What's On This Page?
ToggleParkinson’s disease (PD) impacts 10 million people worldwide, and each year, 90,000 Americans are diagnosed with it! Men seem to be more likely to develop the condition. According to a new prevalence study, as the population ages, the number of people diagnosed with PD increases with age, regardless of sex. You can see more stats about this HERE.
I looked at a prevalence map and Montana and North Dakota have the fewest number of people (about 1,400 and 2,000 people respectively), whereas California and Florida top the list with the most people with Parkinson’s disease (85,000 and 64,000 people respectively).
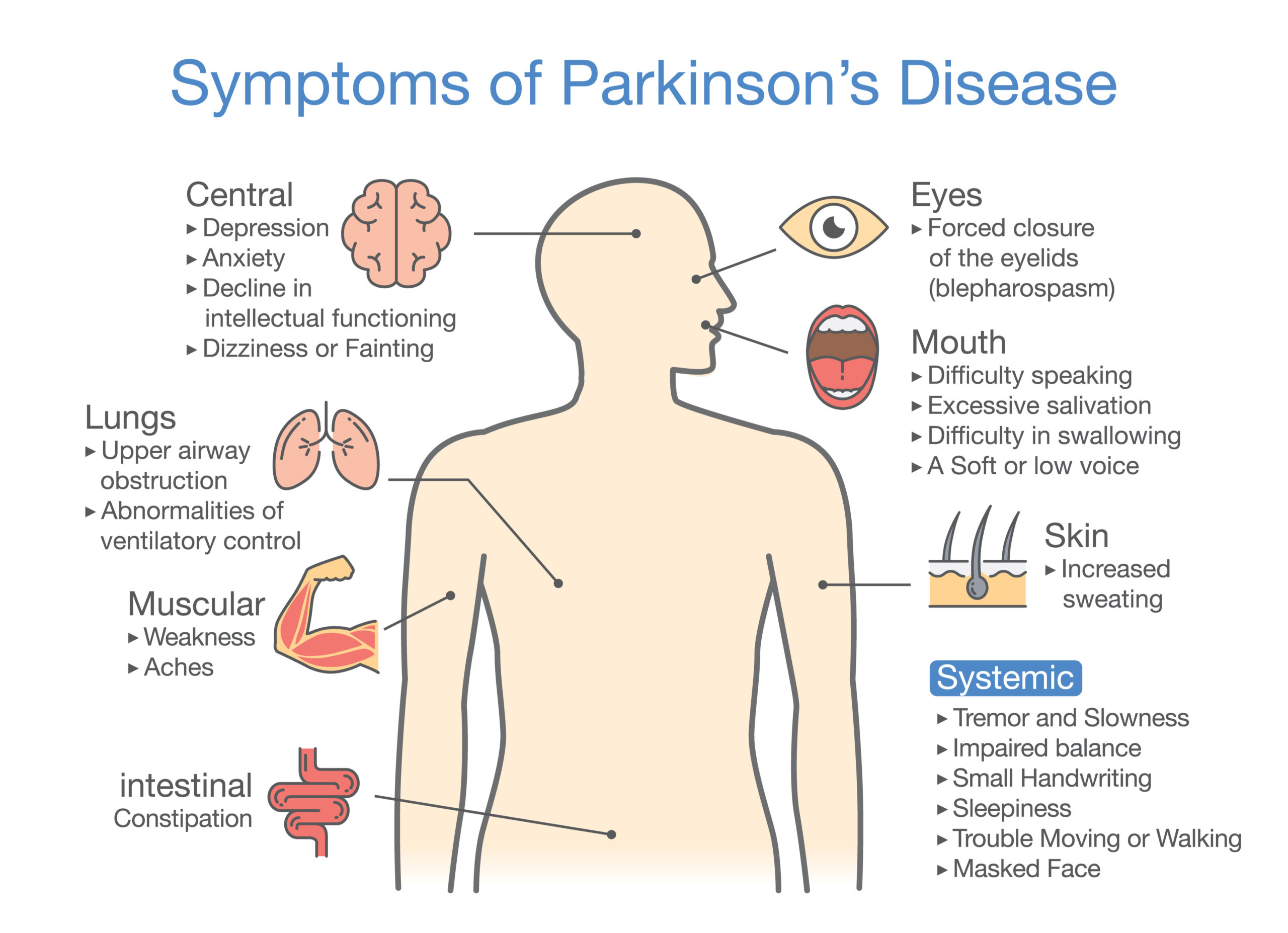
There are websites that offer much more detail regarding symptoms of Parkinson’s disease but a few telltale signs include tremor in the hands, slowed movements, muscle rigidity, poor balance, fatigue, or a distorted sense of smell. Among the cognitive signs and symptoms are disturbing dreams, restless sleep, confusion at night, anxiety, dementia or difficulty with comprehension.
