What's On This Page?
ToggleD-dimer is a blood test that evaluates levels of a protein fragment when there’s a clot hanging around in the bloodstream. If this level is elevated, it’s often a tip-off that there was a tiny blood clot formed in your body and now you’re breaking it down. It is the formation of abnormal blood clots (thrombosis) that is the leading cause of heart attack and stroke and D-dimer is one way to evaluate your personal risk factor for this. It’s not the only way.
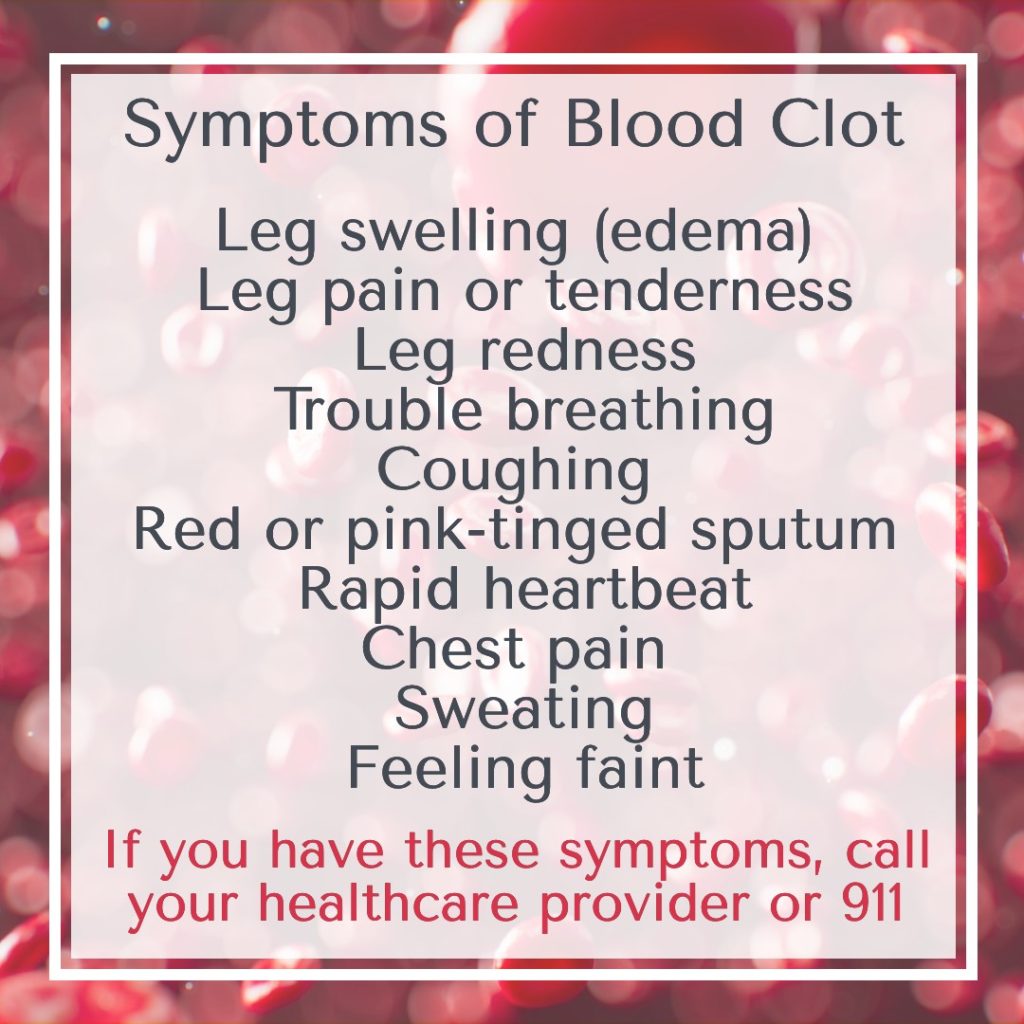
Now that people can self-order their own blood work at many places around town, you might want to evaluate your own D-dimer level. I must caution you that if it’s elevated, you need to alert your physician and find out if you need anticoagulant therapy, and what other measures you can be doing. Blood clots are dangerous so you don’t want to ignore an elevated D-dimer level.
In the hospital setting, a D-dimer blood test will be ordered if you have bronchitis or pneumonia in order to assess risk for respiratory failure, pulmonary embolism, stroke, deep vein thrombosis (DVT) and a number of other blood clotting disorders.
