What's On This Page?
ToggleThis blog is about unintended weight loss in people, which is called cachexia and is pronounced as kuh-KEK-see-uh. The stress is on the second syllable, “KEK.”
That’s the medical term that describes people who you may have seen. They look too thin and frail because they are essentially wasting away! It’s common in older folks due to long-standing illness or dementia.
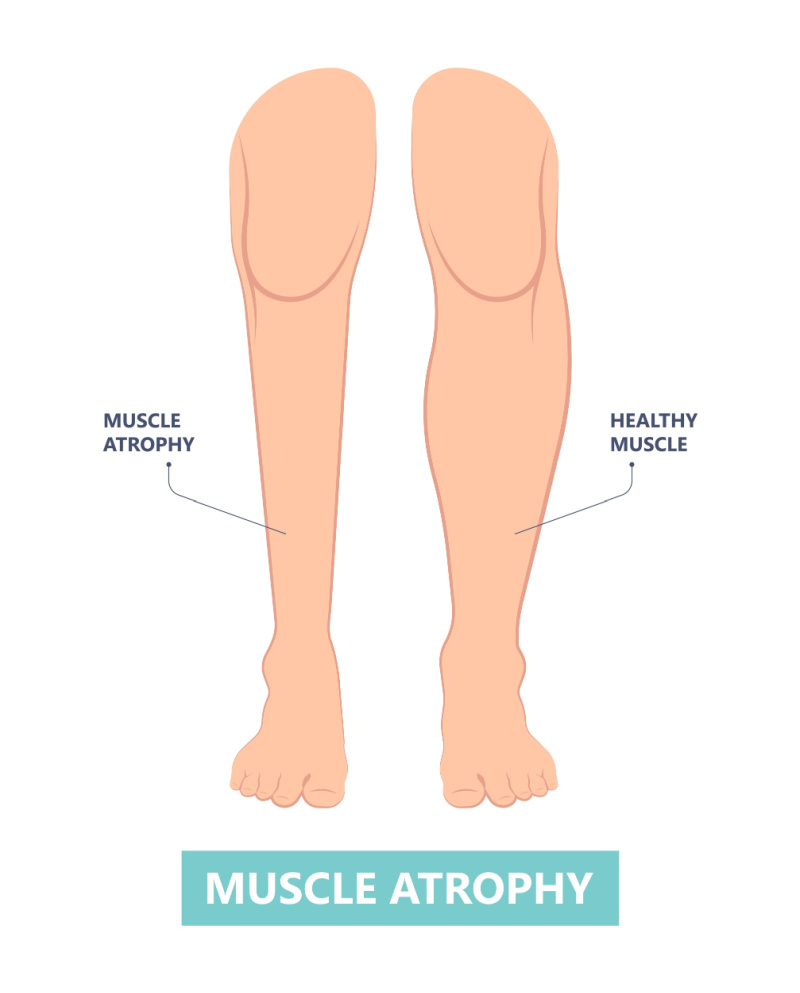
Many assume it’s due to the person not eating, but that’s not it. Cachexia is actually a very complex and severe “wasting syndrome” characterized by significant weight loss, muscle atrophy, weakness, and loss of appetite. It often occurs in individuals with advanced stages of chronic diseases such as cancer, heart failure, and diabetes. I’ve listed more risk factors down below.
Unlike cases of starvation or malnutrition, cachexia involves the body’s metabolism being disrupted, which then causes the breakdown of muscle tissue and loss of body fat. It requires medical attention and treatment because it isn’t about eating more, it’s about reversing the metabolic changes and reducing inflammation so that the food you eat gets incorporated into the body properly.
Is it Just About Growing Older?
We see cachexia in the elderly most frequently, so the assumption is it occurs naturally with age. That is not true. Cachexia is a symptom that can occur at any age, even in children or adolescents, and in kids that age, it’s often associated with cancer or chemotherapy.
You see this condition occur in tandem with reduced muscle function which is medically termed “sarcopenia.” Read more HERE.