Medications for PD
I could write a book on the medications and how to use them properly, but that is not the focus of my article today. I’m planning to give you nutritional options and some understanding of vitamin deficiencies, and how that impacts your prognosis. Nevertheless, I would be remiss if I did not mention the most common medications used for Parkinson’s disease.
These include Carbidopa-Levodopa (Sinemet, Atamet, Dhivy), MAO inhibitors such as Azilect, Eldepryl and Xadago, and of course, the newest class of meds called the COMT Inhibitors like tolcapone and entacapone. Those COMT inhibitors are used to help with tremor, stiffness and muscle rigidity/cramps, dizziness, and sudden freezing of gait… all of these are termed “motor” symptoms of Parkinson’s disease.
Speak to your physician or local pharmacist about the medications and which combination is right for you. There are, of course, many others not listed here.
During my research, I found some interesting findings about nutrients that might be useful for you. As a pharmacist, I can tell you that most if not all of these vitamins are okay to use in combination with medications, however, to be 100 percent sure they don’t interact with the specific medication you take, I want you to ask your own practitioner about taking these.
Here are some nutrients that may play an important adjunctive role in your Parkinson’s disease protocol:
Vitamin B12 (Methylcobalamin) for Parkinson’s Disease
We know that the B complex family of vitamins is important for proper nerve health. There is an important relationship between B12 specifically and Parkinson’s. Down below, I will showcase B1 (thiamine), but first let me talk about B12. We know that people with peripheral neuropathy are often deficient in B12. And it’s not just peripheral, there was a study in 2014 that found that B12 deficiency is one contributing factor and potential cause of SNF (Small Fiber Neuropathy).
A lack of B12 can affect thin-myelinated A-delta fibers and unmyelinated C fibers thus affecting the small fibers. If you do not know what SNF is, but you have diabetes or any kind of neuropathy please read THIS ARTICLE. Small fiber neuropathy occurs in Parkinson’s disease sometimes too.
Testing for B12
You can test yourself to determine levels of B12 easily. One popular test is a “Serum B12,” but I would also recommend the MMA (Methylmalonic Acid) test. I feel that this test will give you more information. An MMA test is most often used to diagnose vitamin B12 deficiency. You can also test your homocysteine while they’re sticking you because knowing those two levels will explain whether or not you have B12 deficiency. If both the MMA and the homocysteine are elevated, you have B12 deficiency in your tissues. And if it’s low in the tissues, it’s low in your myelin which protects your nerve fiber.
In summary, B12 could be very important for muscle health, and sensations of pain and neuropathy in a Parkinson’s disease patient. Furthermore, B12 is important for sleep as it makes melatonin in the body. Finally, B12 levels reflect your probiotic status. It is your microbiome that manufactures B12 for you, so if that is low, your gut needs some work.
By the way, if you’d like to go to a lab and self-order your own blood tests (to later share with your doctor at your next appointment), you can do that nowadays. Read THIS ARTICLE on how to self-order lab tests.
Vitamin D
A 2019 STUDY was among several others that determined vitamin D deficiency could impact the outcome for people with Parkinson’s disease. Keeping levels of D up high enough is difficult for the elderly too, it’s hard to get enough sunlight, and even if they do, their body doesn’t sulfate it, or convert it properly due to mild liver or kidney compromise.
But the study concurs with others in that chronic D deficiency will cause loss of dopaminergic neurons (the brain cells that you want more of if you have Parkinson’s disease). Low D translates to fewer of these brain cells, which then hastens symptoms of PD, especially cognitive function. Research does confirm that people with PD have significantly lower levels of D compared to those people who do not have the condition.
I could leave it here, but since I have a deep interest in genetics — something I’ve been fascinated with since my teenage years when I thought about becoming a geneticist — I’ll delve a little deeper to share some insights:
Research has revealed that millions of brain cells, especially in the substantial nigra, are equipped with doorways for vitamin D. These doorways, known as “vitamin D receptors” or VDR, are crucial for allowing vitamin D to enter the cells. In those with Parkinson’s disease, these receptors might not function as well as they should, which is thought to be linked to genetic factors.
So if you are born with specific variations, known as single nucleotide polymorphisms (SNPs, pronounced “snips”), in your VDR gene, it might influence your risk for developing Parkinson’s. While studies have suggested a connection, the relationship between these genetic factors and Parkinson’s is complex and still under investigation.
VDRs are not only crucial for brain health but are also abundantly present in brain regions like the putamen and caudate nucleus, which are involved in motor control (things like walking, reaching, or even speaking). This presence is significant, but the full implications for Parkinson’s disease are still being studied.

It’s also worth noting that if your body doesn’t effectively process vitamin D due to VDR issues, you could experience symptoms of deficiency. So you can lay in the sun all you want, but again, if you have VDR issues, you could still be deficient.