D-dimers are not normally present in our plasma except when the coagulation cascade has been activated (like when a blood clot has formed). Hence, you would expect the amount of D-dimer to be higher in people who have thrombosis. This explains why D-dimer levels are significantly higher in people with strokes, pulmonary embolism, heart attack or DVT.
There’s a correlation with higher mortality with C*V1D – !9 in people who have very high D-dimers, usually above 1,000 FEU. It is because microscopic clots restrict blood flow in the lungs, impairing oxygen exchange which leads to lung problems and breathing difficulty.
This is why a D-dimer should be evaluated in high risk patients who become infected with this respiratory illness. Elevated D-dimer is practically universal in all people who have C*V1D – !9 but that rarely means fatal complications! It’s just something to measure and watch closely if you have other comorbidities like heart disease, uncontrolled hypertension or diabetes, COPD, obesity and more.
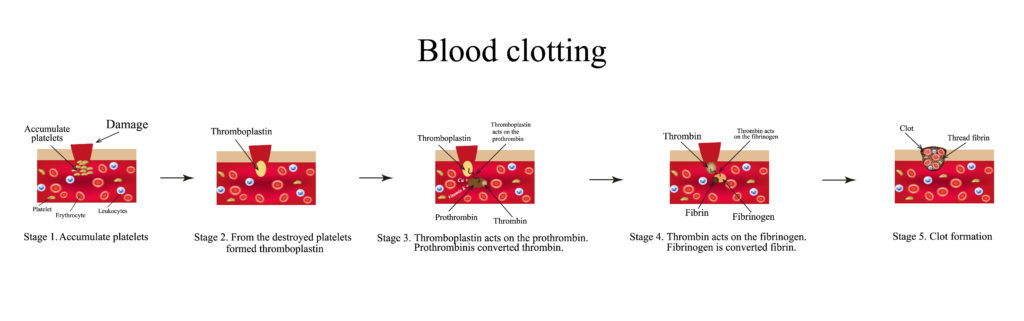
Since the D-dimer is an evaluation of clotting and a blood clot requires fibrin to form, you should think of natural, easy ways to protect your blood, keep it healthy, and keep your fibrin levels down in the normal range. In a moment, I’ll speak to that and offer suggestions.
Fibrin isn’t the bad guy. Fibrin is an insoluble protein formed from fibrinogen when your blood forms a clot. That’s okay and healthy because if you bleed from a paper cut, you want that to happen. The scab that forms is part of the normal hemostatic response.
Healthy fibrin levels means your blood moves through your vessels freely, and comfortably, without sticking to capillary walls and impeding blood flow. That’s important because a healthy fibrin level means that oxygen and nutrients get delivered to all your organs.
The relationship between D-dimer and fibrin and fibrinogen is noted HERE. But simply put, the D-dimer level represents the level of fragmentation of a clot formed from fibrin/fibrinogen.
Conditions Associated with Elevated D-Dimer
Viral or bacterial respiratory pathogens (active or in the past)
Recent surgery
Liver disease
Heart disease
Myocardial infarction
Kawasaki disease
Lupus (SLE)
Anti-neutrophil cytoplasmic antibody-associated vasculitis
Eosinophils granulomatosis
IgA vasculitis
Takayasu’s arteritis
Venous malformation
Pregnancy
Blood clots (see below for the graphic explaining how a clot is formed)
Disseminated Intravascular Coagulation (DIC)
Aortic dissection
Lyme disease because tickborne infections increase the hypercoagulability of blood.
Shortcomings of the D-dimer Test.
You can have a ‘false positive’ for lack of a better term in the sense that your D-dimer is borderline high, but you do NOT actually have a blood clot! And that can be very stressful to see a lab level that comes back high… so I see this as a shortcoming of the test. This is important because I never want to alarm a person.
So again, a ‘false positive’ is where the D-dimer is high (elevated) but there is no blood clot. You will often see this after surgery, or in pregnancy, in some cases of C*V1D – !9 long after they have healed; also in cases of liver disease and some types of cancer. When I say that the D-dimer can be “borderline high” I am referring to levels of 500 FEU, but lower than 1,000. See below for more details regarding reference ranges.