It’s safe to say the syndrome occurs as the body’s response to some other serious illnesses, it’s not a disease in and of itself. Mortality rates in people with it vary based on their underlying conditions. As one might expect, cancer-induced cases have higher mortality rates than patients with COPD or heart failure.

What happens is the body’s normal balance of producing and utilizing energy gets all messed up. The immune system and inflammation play a big role here. When you’re dealing with an illness, the immune system can go haywire and release a bunch of substances (pro-inflammatory cytokines) that cause inflammation. These cytokines put the body into full attack mode. It’s on fire!
As a result, the body shifts into a “survival mode.” It starts breaking down muscle and fat to get more energy to fight off whatever it thinks is a threat. As this happens, muscle tone declines, and a person begins to lose weight unintentionally. Those cytokines also mess with how the body uses nutrients. They can make it harder for the body to absorb important things like protein, which is absolutely essential to build muscle.
The best analogy for what the body is doing during cachexia is this: Imagine trying to keep the lights on in your house during a power blackout by burning all your furniture for power – not the best plan!
The Inflammation is Caused by Cytokines
I keep mentioning cytokines because they light the fire. You might be curious about which ones they are that become elevated in the body during cachexia. If we know which ones they are, we can still figure out how to reduce them, even if we can’t cure the disease itself. It might even help with the associated sarcopenia associated.
The most notable pro-inflammatory cytokines are IL-6 (interleukin-6) and TNFα (tumor necrosis factor-alpha). These cytokines are consistently found at elevated levels in cachexia and are often referred to as the ‘troublemakers’ because they trigger inflammation and subsequent muscle wasting. Reducing IL-6 and TNFα can be beneficial and improve symptoms, but it doesn’t cure cachexia.

IL-6 and TNFα are both measurable if you take a simple blood test.
There are both natural and pharmaceutical approaches to reduce the levels of these cytokines which can alleviate some effects, and dampen the “fire” by throwing a wet blanket on them so to speak. Before I get to your options, let’s discuss risk factors because prevention is possible.
Risk Factors
Chronic Diseases: Conditions like cancer, heart failure, chronic obstructive pulmonary disease (COPD), kidney disease, and advanced HIV/AIDS increase the risk of cachexia. While diabetes itself might not directly cause it, uncontrolled diabetes and chronic kidney disease will hasten muscle wasting and weight loss. Treating chronic illness is the best way to avoid the problem.
With cancer-induced cases, there are 3 clinical stages technically speaking: pre-cachexia, cachexia, and what’s called refractory cachexia but not everyone goes through all the stages. The refractory stage is when the person is expected to have less than 3 months of survival. There is an organization that provides information: Cancer Cachexia Society.
Dementia-related cachexia is common in advanced stages of the cognitive disorder. It happens due to changes in brain function which then affect appetite regulation which leads to a refusal to eat, resulting in weight loss and muscle wasting. Dysphagia or discomfort while swallowing contributes to the problem in the elderly. I wrote an article on that very topic, CLICK HERE to read it.