Fortunately, today’s genetic tests can provide some insights into your VDR status. Even if you have a VDR SNP, maintaining proper vitamin D levels by supplementing can be beneficial, but it’s important not to overdo it because you’ll become hypercalcemic.
That will impact your heart rhythm among other health issues. Always ensure your supplementation is done under proper medical guidance to balance benefits against potential risks.
CoQ10 and Parkinson’s Disease
Recent studies have highlighted the potential benefits of Coenzyme Q10 (CoQ10) also called “ubiquinone” for people with Parkinson’s disease. As you know, CoQ10 is a naturally occurring antioxidant that plays a pivotal role in energy production within the cells and it’s made in the liver. For people with Parkinson’s, CoQ10 levels are often found to be lower than average. Supplementation of this nutrient has been studied for its role in neuroprotection, potentially slowing the progression of symptoms.
A 2023 STUDY suggests that CoQ10 supplementation could lead to improved symptoms in PD patients. This is attributed to its antioxidant properties and its role in supporting mitochondrial function, which is often compromised in neurodegenerative disorders such as this. While CoQ10 does NOT cure Parkinson’s, it may enhance cellular energy levels and reduce the oxidative damage to neurons, offering a complementary and easily accessible supplement to try.
Before starting any new supplement, it’s crucial to consult with a healthcare provider, as CoQ10 can interact with certain medications, including blood thinners and chemotherapy.
Fish Oil
Sometimes tremors respond to DHA fish oil, and this could be a promising strategy to slow down the progression. Remember, even if our drugs are useful, they don’t cure it, so this natural omega-3 fatty acid is probably safe and might be slightly effective for the management of tremors and other symptoms in the early stages.
Ask your doctor of course, because fish oils are blood thinners. These work by improving synaptic development and functionality. Fish oils are useful at making things more ‘slippery’ in the sense that the signals travel faster in the body, thus communication between neurons will improve. Research confirms that essential fatty acids contribute to improving cognitive activity and more neuroplasticity. You may be interested in this article entitled, Are Fish Oils Your Only Option.

Vitamin B1 (Thiamine)
Thiamine, also known as vitamin B1, is essential for the proper functioning of the nervous system. Supplements of this important B vitamin are always found in B Complex vitamins including Mito B Complex. Emerging research in 2023 has started to explore the relationship between thiamine deficiency and Parkinson’s disease.
Thiamine is vital for glucose metabolism, which is critical for brain function. A deficiency in vitamin B1 has been linked to various neurological symptoms that can exacerbate Parkinson’s manifestations, such as cognitive decline and muscle weakness.
Parkinson’s patients may be at higher risk for B1 deficiency due to dietary gaps, a leaky gut as in GI malabsorption, or the use of certain medications and/or alcohol that act like drug muggers and deplete vitamin B1 levels.
Supplementing with thiamine has shown promise in some clinical trials, specifically to help improve motor function and cognitive function.*
Although these findings are promising, and you may be eager to try B1, you might consider a simple blood test to see if you’re low in it or not. Addressing a B1 deficiency may offer a new avenue for symptom management in Parkinson’s disease, and it’s affordable and easy to buy.

Summary
In this blog, we delved into the complexities of Parkinson’s disease which sadly affects millions of people globally. As we age, the prevalence of Parkinson’s increases, highlighting the urgent need for effective management strategies. While traditional medications play a critical role in managing Parkinson’s, we explored the promising potential of Coenzyme Q10 (CoQ10) and vitamin B12, vitamin D and thiamine in supporting neurological health.*
CoQ10 was studied a few times. The positive benefit seen in 2023 isn’t always reproducible, but it makes a lot of sense in terms of mechanism of action. I think it could be a key player in cellular energy production and a powerful antioxidant that one could try. It is something we make in the human body, but it’s reduced by many medications including STATINS.
It has the potential to protect the nervous system and improve symptoms associated with neurological diseases, through its antioxidant effect. Vitamin B12 helps to form myelin in the nerve health and its potential cannot be overstated, with deficiencies linked to various neurological impairments as well as confusion.
I hope my blog offered you a holistic view of Parkinson’s management today. Feel free to share it. By understanding and addressing vitamin deficiencies and exploring supplements like CoQ10, individuals with Parkinson’s can find new hope and potentially improved outcomes in their journey with this challenging disease.

Suzy Cohen, has been a licensed pharmacist for over 30 years and believes the best approach to chronic illness is a combination of natural medicine and conventional. She founded her own dietary supplement company specializing in custom-formulas, some of which have patents. With a special focus on functional medicine, thyroid health and drug nutrient depletion, Suzy is the author of several related books including Thyroid Healthy, Drug Muggers, Diabetes Without Drugs, and a nationally syndicated column.