Another shortcoming is the non-specificity of the test. For example, if you do have a blood clot, and your D-dimer is elevated, it doesn’t tell you where the clot is! Is it in the leg vein, or the lungs as a pulmonary embolism, or where? The D-dimer does not provide that detail (it’s just a level). and it is an obvious limitation since a medical emergency is easier to head off if you know where the clot is in the body.
What Can You Do
Self treating a high D-dimer is not something you should be doing. Once your physician has evaluated your D-dimer, they may want to prescribe heparin, warfarin, clopidrogel or enoxaparin. This is a discussion to have with your doctor(s).
Statins which are traditionally used for high cholesterol have been proven to have anti-thrombotic properties and some of them like the lipophilic statins can lower D-dimer. These are sometimes prescribed for people with DVTs. You can read this ARTICLE which suggests 3 months use of statins can reduce D-dimer levels.
The D-dimer Test.
A normal predictive value is noted on your lab test. It can vary from lab to lab. For example, there are two ways to note D-dimer levels on a blood test:
1) Evaluate the DDU (D-dimer Unit) and it should be < 250 ng/ml
2) Evaluate the FEU (Fibrinogen Equivalent Units) and it should be < 500 ng/ml
So even though there are two different ways to note the levels of D-dimer, they are still measuring the same thing. They just have different cut-off ranges. So when you are told your number, look at the reference range on your own test to see where you fall.
For the sake of this discussion, let’s use the FEU range of 500 ng/ml or less.
If your D-dimer value is 722 for example, this is considered borderline and may not necessitate serious interventions. Anything between 500 and 999 is elevated, but not too serious. You can speak to your physician and try some dietary recommendations or supplements if she/he agrees. (See below).
DANGER: Once the D-dimer is higher than 1000 ng/ml that’s a problem! Your doctor should consider giving you some treatment to break down the clot faster that is somewhere in your body.
They know best about what is right for your individual case, but as a pharmacist I can certainly name the drugs that they could use, that are currently FDA approved to protect against blood clot diseases and stroke prophylaxis:
1. Low molecular weight heparin or LMWH
2. Enoxaparin SQ injection (Lovenox® or Clexane® often administered at home)
3. Apixaban (Eliquis®) Tablets
4. Rivaroxaban (Xarelto®) Tablets
5. Edoxaban (Savaysa®) Tablets
6. Dabigatran (Pradaxa®) Tablets
7. Warfarin (Coumadin®) Tablets
The purpose of these drugs is to reduce overall risk of stroke related to blood clots (or atrial fibrillation). See the graphic below for how a clot is formed.
Pradaxa (dabigatran), Xarelto (rivaroxaban), Eliquis (apixaban), and Savaysa (edoxaban). Like warfarin, all four of those newer drugs are “blood thinners” that reduce the overall risk of stroke, but if the dose is too high, they can also cause excessive bleeding and easy bruising. As a physician, dosing them properly is key. As a patient, taking them properly is critical.
Normally, the body maintains a delicate balance between clotting and dissolving clots, but certain illnesses, including thyroid disorders, can disrupt this balance. It’s mainly hyperthyroidism – if you have this condition, you will want to read my other article HERE.
10 Natural Strategies to Help Thin Blood
While I cannot offer advice for your personal medical condition, or even speak to what’s right for you, I can certainly talk about natural strategies to keep the blood thin and flowing smoothly. Let’s do that now.
1. Grape seed extract.
Among the most famous heart-loving and blood-thinning agents we have grapes! You have all heard that a glass of red wine is good for the heart. I don’t exactly believe that myself, nor do I advocate it, but the seeds of grapes do have merit. So at the top of my list is grape seed extract. These are edible and delicious.
There are supplements that offer a concentrated dose of the antioxidants that are known to support blood health and the entire cardiovascular system. Grape derived polyphenols lower LDL oxidation, and that’s good because it helps atherosclerosis. It has proteolytic activity and prolongs plasma clotting time and in short, I think it could help towards reducing D-dimer.
2. Bromelain.
The pineapple extract is like Pac-Man® and will digest proteins which is good because fibrin is a protein. It acts like a drug and inhibits platelet formation. Know what else does that? Aspirin… aspirin blocks platelet formation to some degree too.
Bromelain is an enzyme has important constituents like glucosidase, peroxidase, cellulase, escharase and other protease inhibitors. It’s a well-documented fact that bromelain has fibrinolytic activity, and is also anti-thrombotic. Amazingly, you can eat pineapple, or take supplements and all the goodness gets past your stomach acid!