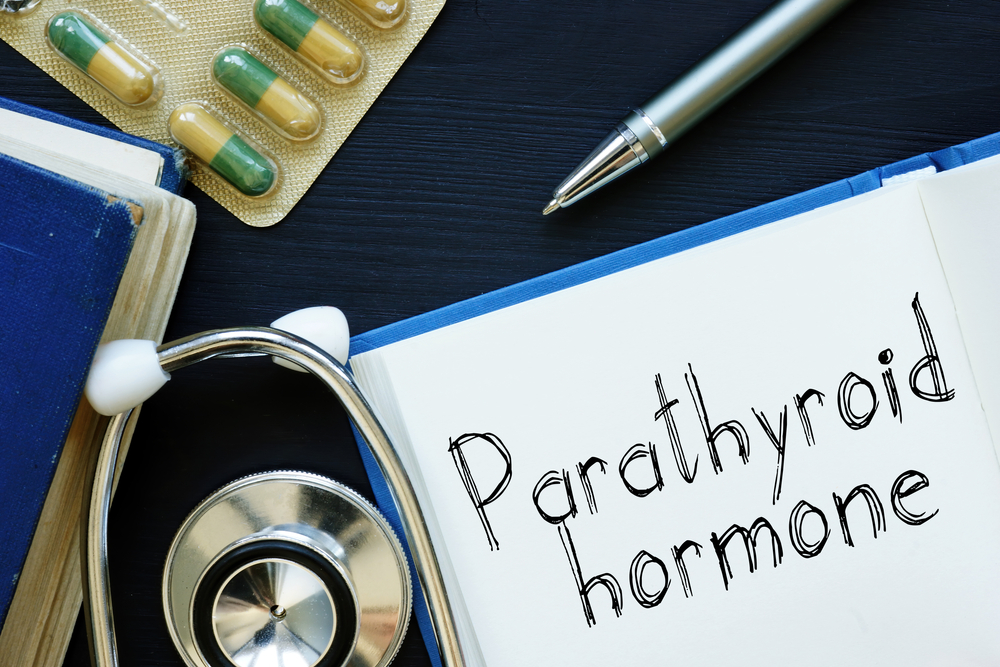
What if your PTH (parathyroid hormone) is high? Termed hyperparathyroidism, this is a condition where the parathyroid glands produce too much parathyroid hormone, and if left untreated, it causes bone and muscle breakdown over time.
This can potentially lead to muscle wasting and contribute to cachexia. It’s not a well-known risk factor, but it does exist so I want you to know about it because this condition is treatable.
Long-Term Inflammation: Chronic inflammation, often seen in conditions like rheumatoid arthritis, or other autoimmune conditions exacerbate cachexia. Going on a healthy diet is my advice to deal with autoimmunity. By “healthy diet” I mean keto or keto-carnivore diets. I no longer believe in the food pyramid.
Age: It’s more common in older adults not so much due to their age, but more because of decades-long illness, inflammation and/or pain. I know healthy 80-year-olds without cachexia, so it’s not the number itself.
Malnutrition: Individuals who are not receiving adequate nutrition due to appetite loss, lack of available food, or difficulty eating are at a higher risk. That said, malnutrition is not the same as cachexia. Malnutrition would be solved to some extent by eating more food, whereas cachexia would not be.
You might think that a feeding tube could resolve the situation, but no, that does not work because it is a problem of disordered metabolism, not low calories.
Strategies for People with Diabetes-Induced Cachexia
I want to elaborate here because many people assume the neuropathy or high blood sugar levels cause the cachexia, but those things only exacerbate it. They don’t cause it. Diabetes, especially when poorly controlled, causes chronic inflammation in the body, meaning high levels of pro-inflammatory cytokines. I’m referring to IL-6 and TNFα, which are tightly associated with cachexia.
Also, if you have type 2 diabetes, you have insulin resistance, which is where the body’s cells don’t respond effectively to insulin floating around. It is this insulin resistance that causes muscle protein breakdown and an inability to use glucose for energy! You probably know that chronically high levels of blood sugar contribute to atrophy.
Then there’s poor glycemic control (ups and downs and fluctuating blood sugar levels). Finally, neuropathy plays a small role in that it leads to damaged nerves, which causes muscle weakness and makes it harder to exercise (adding to muscle wasting). All of this causes a major metabolic disturbance that drives the cachexia.
