What's On This Page?
ToggleIron deficiency anemia or “IDA” is one of the most common yet overlooked health issues, affecting energy, cognitive function, and overall vitality. It is something I have dealt with myself in years past, making it a focus of my research. At one point in my 40s, my ferritin levels dropped dangerously low, hitting a value of just 8.
Thankfully, this issue was resolved for the most part, leaving me borderline anemic for many years, and it’s something I track to this day. I had lowered my ferritin (reducing iron stores) because I’d been taking calcium supplements after the hyperparathyroidism surgery which you can learn more about in this ARTICLE. But the point is calcium intake reduces iron absorption, and if you also drink coffee, you’re sure to develop IDA. Taking antacids or acid blockers will also reduce iron. These are common things that people do all the time, never thinking that their iron levels will be impacted – but they will be.
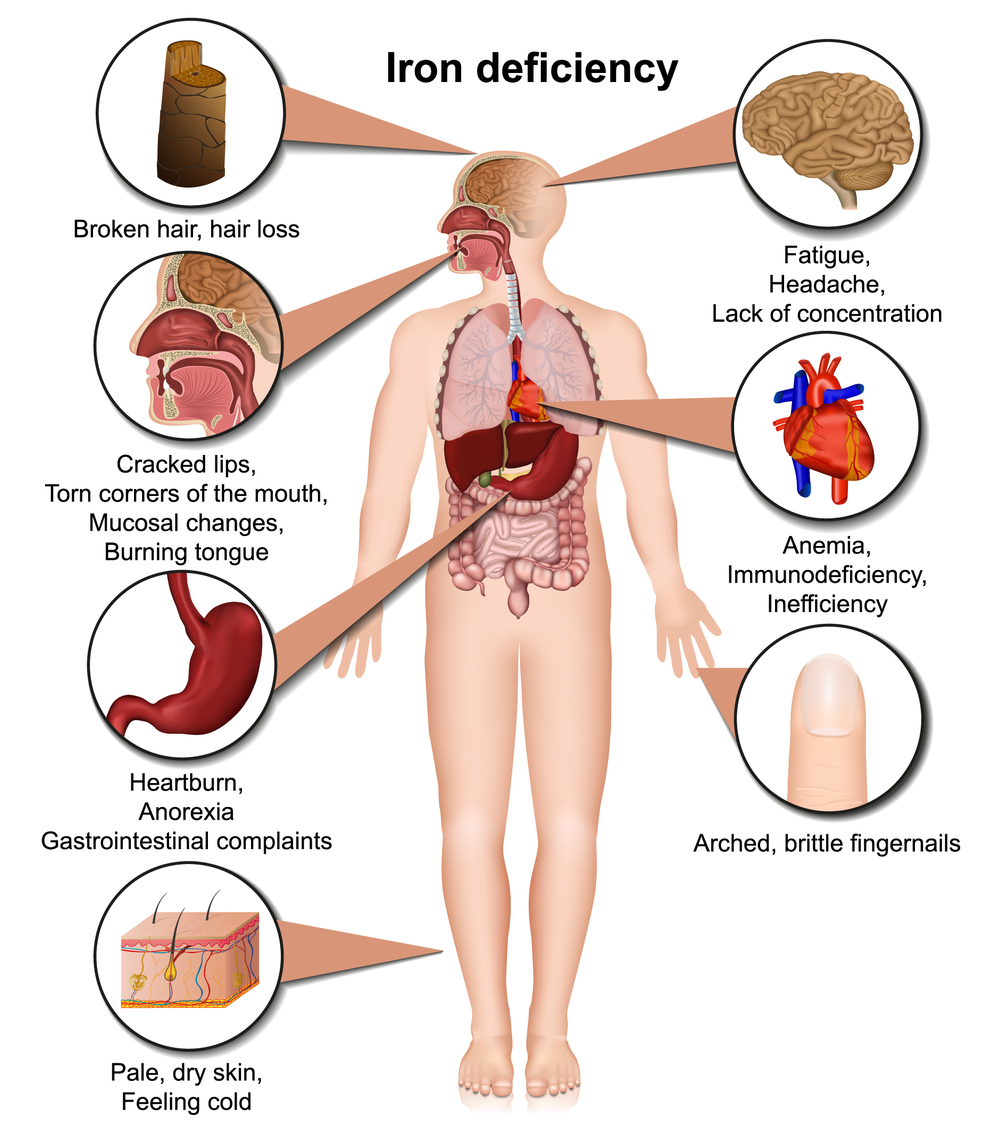
Perhaps many of you are struggling with borderline anemia, or even very low ferritin levels – this can leave you feeling unwell. Iron deficiency anemia not only causes fatigue, it can also bring on shortness of breath, dizziness, brittle nails, and even hair loss depending on the severity. With pica, people may crave dirt and, in some bizarre cases, even eat it, driven by a compulsion linked to nutritional deficiencies like low iron! I’ve never known anyone to do this, but it can happen so I’m listing it if only for the weirdness of it!