This is why bromelain has so many post-surgical therapeutic benefits. It’s often prescribed by natural-minded physicians for bronchitis, sinusitis, wound debridement and various clotting and cardiovascular disorders. For more information, here’s a good ARTICLE.
3. Ginkgo biloba.
This herb comes from a beautiful tree and everyone knows it is a natural blood thinner! It’s often used to improve circulation of blood around the body, and to protect the brain by improving blood flow to that region. It blocks plaquing around the arteries and reduces risk of arterial clots. There have been studies on venous thrombosis and ginkgo supplementation led to improved vascular health.
Not only does ginkgo help support the vascular system and reduce risk of thrombosis, evidence suggests it may improve lipid ratios. Finding teas of ginkgo, and supplements are easy. Find this at any health food store and online.
4. Garlic.
If you’re not allergic to garlic, and you like it, use it as often as you can. There are also supplements of aged garlic made by Kyolic® brand that are odorless. While no medical claims can be made about supplements in the USA, I can talk about the food’s nutritional benefits here. Cooking with garlic may help lower thrombosis risk while also inhibiting the clumping of platelets.
Garlic reduces fibrinogen levels, and remember, that’s a good thing. Garlic will speed the breakdown of clots too. There are many compounds that are responsible for the anti-thrombotic properties of garlic, and one of them is called ajoene. Eating garlic should be okay with warfarin therapy, but of course do as your physician says.
5. Nattokinase.
Nattokinase is an enzyme, but we don’t make it. Found in a cheese-like food called natto, this is popular in Japan, South Korea and China. Of all the dietary supplements used for breaking down blood clots, nattokinase is probably the most studied. According to this ARTICLE published in 2017,

“Nattokinase (NK) can break down blood clots by directly hydrolyzing fibrin and plasmin substrate, converts endogenous prourokinase to urokinase (uPA), degrades PAI-1 (plasminogen activator inhibitor-1), and increases tissue plasminogen activator (t-PA) which supports fibrinolytic activity.
Unlike common fibrinolytic proteases, such as t-PA and uPA, which can produce various side effects such as bleeding, NK exhibits little to no side effects. Studies also indicate that an oral administration of NK can be absorbed by the intestinal tract. NK exhibits strong fibrinolytic activity after intraduodenal absorption. These characteristics make NK a versatile and potent fibrinolytic enzyme that can be used to combat blood clots.”
Put simply, nattokinase has well-documented anti-thrombolytic activity makes it a good adjunctive treatment for some people. Sold over-the-counter, nationwide in health food stores, ask your doctor if it’s right for you. You can eat natto as well. By the way, natto is produced by fermenting soybeans. After taking a pill of this, it may take 2 to 8 hours to even begin working.
Some experts worry about a theoretical problem where a clot dislodges. This is an interesting consideration, but it’s only theoretical. Nevertheless, I advise caution with this, and ALL supplements here. If you have an existing problem, such as DVT, you should be under physician’s care, and should NOT be self-treating with these supplements.
6. Lumbrokinase.
Lumbrokinase is the word that names an enzyme which comes from earthworms! After the obvious “eeew” factor, consider the medical (and potential life-saving) benefits. You’ve got to get out of your head when you take these capsules, because the clean, purified supplements like Boluoke® aren’t selling earthworms, they’re selling a clean, purified, proprietary standardized enzyme of lumbrokinase.
With some other brands (not all), you might be just getting earthworms. You just never know. So insist on high-quality brands, my favorite is Boluoke® because they are the leaders.
Boluoke® is a fully researched oral fibrinolytic supplement that publishes in vitro studies, animal studies, toxicity studies, and pharmacokinetic studies. According to the makers, Boluoke® does not affect INR or aPTT, thus is compatible with Coumadin® or heparin. There’s an interesting STUDY that you can read about regarding lumbrokinase in combination with LMWH (and subsequent warfarin), which should benefit.
Again, I like this brand name, I trust them. Their product works by reducing fibrinogen and fibrin, and it does not interfere with the natural coagulation cascade. It also contains 20mg lumbrokinase per capsule, and they verify that.
Finally, if you have a hypercoagulable blood condition (whether that’s from a respiratory illness, or from taking IVIg, take birth control pills, or other), this is a good product because it seeks to prevent clots. Infections as well as those medications I’ve just listed increasehypercoagulability of blood.