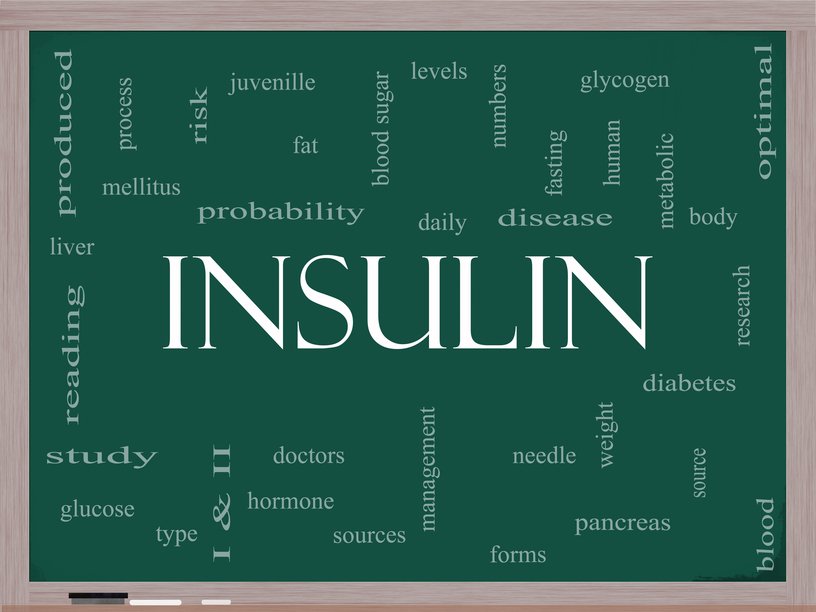
So the strategy in a person with diabetes-induced cachexia is multi-faceted. Have the doctor work on maintaining glycemic control so you have more stable blood sugars, and less highs/lows. You also want to reduce high levels of insulin!
Check out my formula called GlucoScript which supports a healthy pancreas, blood sugar levels and cholesterol*
Eat more protein because this is essential to support muscle health and prevent malnutrition. Exercise to your ability because this counters the atrophy caused by neuropathy and high blood sugar. It’s not a bad idea to get your sex hormones evaluated so that imbalances can be addressed, if nothing else, it makes you feel more youthful and builds muscle mass.
Stay on top of your appointments. If you take medicine, make sure you restore what the “drug mugger” stole. Metformin is a potent drug mugger of Vitamin B12.
Strategies for People with Cancer-Induced Cachexia
Cachexia in individuals with cancer is a common and complex condition that results from both the presence of cancer and the body’s response to it. Your oncologist is your best source for information on this. I will at least address the basics here:
Many cancer types can trigger a systemic inflammatory response in the body. This inflammation is driven by pro-inflammatory cytokines and can lead to muscle wasting and weight loss. Tumors “eat” a lot of energy and nutrients from the body, stealing it from normal tissue. This diversion of energy and nutrients results in muscle breakdown and loss of weight.
Then there are changes in appetite whether that’s from the tumor itself, or the treatments. Regardless, there is usually a reduction in food intake compounded with altered nutrient absorption from the gut, changes in digestion and transit time, as well as increased ATP expenditure.
Some cancers produce hormones or substances that can affect metabolism and appetite. For example, pancreatic cancer can lead to high levels of insulin, which can result in muscle wasting. I could go on, but these are the main points. Add in pain and fatigue, and then depression (!) and you can see these as other primary contributors to cachexia!
An oncologist or dietician can best help you. I can tell you that addressing the emaciation in individuals with cancer is very challenging, but it does improve quality of life if you can do it. Ensure adequate caloric intake each day, and eating proteins is crucial to help offset muscle loss. There are IV cocktails for nutrition as well.
Managing cancer-related inflammation through medications, lifestyle changes, or nutritional interventions may help mitigate muscle wasting. Controlling pain will be critical. Physical therapy isn’t a bad idea at all but it should be tailored to the individual’s capabilities can help counteract muscle weakness and lack of use.
Psychological support should be emphasized as well. A comprehensive approach involving an entire team of healthcare professionals will provide the best outcome. Managing inflammation is critical because that helps reduce pain, improve signs of malnutrition, and reduce cytokines.
Cytokine Involvement
I mentioned cytokines earlier. Did you know that lung cancer, kidney cancer, and ovarian cancer among others have high levels of IL-6? Breast cancer is associated with high levels of TNFα. And then there’s the spike protein.