The symptoms of iron deficiency anemia often creep in quietly, long before standard lab tests reveal it. Borderline cases are what I see mostly, which is where you fall into the “normal” range on some of the 8 blood tests (scroll down below), but you’re at the low end of the spectrum. While you might rely on coffee, caffeinated drinks, or pills for a quick energy boost, these stimulants, along with alcohol, act as “drug muggers” of iron. They gradually deplete your iron stores over time, potentially worsening fatigue and energy issues.
It’s easy to attribute low energy to a busy lifestyle or aging, the root cause could be something as simple and correctable as low iron. Let’s dive into how iron functions in your body, what tests to ask for, and the best strategies to restore your levels naturally and with supplements.
Why Iron is Essential
Iron isn’t hyped up as much as other minerals like magnesium and calcium, but nonetheless, it’s important. Iron acts as your body’s oxygen delivery system. It’s a critical component of hemoglobin, the protein in red blood cells that transports oxygen to every single cell. Without enough iron, your body struggles to make adequate hemoglobin, leaving your tissues starved of oxygen.
This isn’t just about oxygen, though. Iron also supports:
- Energy production –Iron helps your cells make energy by being part of proteins in the mitochondria that move electrons along a chain, creating the energy needed to make ATP, the fuel your body runs on.
- Brain health – playing a role in neurotransmitter synthesis and focus. You may want to read my other article, 8 Ways to Save Your Brain and Calm Down. And this is another interesting read: 5 Tips to Boost Serotonin: How the Gut-Brain Axis Works.
- Immune function – helping your body fight off infections. Many people have lingering syptoms from cold/flu or covid, and if this is the case for you, READ THIS ARTICLE.
When iron levels drop, even slightly, you might feel tired despite sleeping well. You may struggle with mental clarity or notice physical changes like pale skin, brittle nails, or thinning hair. These early signs can snowball into more serious issues like rapid heart rate, shortness of breath, and full-blown anemia if not addressed.
Recognizing the Signs of Iron Deficiency
Iron deficiency often starts subtly. You might notice some of these signs and symptoms:
- Feeling worn out or sluggish even after a good night’s sleep.
- Wanting to lie down during the day to recuperate from not much!
- Restless legs at night, making it hard to wind down.
- Difficulty catching your breath during mild exercise or even walking up stairs.
- Hair that’s shedding more than usual or nails that break easily.
- A faster-than-usual heartbeat or palpitations.
- Dry or cracked corners of the mouth (medically called angular cheilitis).
- Spoon-shaped nails (koilonychia)
- Fingernails are brittle and break easily. (Aside from iron, COLLAGEN DEFICIENCY may be at play).
- Difficulty concentrating, forgetfulness, or feeling mentally “cloudy.”
- Unexplained irritability or feeling low or apathetic can sometimes be linked to iron deficiency.