7. Water.
Does water lower D-dimer? No, it does not. But becoming dehydrated lowers blood volume, and this makes your blood ‘thicker’ raising your risk for blood clots if you are predisposed. So water is listed here as an important reminder to drink pure, filtered water each day. It doesn’t cost anything to drink a bit more and as a perk, it improves constipation, migraines and immunity. If your lips are cracked or dry, or your urine is potent and concentrated dark yellow or amber color, it’s a sign you’ve waited too long.
8. CoQ10 and Selenium.
This duo is interesting and was studied by researchers in Sweden. The paper was published in Nutrients 2021. The objective of the study was to find out how a combination of selenium and coenzyme Q10 would impact the D-dimer levels of people who had heart disease. D-dimer was measured in 213 individuals at the start and after 4 years of a well-designed double blind placebo-controlled trial, they found that it helped!
A significantly lower D-dimer concentration was seen in the group treated with these supplements. They used 200 mcg selenium and 200 mg CoQ10 which are both available nationwide. Ask your doctor if they’re right for you.
9. Green Tea or Matcha.
There are some studies that suggest green tea is as good as aspirin in terms of inhibiting clot formation, however, the compounds in green tea leaves work differently than aspirin, so the consensus is that you would continue to take your baby aspirin even if you drink green tea.
However, it should be noted that aspirin has some anti-thrombotic effects that differ from green tea, so if you are taking low-dose aspirin to prevent a heart attack or stroke, you should continue doing so even if you also drink green tea.
Compounds in green tea decrease levels of fibrinogen, a protein that helps clot blood. Green tea also prevents the oxidation of fatty acids, which can lead to thinner blood consistency.
10. Ginger.
Inhibits platelets from sticking together similar to aspirin. There are many studies, this is a well-documented effect of zingiber officinale (ginger). In September, 2019, this STUDY on rodents confirmed yet again, ginger’s pronounced anti-thrombotic effect on the blood. Here’s one of my other articles you will like, Why You Should Eat More Ginger. One other impressive benefit of ginger is its ability to help with coughs. I talked about that in my other article entitled, 9 Amazing Cough Suppressants to Shut You Up.
As a bonus, I’ll mention one more, CHAMOMILE. It’s easy to find supplements and teas of chamomile which is best known for its relaxation benefits. If you’d like to read how Chamomile acts as a platelet-inhibitor, CLICK HERE to read my article entitled, Chamomile Helps Arthritis, Blood Thinning and Oral Pain.
Also, I have a recipe for a sleep tea called Lavender Rose Tea, and this contains some chamomile in it. This is great to drink at night, and it has broad spectrum anti-microbial activity, blood-thinning benefits and immune-boosting properties.
In summary, the D-dimer test is one that can be self-ordered, or ordered by a physician in order to see if you may have a blood clot somewhere in your body. It’s seen after a blood clot has formed and is in the process of breaking down. An elevated D-dimer level is not a normal finding, but it doesn’t mean it’s serious either.
If you are having significant creation of blood clots in your body, your D-dimer will be elevated. If you take the D-dimer blood test and it’s normal, there’s no blood clot to worry about.
It’s evaluated as a predictor of mortality, and to try to head off a variety of dangerous conditions. We do have the ability to alter D-dimer levels with medications. As to how frequently to test, there is no consensus on that. If you are out-patient, then perhaps once per month is good enough. If you have a history of having C*V1D – !9, then bear in mind that your D-dimer levels may be high for 3 – 4 months afterwards.
I know many of you will self-order this test. If you didn’t realize you can self-order your own blood tests, CLICK HERE to read my article about that. If your D-dimer is not in the normal range, be sure to consult a qualified physician, especially if your blood pressure is high or you have heart disease. While you’re waiting for your doctor’s appointment, consider a clean, nutrient-dense diet that you can be proud of, and perhaps some of the nutritional dietary supplements mentioned above.

Suzy Cohen, has been a licensed pharmacist for over 30 years and believes the best approach to chronic illness is a combination of natural medicine and conventional. She founded her own dietary supplement company specializing in custom-formulas, some of which have patents. With a special focus on functional medicine, thyroid health and drug nutrient depletion, Suzy is the author of several related books including Thyroid Healthy, Drug Muggers, Diabetes Without Drugs, and a nationally syndicated column.