You’ve probably heard of that these past couple of years. The spike protein can cause a strong reaction in the body, leading to the production IL-6, IL-1β, TNFα, CXCL1, CXCL2, and CCL2. These substances play a role in the body’s immune response but when elevated, lead to inflammation.
Let’s discuss how to control those cytokines next. I have some helpful tips to share.
The 14 Best Natural and Conventional Options to Help
Remember, what works for one person might not work the same way for another. It’s always a good idea to chat with a dietician or other qualified practitioner to design the best strategy for you. One more thing real quick, a comprehensive approach involving medical supervision, proper nutrition, and physical therapy is needed, it’s not just about popping supplements!
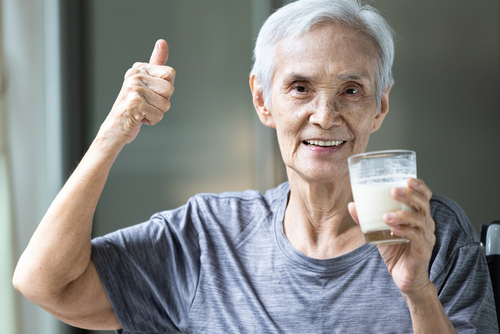
1. Drink Nutrition
High-calorie, high-protein supplements, such as nutritional drinks, can be recommended to support caloric intake and prevent further muscle wasting. For individuals with dementia-related weight loss, vitamin-packed drinks like Prosure®, Boost®, Ensure®, Glucerna® help fill a nutritional gap. Each brand offers multiple flavors. Look for options that are high in both protein and calories, as this can provide energy and support muscle maintenance (reduce sarcopenia).
2. Omega-3 fatty acids
Keep in mind that while these herbs could have potential benefits, they aren’t a substitute for proper medical care, they support cytokine balance. You can find these sold widely as “fish oils” by many brands. The reduction of inflammation in the body contributes to more general health and well-being. These are not appetite stimulants. The recommended dose for EPA (eicosapentaenoic acid) for cancer cachexia patients is about 2000 mg per day. The studies about this vary, but most say that it takes about 2 – 3 months for benefits to appear using this supplement.

3. Cannabinoids
From the marijuana plant – natural compounds called cannabinoids exist in the plant. This appetite-stimulating effect dubbed “the munchies” has been recognized for quite some time, and certain legal forms have been used in clinical settings for cancer patients. As you probably know, there are edible forms (ie gummies, brownies, etc) as well as classic “joint” which is smoked. A joint has both THC and CBD, where the former compound has psychoactive effects and the latter does not.
Cannabis compounds activate the CB1 receptor, which can lead to increased food consumption and a heightened sense of taste and smell. This is what makes munching more appealing. A study published in the journal ‘Pharmacology, Biochemistry, and Behavior’ in 2005 found that dronabinol increased appetite and food intake in patients with Alzheimer’s disease.
Dronabinol is a prescription version of cannabis that your doctor can prescribe for you.
There are legal considerations regarding use of regular plant-grown cannabis (vs. dronabinol), in each state so make sure you follow the law if you’re using this as an appetite stimulant. Also, just because you eat more doesn’t mean you can counteract the effects of long-standing cachexia.

4. Anti-Inflammatory Drugs
Medications like nonsteroidal anti-inflammatory drugs (NSAIDs) or corticosteroids might be used to manage inflammation associated with cachexia. NSAIDs are the category of drugs you know as ibuprofen, naproxen and others. Acetaminophen (Tylenol®) is not an NSAID. If you’d like to know the differences and which is better, CLICK HERE to read my other article.
5. Progestins
Drugs like megestrol acetate can stimulate appetite and promote weight gain in people with cachexia, especially in cancer-related cases. FYI, progestins are a category of synthetic medications that look like the natural hormone called progesterone. But natural progesterone hasn’t been tested in patients, only progestins like megestrol acetate. By the way, the brand name Megace® is no longer on the market, only generics.