- Pale skin and a lightening in color of your inner eyelids, gums, or nail beds. Even lips may be pale and match your skin.
- Burning mouth syndrome
- Tinnitus (ringing of the ears) which is linked to reduced blood flow and oxygenation.
- Chest heaviness during exertion
- Muscle fatigue or weakness and difficulty sustaining physical activities (because of reduced oxygen delivery to muscles).
It’s not uncommon for these symptoms to be dismissed or chalked up to stress. However, if they persist, especially in combination, it’s worth investigating your iron levels.
8 Key Tests for Diagnosing Iron Deficiency
If you suspect iron deficiency, it’s important to go beyond the basic hemoglobin test. Hemoglobin alone doesn’t tell the full story, especially in the early stages. Ask your doctor for these key markers:
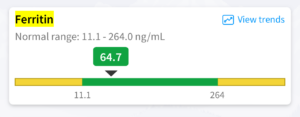
- Ferritin: This reflects your stored iron. Levels below 30 ng/mL often indicate low reserves, even if your other labs are in the “normal” range. However, even “low-normal” ferritin can signal potential problems. If your ferritin is just barely within range, it’s worth considering iron deficiency anemia, especially if symptoms align.
-
Hemoglobin and Hematocrit: These are standard components of a Complete Blood Count (CBC) and indicate anemia. However, they can be normal in early iron deficiency, so they should always be interpreted alongside ferritin and transferrin saturation.
-
Serum Iron and Transferrin Saturation: These measure how much iron is available for immediate use. Low serum iron paired with a low saturation percentage (below 20%) is a red flag for deficiency. These tests measure how much iron is available for immediate use and how efficiently it’s being transported.
-
TIBC (Total Iron Binding Capacity): This test measures your body’s capacity to bind and transport iron. A high TIBC often signals iron deficiency because your body is trying to grab every bit of iron it can.
-
Reticulocyte Count: This shows whether your bone marrow is producing enough new red blood cells. A low reticulocyte count suggests your body is struggling to keep up due to insufficient iron.
-
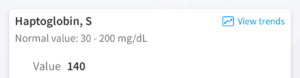
Haptoglobin: This test assesses whether there is excessive red blood cell destruction in your body. When haptoglobin levels are low, it may indicate hemolysis (red blood cell breakdown), which can contribute to iron depletion. This is particularly relevant in cases where anemia isn’t solely due to insufficient iron intake but involves loss through red cell turnover.
-
Hepcidin: A relatively newer marker, hepcidin is a hormone that regulates iron absorption and storage. High levels can block iron absorption, contributing to deficiency despite adequate dietary intake. Elevated hepcidin is often seen in cases of chronic inflammation, infections, or certain metabolic disorders, making it a valuable test for uncovering hidden causes of iron deficiency anemia.
- Lactate Dehydrogenase: LDH testing isn’t typically used for Iron Deficiency Anemia but can help distinguish it from other types of anemia, like hemolytic or megaloblastic anemia. Elevated LDH levels often indicate red blood cell destruction or tissue damage, not commonly seen in iron deficiency anemia.
Causes of Iron Deficiency Anemia: It’s Not Always About Diet
While diet is often a factor, low iron levels can stem from a variety of issues:
- Blood Loss:
- Heavy periods are the most common cause for menstruating women. (If you have PMS, read THIS ARTICLE for 7 hacks).
- Chronic gastrointestinal bleeding (from ulcers or GERD/reflux, polyps, or hemorrhoids) is another frequent culprit. Chronic GERD can lead to esophagitis, which might result in tiny amounts of chronic blood loss from the esophageal lining. This blood loss can exacerbate iron deficiency anemia over a long time.
- Poor Absorption:
- Medications like proton pump inhibitors (PPIs) or antacids reduce stomach acid, which is necessary for absorbing iron.
- Conditions like celiac disease or inflammatory bowel disease impair your gut’s ability to take in nutrients, including iron.
