodule: The Symptoms
Individuals with a thyroid nodule, or multiple nodules may experience a range of symptoms, including palpable lumps in the neck, changes in voice, difficulty swallowing, and unexplained weight fluctuations. These symptoms often prompt further medical evaluation to determine the nature of the nodule.
Symptoms you may have noticed:
Anxiety or feelings of nervousness
Challenges in swallowing
Changes in voice, including hoarseness
Cold sensitivity
Dryness of the skin
Edema, particularly noticeable as facial swelling
Exhaustion or fatigue
Fast, or irregular heart rate
Noticeable swelling in the neck, known as a goiter
Pain located in the neck
Unexplained weight fluctuations, including both weight gain and sudden, significant weight loss
Many thyroid nodules remain symptomless until they grow large enough to impact adjacent tissues and organs or become noticeable on the neck. The manifestation of symptoms can vary based on the nodule’s nature and origin. Sometimes an iodine deficiency causes these, but not always.

7 Key Steps in the Diagnosis of Thyroid Nodules
Understanding thyroid nodules and their potential implications can be crucial. Here’s a concise list of how a typical diagnosis is made, although every doctor has their own way. The reason they have to test these nodules is because they are concerned they may NOT be benign, but potentially cancerous. Thyroid cancer is highly treatable! There are four types and most are of the papillary form.
- Initial Consultation and History Taking: This first step involves a detailed discussion of your symptoms, medical history, and any family history of thyroid issues with your physician.
- Physical Examination: The doctor will palpate your neck to feel for lumps or enlargements in the thyroid gland.
- Blood Tests: These tests help to assess thyroid function and look for markers that indicate how the thyroid is performing. They will usually check T3, T4, TSH, antibody levels and sometimes iodine. Use my search box to learn more about these specific tests.
- Ultrasound of the Neck: A non-invasive procedure that provides a clear image of the thyroid and any nodules present.
- Fine Needle Aspiration (FNA) Biopsy: If nodules are detected, an FNA biopsy may be conducted to determine if the nodules are benign or malignant. A biopsy is almost always done.
- Additional Imaging Tests: In some cases, additional scans like CT or MRI may be required to further assess the nodule.
- Genetic Testing and Polygenic Risk Score (PRS) Analysis: Emerging technologies like PRS can offer insights into your genetic risk factors for thyroid cancer, potentially reducing the need for invasive procedures.
Types of Thyroid Cancer
-
- Papillary Thyroid Cancer: The most prevalent form, accounting for approximately 80% of cases. It generally has a favorable prognosis and is often detected early.
- Follicular Thyroid Cancer: Represents about 10% to 15% of cases. This type can spread to the lungs and bones and requires thorough evaluation and treatment.
- Medullary Thyroid Cancer: Comprises 2% to 4% of cases. It is unique because it often involves genetic mutations that can be inherited, necessitating genetic counseling for patients and their families.
- Anaplastic Thyroid Cancer: Although rare, accounting for less than 2% of thyroid cancer cases, it is highly aggressive and often resistant to standard treatments.
Significance of the Research
This groundbreaking study utilizes international biobanks to construct a comprehensive dataset, enabling the development of a PRS. This score is anticipated to better quantify the risk of thyroid cancer in individuals with thyroid nodules, based on a constellation of genetic factors rather than a single genetic mutation. The approach acknowledges the complexity of thyroid cancer risk, which is influenced by multiple genes interacting with each other and the environment.
The research team’s use of genome-wide association studies meta-analysis aims to pinpoint genetic associations directly related to thyroid cancer, distinguishing them from traits associated with benign nodules and other thyroid conditions such as goiter.
Impact on Clinical Practice
The successful implementation of a polygenic risk score in clinical settings could significantly transform the management of thyroid nodules and many other disorders. See below for what else they will use a PRS for in the coming months to years.
By integrating genetic risk assessment with current diagnostic tools, such as ultrasound imaging, healthcare providers may be able to more accurately determine which nodules are likely benign and which warrant further intervention.
This precision in diagnosis is expected to decrease the number of unnecessary FNA biopsies and surgeries, reducing patient anxiety, the risk of surgical complications, and healthcare costs. Moreover, it lays the foundation for a more personalized approach to thyroid nodule management, aligning with broader trends toward precision medicine.
Polygenic risk scores (PRS) are not limited to thyroid nodules or thyroid-related disorders; they have a broad application across many diseases and conditions. A PRS is a tool used in genetics to estimate an individual’s predisposition to a certain disease based on the presence of multiple genetic variants. This approach acknowledges that most diseases are influenced by many genes, each contributing a small amount to the overall risk.
PRS is Being Explored for Other Diseases
Cardiovascular Diseases: PRS can help predict the risk of conditions such as coronary artery disease, atrial fibrillation, and hyperlipidemia. It can guide early interventions or lifestyle modifications to mitigate risk.
Cancer: Beyond thyroid cancer, PRS are being developed for breast cancer, prostate cancer, colorectal cancer, and more. These scores can inform screening strategies and, in some cases, influence treatment decisions.
Neurological Disorders: PRS have potential applications in predicting the risk of developing conditions such as Alzheimer’s disease, Parkinson’s disease, and multiple sclerosis. They could be used to identify individuals at higher risk for early interventions.
Psychiatric Conditions: Disorders like schizophrenia, bipolar disorder, and depression have also been subjects of PRS research. These scores may one day help in understanding the risk and potentially guiding treatment choices. If you are interested in mental health conditions such as misophonia – the term for people who don’t like to hear certain sounds (like chewing food or breathing), read my article, When Noise Triggers Rage.
Autoimmune Diseases: Conditions like type 1 diabetes, rheumatoid arthritis, and celiac disease have genetic components that PRS can help elucidate, potentially leading to better risk stratification and management.
Metabolic Disorders: PRS can predict the risk of developing Type 2 diabetes and obesity, among other metabolic conditions, which can be crucial for preventive health measures.
The use of PRS in clinical practice is still an area of active research and debate. I am sure we’ll get to a place soon where its usage is standard of practice (before the needles). One of the key challenges is the need for large, diverse datasets to develop and validate these scores across different populations, keeping all other variables stable.
Additionally, there’s an ongoing discussion about how best to incorporate PRS into clinical decision-making, considering the multifactorial nature of most diseases, which are influenced by many things other than your genes. For example, environmental factors, lifestyle, diet, prior medical history, and more.