6. Anabolic Steroids
These medications, like oxandrolone, can help increase muscle mass and appetite in some cases. However, they may come with potential side effects like headache, nausea/vomiting (which is ironic because that will make malnutrition worse!), bone loss, immune suppression, acne, hair loss, oily skin and low libido.
7. Ghrelin Agonists
Ghrelin is a hormone that can stimulate appetite and increase body weight. Some medications can mimic ghrelin’s effects and might be used in certain cases. One such medication is “Anamorelin” which is a ghrelin receptor agonist. It makes you hungrier. They use this drug to improve symptoms of pancreatic or other GI-related cancer and it stimulates more growth hormone release. Studies suggest it improves anorexia, and possibly lean body mass.
8. Anti-TNF Drugs
I’m going to list the medications that target and reduce TNF-alpha (TNFα), a major pro-inflammatory cytokine involved in cachexia. It just so happens that TNFα is high in many autoimmune conditions, including rheumatoid, so you may recognize these drugs names from TV commercials.

The most popular anti-TNF drugs include Humira® (adalimumab), Remicade® (infliximab), and Enbrel® (etanercept). There are lots of side effects that could potentially occur with these drugs, so risk vs. benefit must be discussed with your physician.
Don’t just ask for the drug because you saw a TV commercial. Think it through. The benefits are reduced self-attack, the risks vary with each individual.
What About Natural Anti-TNF Herbs?
In cases where you want to try natural options to support your weight and reduce cytokines, they exist! The following items are sold widely at health food stores, supermarkets, online sellers and spice shops.
There are 5 very powerful anti-TNF options that are easy to incorporate into your day. They are curcumin, ginger, boswellia, green tea and resveratrol and so I’ve finished up my list with the 5 BEST natural Anti-TNF inhibitors:
9. Curcumin
Found in turmeric, curcumin has anti-inflammatory properties and may help lower TNFα levels. I put this in Joint Script which isn’t just for joints. You can cook with this spice too! It reduces TNFα and suppresses inflammation. There are supplements of it and of course the spice!
I put a very expensive patented brand called C3® Curcumin in my custom formula Joint Script® because it is so clean, powerful, has 3 different biologically active forms of curcuminoids (all of which have been clinically studied). There are hundreds of studies that show curcumin can reduce IL-6 and TNFα. Here’s one PAPER.
10. Ginger
Ginger contains bioactive compounds with anti-inflammatory effects that might help reduce TNFα production. Make yourself a tea, or grate some ginger in your soup and recipes. Buy it fresh from the produce store for best effects, or use a dry powdered spice form. Ginger has been shown to clinically reduce IL-6 by about 15% in some individuals. Read the PAPER here.

11. Boswellia
Also known as frankincense, boswellia has anti-inflammatory properties and may help reduce TNFα levels and IL-6. I also put this in Joint Script (and topically in my collagen serum!). Boswellia has been studied extensively. Read THIS.
It can not only suppress IL-6 and TNFα, but also Nitric Oxide and COX-2 that’s why you intelligent formulators put it in their joint supplements rather than glucosamine which doesn’t even absorb well (and causes lots of gas). By the way, boswellia’s other name is frankincense, I’m sure you know that!
12. Green Tea
Drink it! The antioxidants in green tea, particularly epigallocatechin gallate (EGCG), have been studied for their potential to inhibit TNFα. Supplements of this are available too. But to make it easy, and prevent swallowing fatigue, you could just drink a cup of green tea while you read the news or a book!
It’s easy to incorporate this into your day. It’s okay to add honey because high-quality brands have potent anti-inflammatory effects too. Some RESEARCH from 2021 shows it reduces all kinds of pro-inflammatory cytokines like IL-1β, IL-6, and TNFα. Read my article on the benefits of HONEY.

13. Resveratrol
Found in grapes and red wine, resveratrol has been studied for its potential to modulate inflammatory pathways, including TNFα. Here’s one of many studies, this is found at the NIH, National Library of Medicine.