- Dietary Factors:
- Plant-based eaters may struggle with iron absorption, as non-heme iron (from plants) isn’t as bioavailable as heme iron (from animal products).
- Regular consumption of coffee or tea with meals can block iron absorption due to tannins.
- Increased Demand:
- Pregnancy, breastfeeding, and rapid growth spurts in teens increase the body’s iron requirements.
-
Infections:
- Tuberculosis
- Osteomyelitis
- Parasitic infections like hookworms, schistosomiasis, or whipworms can cause blood loss through the gastrointestinal tract, leading to iron deficiency anemia. Other parasites, such as Plasmodium (malaria), may cause anemia due to red blood cell destruction, which can further complicate iron levels.
- Helicobacter pylori (H. pylori) is the organism that leads to ulcers, and it infects the stomach lining. This is a well-documented link to developing iron deficiency anemia.
Rebuilding Iron Levels: Food and Supplements
Fixing an iron deficiency takes a multi-pronged approach. It’s not just about popping a pill, though supplements are often necessary. I recommend iron-supportive supplements for people who just slide into the “normal” range if you have symptoms.
That’s because borderline iron deficiency is so common, and most people drink coffee or take calcium supplements, so their levels are possibly low, and overlooked.
Start with Food
Your body absorbs heme iron from animal sources much more efficiently than non-heme iron from plants. To boost your intake:
- Heme Iron Sources: Eat a steak! If you don’t like red meat, eat poultry, or fish because they are also excellent options but not as rich in iron as a steak.
- Non-Heme Iron Sources: Beans, spinach, and fortified cereals can help, but always pair them with vitamin C to improve absorption. A spinach salad with orange slices or lentil soup with a squeeze of lemon is fine if you are vegetarian.
Cooking in a cast-iron skillet can also add a small amount of dietary iron to your meals.
Iron Supplements: Choosing and Using Them Wisely
For many people, food alone isn’t enough to relieve iron deficeincy anemia, especially if levels are severely depleted. Supplements can be a game-changer, but they come with some rules. Follow the directions on the product that you buy. Be sure to follow the dosage instructions on the label and avoid exceeding the recommended amount. All iron supplements can harmlessly darken the color of your stool.
-
- Choosing Iron Supplements:
- Ferrous Bisglycinate: Relatively gentle on the stomach and highly absorbable.
- Heme-Based Iron: Found in products like Proferrin, ideal if you tolerate animal-based supplements.
- Ferrous Sulfate: My least favorite type of iron due to stomach discomfort, and poor absorption, but it’s widely sold and used in studies.
- Iron Polypeptide: This is a highly absorbable iron supplement derived from heme iron, designed to treat or prevent iron deficiency anemia. It is gentle on the stomach and less likely to cause side effects like nausea or constipation compared to traditional iron supplements.

- Miscellaneous Supplements that Support IDA
- Lactoferrin: This is not iron, it’s a natural protein that improves the absorption and reduces inflammation, especially helpful in inflammatory conditions like celiac disease. It impacts hormones so some people may experience breast pain.
- Betaine: Keep this supplement in your back pocket – it isn’t for everyone. Adequate stomach acid is critical for digesting food and absorbing nutrients, including iron, calcium, magnesium, and vitamin B12. Betaine HCl supplements taken with meals may improve digestion and absorption of minerals, however, this supplement is not recommended for GERD sufferers due to the risk of worsening symptoms.
- Vitamin C: Enhances the absorption of non-heme iron (the type found in plant-based foods).
- B vitamins: Specifically B12 and folate are essential for red blood cell production and overall anemia management.
- Vitamin D: Studies suggest that low vitamin D levels are common in individuals with anemia, and correcting this deficiency may improve overall outcomes, including red blood cell health.
- Choosing Iron Supplements:
The Rules of Iron Supplementation
-
- Take iron on an empty stomach with vitamin C to maximize absorption.
- Avoid taking iron supplements with dairy, calcium supplements, or coffee, as these block iron uptake.