While the potential of PRS is significant, its implementation in every clinic across the country is likely to not happen. I’d say it varies by condition and is dependent on ethical considerations –> because let’s face it, some people simply don’t care to know their genetic propensities, they won’t do a 23andme because it can be frightening to imagine your fate.
The odds are still in your favor. Also, people don’t want to submit themselves for a genetic test (rendering a PRS impossible) because they worry that their insurance carrier will drop them if certain disease propensities are revealed by the test.
That said, I still hold that it will be here soon, at least for thyroid nodule testing! You can learn more about Polygenic Risk Scores HERE.
Summary
The University of Colorado School of Medicine’s research represents a significant stride towards improving the diagnosis and treatment of thyroid cancer. Their goal it to use our genetic information (which is the stuff that makes you, you!) and minimize invasive diagnostic procedures.
So by looking at a bunch of different genes and how they interact, the researchers are developing a new way to assess a person’s risk of having thyroid cancer. This is done whenever they find a thyroid nodule on you. So having a PRS, will mean something and determine next steps!
The idea is pretty awesome because, with this score, doctors could look at your lump, consider your genetic risk, and then decide if you really need that needle biopsy or surgery! This would mean fewer unnecessary procedures, less stress, and saving money for up to 130,000 people every year in the United States.
In simpler terms, this study is all about finding a smarter, less invasive way to figure out if a thyroid lump is dangerous or not, using the power of genetic information. This could change how doctors deal with these lumps, making it less of a guessing game and more of a science, which is pretty cool for future patient care.
I am all about simple! I love tests that are easy and convenient. Since having a thyroid nodule, or multiple thyroid nodules is extremely common for people (almost always going under the radar due to their tiny size) this is wonderful news. This method is not available at the time of this writing (March 2024), but it will be very soon, probably by the end of this year, thus averting unnecessary medical interventions for so many of you who require continued monitoring with periodic FNAs.

Suzy Cohen, has been a licensed pharmacist for over 30 years and believes the best approach to chronic illness is a combination of natural medicine and conventional. She founded her own dietary supplement company specializing in custom-formulas, some of which have patents. With a special focus on functional medicine, thyroid health and drug nutrient depletion, Suzy is the author of several related books including Thyroid Healthy, Drug Muggers, Diabetes Without Drugs, and a nationally syndicated column.