And here’s a PAPER showing the combination of resveratrol with curcumin.
14. HMB (Beta-Hydroxy Beta-Methylbutyrate)
This is a substance made from the amino acid leucine. And leucine is a building block of protein in our body. This more biologically active form of leucine called “HMB” helps our muscles grow and prevents muscle breakdown.
For healthy young people, HMB may help muscles get bigger, especially when combined with exercise. It might also protect the muscles of elderly people who can’t move much due to being sedentary or having an illness. You can supplement with HMB, it comes as a capsule, or a powder, and it’s made using a calcium molecule. It’s sold on Amazon. The recommended dose is about 3 grams (3000 milligrams) per day, and as for studies about harmful effects, I haven’t seen any.
Researchers think this works by slowing down certain chemical reactions in the body that would otherwise destroy muscle proteins. Oncologists have combined HMB with both glutamine and arginine supplements, and that trio seems to work even better than HMB alone. It may take about 4 weeks of regular use for HMB to begin showing benefits and muscle protection (at least in cancer patients), so it’s essential to be patient and consistent with it, and have a chat with your doctor
What Should You Eat?
People wonder what you should avoid eating if you have this condition, and the most important thing would be processed (junk) food, followed by alcohol which spawns free radical damage and caffeine which suppresses appetite. Also, fiber, while it’s kind of important, I think excessive amounts can fill you up quickly and make it harder to get the calories needed.
Prioritize nutrient-rich, calorie-dense foods and animal protein that support muscle mass.
Summary
Cachexia is the result of a bigger medical condition. It happens when some other condition is going on. It’s important to understand that medical problems always contribute to the development of the condition, so there is not a single cause. I think that’s what makes it so difficult to treat. It’s also why there isn’t a single solution for everyone with the problem.
You’re having to get to the underlying illness or disorder of each person with wasting, in order to help them. So this is a complex syndrome involving excessive inflammation, impaired immune responses, and altered metabolism. There isn’t just one thing, there are many.
There are prescription medications that can be used to address cachexia, as well as its underlying causes. The suitability of any medication depends on your specific condition, medical history, and other factors. There is no panacea.
There are also natural interventions as shared above.
Time is of the essence for the very frail. Most people will try to eat if you ask them to, or cook for them. But there are others who are just not hungry at all, or they’re too picky an eater to eat what you make for them. Just remember, it’s not as much about caloric intake as it is about metabolism. This is why experienced medical intervention, proper nutritional support, and disease management works, versus just eating more.
Simply eating more may not be enough to counteract the effects of cachexia, you have to target the cytokines that are high causing the disease and inflammation. And eating is sometimes uncomfortable, especially for a person with dysphagia, contributing to even more weight loss. This will lead to frailty, reduced quality of life, and increased falls and fractures.
Natural herbal remedies like curcumin, resveratrol, ginger, and others may help reduce cytokines and restore balance to the inflammation problem. Other agents are available that stimulate appetite like cannabis and megestrol. Still, there are nutritional drinks that boost calories and fill a nutrient gap.
A dietician and physician will be necessary to reverse the condition because together they can work on solving the medical condition driving the cachexia, while simultaneously designing a proper meal program. Eating carbs is not the answer. Addressing the underlying conditions with appropriate medical care and management is essential to help prevent or mitigate cachexia’s effects.
If someone is experiencing weight loss and muscle wasting due to these or other underlying conditions, consulting a healthcare professional is recommended.

Suzy Cohen, has been a licensed pharmacist for over 30 years and believes the best approach to chronic illness is a combination of natural medicine and conventional. She founded her own dietary supplement company specializing in custom-formulas, some of which have patents. With a special focus on functional medicine, thyroid health and drug nutrient depletion, Suzy is the author of several related books including Thyroid Healthy, Drug Muggers, Diabetes Without Drugs, and a nationally syndicated column.