-
I mentioned this earlier, but follow the directions on the supplement label, not what you see on Google. Iron can be constipating, and also, it can darken the color of your stool – don’t be alarmed. If you need a stool softener for the constipation that iron supplements cause, use something like Colace® or Surfak®. Drink plenty of water.
Feeling better is a great sign, but don’t stop there. Retest your ferritin and iron panel every few months to ensure your levels are climbing. It’s common to feel improvements in energy and focus within a few weeks of starting supplementation, but true recovery takes time.
If oral iron doesn’t work or symptoms persist, intravenous (IV) iron therapy may be necessary, especially for those with severe deficiencies or absorption issues but this does come with some side effects. You can read more HERE about the signs and symptoms of iron deficiency anemmia.
How Do You Know if You’re Taking (or Have) Too Much Iron?
Taking too much iron can lead to iron overload, which may cause harmful effects in the body. Monitoring iron levels through specific lab tests and recognizing symptoms is essential if you’re supplementing iron regularly. Read this: You Can Order Your Own Blood Work and Lab Tests: Here are 6 Advantages!
Symptoms of iron overload include nausea, vomiting, diarrhea, or abdominal pain. You may also experience some degree of paradoxical fatigue (despite taking iron), and joint pain because iron deposits in the joints. If the condition persists for a long time, you may end up with liver dysfunction (jaundice or abdominal swelling), grayish or bronze-toned skin, and heart problems (ie palpitations or chest pain, heart failure etc). If iron continues to build up, you have iron toxicity in the pancreas or pituitary gland.
To summarize this briefly, I’d say that if you’re experiencing unexplained fatigue, joint pain and/or persistent abdominal discomfort, or symptoms that worsen despite supplementation, it may not be something you need. For that matter, people with hemochromatosis never need iron becuase they ahve a genetic predisposition to having excessive amounts! But you can be sure of iron overload by taking some lab tests.
Key Lab Tests:
- Ferritin: Measures iron stores. High levels (>300 ng/mL in women) suggest iron overload.
- Transferrin Saturation (TSAT): Shows how much transferrin is carrying iron. Levels >45–50% indicate overload.
Beyond Iron: The Bigger Picture
Low iron often doesn’t occur in isolation. It can affect and be affected by other systems in your body. For example:
- Thyroid Function: Your thyroid needs iron to produce hormones, and low thyroid function can mimic anemia symptoms. Read this article next, 5 Reasons for Low Iron and How It Relates to Thyroid Disease.
- Gut Health: Conditions like SIBO or leaky gut can interfere with iron absorption and should be addressed alongside treatment.
- Medications: Taking acid blockers for reflux or heartburn interferes with iron levels. I can’t emphasize this enough. If you take any kind of antacid, or heartburn reliever like a PPI (omeprazole) or an H2 antagonist (famotidine), or anything similar to these, it can cause iron deficiency anemia.
- B12 and Folate: These nutrients are also critical for red blood cell production and may need supplementation if deficient.
Final Thoughts
Iron deficiency anemia is more than a lab value – it’s a debilitating condition that will zap your energy and quality of life. The good news is that with the right approach, you can rebuild your levels and feel like yourself again. Start with thorough testing, tackle absorption barriers, and support your body with a combination of food and supplements.
Whether you’re a clinician helping patients navigate their iron journey or someone struggling with low levels, remember: iron isn’t just a nutrient, it’s your lifeline to energy, vitality, and optimal health. Stay consistent, track your progress, and give your body the time it needs to heal.

Suzy Cohen, has been a licensed pharmacist for over 30 years and believes the best approach to chronic illness is a combination of natural medicine and conventional. She founded her own dietary supplement company specializing in custom-formulas, some of which have patents. With a special focus on functional medicine, thyroid health and drug nutrient depletion, Suzy is the author of several related books including Thyroid Healthy, Drug Muggers, Diabetes Without Drugs, and a nationally syndicated column.